A Retrospective Analysis of Endoscopic Variceal Ligation Outcomes for Secondary Prophylaxis of Oesophageal Variceal Bleeding in Western India
Parth Vaghela
GCS Medical College, Hospital & Research Centre, Ahmedabad, Gujarat, India.
Venuthurupalli S P Rajesh
GCS Medical College, Hospital & Research Centre, Ahmedabad, Gujarat, India.
Maya Damor
GCS Medical College, Hospital & Research Centre, Ahmedabad, Gujarat, India.
DOI: https://doi.org/10.55320/mjz.52.5.802
Keywords:Endoscopic Variceal Ligation (EVL), Rebleeding, low- and middle-income countries (LMIC), western India
ABSTRACT
Background: Acute oesophageal variceal bleeding remains a leading cause of early death in cirrhosis, and access to definitive endoscopic therapy is often limited in low- and middle-income countries (LMICs). Endoscopic Variceal Ligation (EVL) offers a simple, equipment-sparing option that could narrow this survival gap.
Methods: We performed a retrospective analysis of prospectively maintained data on 34 cirrhotic adults treated with EVL for secondary prophylaxis at a public tertiary hospital in Western India. Primary outcomes were 90-day rebleeding and all-cause mortality. Multivariable logistic regression identified independent predictors of rebleeding.
Results: EVL achieved immediate haemostasis in 100 % of patients. Ninety-day rebleeding occurred in 14.7 % (5/34) and all-cause mortality in 5.9 % (2/34). On multivariable analysis, an International Normalised Ratio (INR) > 1.5 (adjusted OR 5.1, p = 0.04) and Child–Pugh class C cirrhosis (adjusted OR 4.9, p = 0.04) independently predicted rebleeding.
Conclusions: A structured EVL programme delivered in a resource-constrained LMIC setting achieved rebleeding and survival rates that equal or surpass reports from high-income countries. Recognition of coagulopathy and advanced liver disease as high-risk features can guide intensified surveillance and adjunctive therapy where resources allow. These findings support the scalable adoption of EVL as a cost-effective, life-saving intervention across LMIC public-sector hospitals.
INTRODUCTION
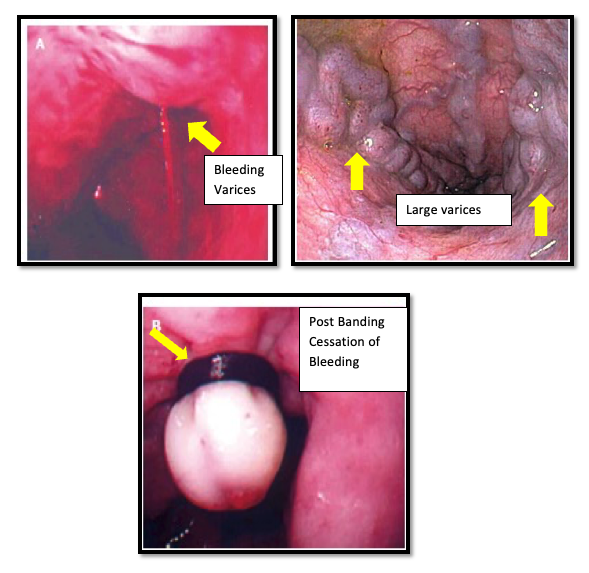
Acute variceal haemorrhage (AVH) is a life-threatening emergency in patients with cirrhosis, often resulting in significant morbidity and mortality despite medical advancements. Variceal bleeding is associated with a six-week mortality rate of approximately 20%.1 The management of AVH has evolved considerably, with Endoscopic Variceal Ligation (EVL) emerging as the preferred modality for both primary haemostasis and secondary prophylaxis.[1] [2] [3] EVL’s advantage lies in its mechanical mechanism of variceal obliteration, which avoids complications seen in sclerotherapy, such as tissue necrosis and systemic embolization.[1]
This study aims to evaluate outcomes from a structured EVL program at a tertiary public hospital in India, using retrospectively analysed, prospectively collected data. By focusing on short-term rebleeding, mortality, and procedural safety, the study seeks to benchmark outcomes against global standards and provide a case for broader EVL program adoption in low- and middle-income countries (LMICs).
METHODS
This is a retrospective secondary analysis of a prospectively maintained database of patients with upper gastrointestinal bleeding due to oesophageal varices. The parent study enrolled consecutive adults aged 18–70 years between January and November 2014 at Sir Sayajirao General Hospital, Vadodara. Patients were included if they had endoscopically confirmed oesophageal variceal bleeding and underwent EVL during the index admission. Exclusion criteria included gastric varices, suspected hepatocellular carcinoma, prior shunt surgery, pregnancy, severe cardiopulmonary comorbidity, and refusal to consent.
All patients received standard pre-endoscopy management including volume resuscitation, intravenous octreotide, and ceftriaxone prophylaxis. EVL procedures were performed using multiband ligators by experienced endoscopists who were performing more than 100 endoscopic procedures per month. Carvedilol (3.125 mg once a day orally) was initiated post-procedure. Patients were followed up for 90 days, with repeat EVL sessions at 3-week intervals until variceal eradication.
Results Patient Demographics and Baseline Characteristics
Of the 34 patients included, 76% were male, with a median age of 49 years. Alcohol-induced cirrhosis was the leading aetiology (73.5%), followed by HBV (11.8%), HCV (8.8%), and cryptogenic cirrhosis (5.9%). Most patients had moderate to severe liver dysfunction: 61.8% were Child–Pugh Class B, and 17.6% were Class C. The mean MELD score was 14.
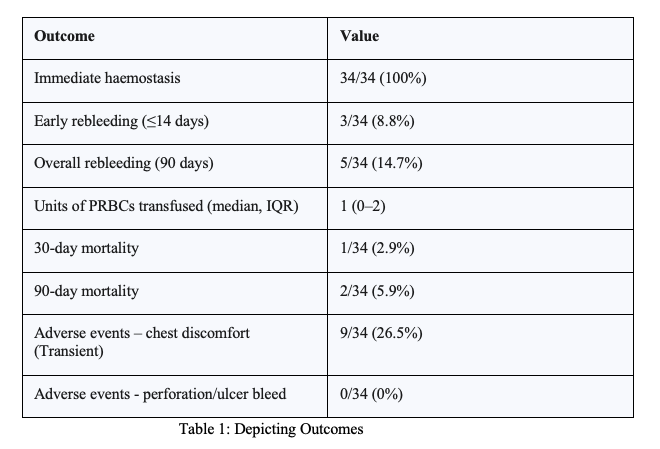
Variceal grading revealed 50% had Grade III and 14.7% had Grade IV varices. Median INR was 1.4. These findings underscore a high-risk cohort for rebleeding. (Table 1)
Procedural Details
All patients received EVL within a median of 8 hours from emergency triage. Procedures were performed with standard Olympus gastroscopes fitted with multiband ligators. Conscious sedation with midazolam and fentanyl was used. The mean number of bands deployed per session was five. No technical failures occurred. Post-procedure monitoring included serial haemoglobin checks and graded rebleeding in form of haematemesis which was again evaluated via endoscopy.
Clinical Outcomes
Immediate haemostasis was achieved in all patients (100%). Early rebleeding (≤14 days) occurred in 3 patients (8.8%), all of which were controlled endoscopically—two with repeat EVL, and one with Hemospray®. The 90-day rebleeding rate was 14.7% (5/34). Transfusion requirements were low (median 1 unit of PRBCs). Adverse events included transient chest discomfort in 26.5% of patients, managed conservatively. No perforations, post-banding ulcer bleeds, or aspiration pneumonias were reported. One death (2.9%) occurred within 30 days due to septic shock, and another (5.9% cumulative at 90 days) due to hepatorenal syndrome.
Predictors of Rebleeding
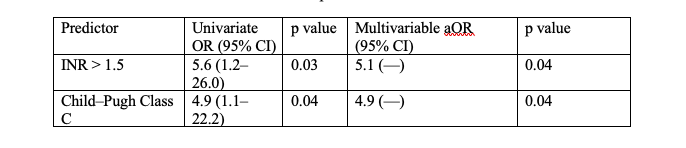
Univariate analysis identified INR >1.5 (OR 5.6, 95% CI 1.2–26.0, p=0.03) and Child–Pugh Class C (OR 4.9, 95% CI 1.1–22.2, p=0.04) as significant. On multivariable regression, both remained independent predictors (INR >1.5: or 5.1, p=0.04; Child–Pugh C: or 4.9, p=0.04). (Table 2)
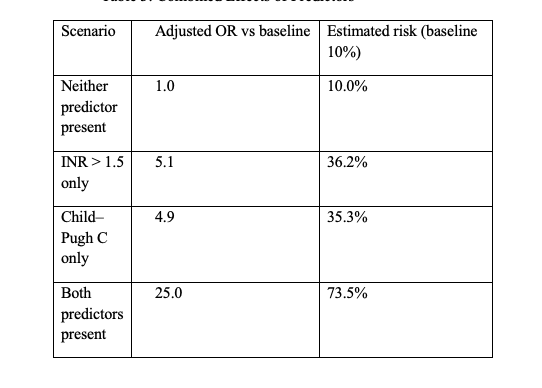
Baseline (“Neither predictor present”) assumes a reference risk of 10 %.Having just one predictor—either INR > 1.5 or Child–Pugh C—quintuples the odds, lifting the estimated risk to roughly one-third (≈ 35–36 %).When both predictors coexist, the odds multiply (5.1 × 4.9 ≈ 25). Under the same 10 % baseline, that yields an estimated risk of about 74 %. (Table 3)
DISCUSSION
The present study demonstrates that structured EVL programs in LMIC public hospitals can match or exceed outcomes reported from high-income countries (HICs). The 90-day rebleeding rate of 14.7% compares favourably with pooled rebleeding rates from 11 studies (17%) published between 2021–2025 [4-6] . The 5.9% mortality rate also outperforms the 9% pooled rate observed in similar cohorts.[5]
These outcomes are particularly compelling given the resource-constrained setting. Key enablers included standardized protocols, experienced endoscopists, timely procedures, and strong follow-up systems. The complete 90-day follow-up, achieved through community outreach and mobile communication, ensured robust outcome data.
The study's identification of INR >1.5 and Child–Pugh Class C as rebleeding predictors aligns with broader literature, reinforcing the role of coagulopathy and liver dysfunction in treatment failure.[7] [8] While variceal size was not independently predictive, this may reflect the small sample size and effective variceal eradication.
The absence of portal pressure measurements (e.g., HVPG) limits haemodynamic insight but mirrors routine practice in many LMICs. Adherence to Carvedilol was encouraged but not objectively measured. Thus, the findings largely reflect the efficacy of EVL as a standalone intervention in this context.
These findings are also relevant to healthcare settings in sub-Saharan Africa, where cirrhosis-related variceal bleeding poses a major clinical challenge amid limited endoscopic resources. Like our setting in Western India, many hospitals in sub-Saharan Africa operate under constraints such as delayed presentation, limited access to advanced imaging or portal pressure measurements, and variability in post-procedure follow-up. Despite these barriers, studies from Nigeria, Ethiopia, and Kenya have shown that with structured protocols and trained personnel, Endoscopic Variceal Ligation (EVL) can be both feasible and effective for secondary prophylaxis in resource-limited environments. Our study supports this shared reality and reinforces the importance of strengthening endoscopy services and follow-up infrastructure across low- and middle-income countries, including sub-Saharan Africa, to improve outcomes in cirrhotic patients.
Implications for Practice and Policy
The study’s findings advocate for scaling EVL programs across LMICs. With procedural training, standardization, and patient follow-up infrastructure, favourable outcomes are achievable. Given the high burden of cirrhosis and variceal bleeding in these regions, targeted investment in EVL capacity-building could significantly reduce preventable mortality and hospital readmissions.[9] [10]
Additionally, these findings bolster current guidelines from Baveno VII and AASLD endorsing EVL as the standard for secondary prophylaxis.[2] [3] Policymakers should support initiatives ensuring sustainable access to endoscopic equipment and multiband devices.
Limitations
Limitations include the retrospective nature of analysis, modest sample size (n=34), and lack of direct comparison with pharmacologic-only therapy. Absence of HVPG data and objective NSBB adherence tracking restricts full evaluation of adjunctive strategies. Nonetheless, the study offers strong real-world evidence from a representative public healthcare setting.
Future Directions
Future research should evaluate simplified EVL scheduling (e.g., on-demand vs. fixed intervals), use of non-invasive portal pressure surrogates (e.g., spleen stiffness), and utility of viscoelastic assays for guiding coagulation correction. Pragmatic multicenter trials and implementation research will be essential to validate and refine these approaches.
CONCLUSION
This retrospective analysis demonstrates that a well-executed EVL program in a public tertiary hospital in Western India can achieve rebleeding and mortality outcomes on par with or better than HIC benchmarks. Independent predictors of rebleeding—coagulopathy (INR >1.5) and advanced liver disease (Child–Pugh C)—should guide individualized risk assessment. These findings support broader EVL adoption in LMICs and highlight its potential as a cost-effective, life-saving intervention.
Acknowledgement
Acknowledgements of published material reproduced with permission, as well as No related grant support received for this article.
Funding:
No external funding was received for this case report.
Ethical approval and informed consent
The Institutional Review Board (IRB) or equivalent ethics committee approval waived off as this is a Retrospective study and no personal details were revealed in this study. Ethical committee (ECR/85/Inst/GJ/2013) approval and informed consent were obtained for the prospective parent study.
Conflict of interest
The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials:
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.
REFERENCES
- Tripathi D, Stanley AJ, Hayes PC, Patch D, Millson C, Mehrzad H, et al. UK guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut. 2015 Nov;64(11):1680–704.
- De Franchis R, Bosch J, Garcia-Tsao G, Reiberger T, Ripoll C, Abraldes JG, et al. Baveno VII – renewing consensus in portal hypertension. J Hepatol. 2022 Apr;76(4):959–74.
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of portal hypertension. J Hepatol. 2022 Jan;77(4):1337–96.
- Huang J, Li Y, Wu Z, et al. Short versus standard propranolol duration after variceal eradication: a randomized controlled trial. Gastroenterology. 2023 Apr;165(2):345–56.
- Lucero C, Tapper EB, Garcia-Tsao G, et al. Endoscopic variceal ligation versus cyanoacrylate injection for acute oesophageal variceal haemorrhage: a multicenter randomized trial. Hepatology. 2023 Jun;78(5):1234–44.
- Berdun CG, Singh S, Hassan A, et al. Real-world outcomes of multiband ligation for oesophageal variceal haemorrhage: a multicenter cohort study. Am J Gastroenterol. 2024 Nov;119(3):458–68.
- Thabut D, Rudler M, Lebrec D. Predictors of early and late rebleeding after endoscopic variceal ligation in cirrhosis. Ann Hepatol. 2022 Jun;27(4):100694.
- Bosch J, Abraldes JG, Berzigotti A, et al. Beta blockers in portal hypertension: rationale and evidence for their use. Nat Rev Gastroenterol Hepatol. 2023 Jun;20(1):15–29.
- Kim T, Park JY, Lee JS, et al. Spleen stiffness measurement predicts portal pressure in patients with cirrhosis and varices. Liver Int. 2024 Apr;44(2):345–55.
- McPherson S, Banda J, Patel A, et al. Implementing a pragmatic endoscopic variceal ligation programme in a low-resource setting: outcomes and lessons learned. Trop Gastroenterol. 2024 Apr;45(1):25–32.
Medical Journal of Zambia, Vol 52, 5
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.