Preoperative hypertension: prevalence and quality of control before elective surgical procedures in North-Central Nigeria
Dr Olufemi Ige
University of Ilorin and University of Ilorin Teaching Hospita
Dr Joshua Oni
University of Ilorin and University of Ilorin Teaching Hospita
Dr Lookman Lawal
University of Ilorin and University of Ilorin Teaching Hospita
DOI: https://doi.org/10.55320/mjz.52.1.630
Keywords:Essential hypertension, Preoperative care, Surgical procedures, Elective surgery, Quality of care
ABSTRACT
Background: patients with perioperative hypertension are frequently encountered and have increased rates of complications like myocardial infarction, renal dysfunction and congestive heart failure. This study was to determine the prevalence and quality of control of perioperative hypertension in elective surgical patients.
Methods: This was a prospective, descriptive cross-sectional study of adult patients scheduled for elective surgical operations. On the day before surgery, the patients were visited on the hospital ward where a questionnaire was administered to obtain demographic data, presence of comorbid diseases, cardiovascular risk factors and compliance with pharmacologic and non-pharmacologic treatment measures.
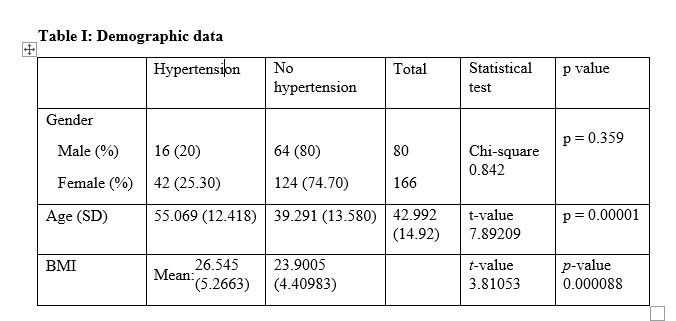
Results: Two hundred and forty-six patients were enrolled in the study. The mean age of the participants was 42.99 (14.92) years. Fifty-eight (23.58%) patients presented with hypertension while 188 (76.42%) did not. The patients with hypertension had a significantly higher mean age (p = 0.00001) and mean BMI (0.000088) than those without hypertension. Twenty-four (41.38%) had blood pressure in the Stage 1 range (140–159/ 90–99 mm Hg) and nine (15.52%) had blood pressure in the Stage 2 range (160–179/ 100–109 mm Hg). No patient had a blood pressure above 180/110mmHg. Three surgeries were postponed; they were all in hypertensive patients consisting 5.17% of all hypertensive patients.
Conclusion: We conclude that the prevalence of hypertension makes it an important peri-operative comorbidity in our environment. Blood pressure control was poor while surgical case postponements were more likely in the hypertensive than in the non-hypertensive subjects.
INTRODUCTION
Hypertension has become a major public health challenge in sub-Saharan Africa in the last few decades as the increase in prevalence rates across low- and middle-income countries has surpassed those of high-income countries.[1] It is defined as a systolic blood pressure (BP) equal to or greater than 140 mmHg or a diastolic blood pressure equal to or greater than 90 mmHg. In Nigeria, the prevalence of hypertension is 28.9%.[2] Despite this high prevalence rate, overall awareness of elevated blood pressure remains low at 17.4%.[2] The challenges to management of hypertension in the region are inadequate financing for non-communicable diseases, frequent medication stock-outs, limited health insurance coverage, and a limited workforce capacity for hypertension management.[3]
During pre-anaesthesia evaluation, elevated blood pressure is the most common perioperative comorbidity encountered in non-cardiac surgical patients, with a rate of 51.8% during pre-anaesthesia review.[4] When adequately controlled, hypertensive patients can have an uneventful perioperative course. However, patients with uncontrolled perioperative hypertension have increased rates of case cancellations[5] and complications like myocardial infarction[6] and renal dysfunction.[7] Perioperative hypertension can also result in complications like excessive surgical bleeding, congestive heart failure (CHF), and acute pulmonary oedema (APE). They also exhibit exaggerated hypotension after induction of anaesthesia and excessive pressor response to stresses such as laryngoscopy and intubation, surgical incision, and extubation. While the control of blood pressure is desirable before elective surgery, it may bring additional challenges such as altered cerebral autoregulation in a patient who has adapted to elevated blood pressures, which may compromise cerebral blood flow.[8]
The prevalence of hypertension is expected to rise with time due to an increase in sedentary lifestyle, obesity, and the aging population.[9] This expected rise in prevalence of preoperative hypertension and the impact of uncontrolled perioperative hypertension has re-emphasized the importance of the control of hypertension before surgery. The prevalence of this group of patients has not been adequately studied in the north-central region of Nigeria. This study was to determine the prevalence and quality of control of perioperative hypertension in elective surgical patients.
METHODS
Study design: This was a prospective, descriptive cross-sectional study of adult patients scheduled for elective surgical operations at the University of Ilorin Teaching Hospital.
Setting: The study was carried out at the University of Ilorin Teaching Hospital, Ilorin, Nigeria. This hospital is a multispecialty facility located in the north-central region of Nigeria that serves as a referral centre for patients from Kwara State and neighbouring states of Kogi, Niger, Ekiti, and Oyo. An average of one thousand six hundred elective operations is carried out in the hospital annually.
Inclusion criteria: Consenting consecutive adult patients scheduled for elective surgical procedures were recruited for the study from July 2022 till the completion of the study.
Exclusion criteria: Included patients' refusal to participate in the study, age less than 18 years, American Society of Anaesthesiologists (ASA) class > II, and inability to understand due to language barriers.
Ethical approval: Approval for the study was obtained from the Ethics and Research Committee of the University of Ilorin Teaching Hospital, Ilorin, Nigeria, before the commencement of the study. Verbal and written informed consent, signed and dated, was obtained from all participants after the investigator provided them with a detailed explanation of the study. Data was stored in password-protected devices with access limited to authorized personnel only. Data will only be used for research purposes and will not be disclosed without the consent of participants.
Sample size determination: The sample size was calculated using Fisher’s formula.[10] In a previous study, the prevalence of hypertension in the nation was estimated to be 28.9%.[2] Therefore, the total number of participants required for this study was 245.
Preoperative AssessmentOn the day before surgery, the patients were visited on the hospital ward where a questionnaire was administered to the patient by a senior registrar in the Department of Anaesthesia who was specifically trained to administer the questionnaire. The questionnaires were verbally administered in person at the patients’ bedside. The patients were given the option of not answering any question they were not comfortable with, and they were permitted to withdraw from the interview at any time if they so wished. Information on the patients’ demographic data and presence of comorbid diseases were acquired with the questionnaire. Participants were also asked if they had been previously diagnosed as hypertensive, if they were prescribed any medication for hypertension, and whether they complied with any prescription. The blood pressure was measured with a mercury sphygmomanometer from the right arm on three occasions, ten minutes apart, with the patient in the supine position. The senior registrar measuring the blood pressure was seated with his eyes parallel to the sphygmomanometer to prevent errors due to parallax. The sphygmomanometer was placed on the bed beside the patient. After pre-anaesthesia evaluation, patients who had their surgical procedures postponed to allow better control of blood pressure elevation were noted.
Data AnalysisResults generated from this study were expressed as frequencies or proportions of total, means, and standard deviations. Tests of significance were analyzed with Student’s t-test for means and Chi-square test for categorical variables using the computer software package SPSS version 19.0. A p-value of less than 0.05 was considered statistically significant.
RESULTS
Two hundred and forty-six patients were enrolled in the study; there were more females, 166 (67.48%), than males, 80 (32.52%). The mean age of the participants was 42.99 years with a standard deviation of 14.92 (Table 1). The males had a slightly higher mean age of 44.63 years (S.D 17.15) than the females, 42.21 years (S.D 13.69). The recruited patients were scheduled for various surgical procedures in diverse specialties. There were 69 gynaecological, 62 general surgical, 43 orthopaedic, 26 urologic, 13 neurosurgical, nine from ENT and plastic surgery, and 16 from other specialties.
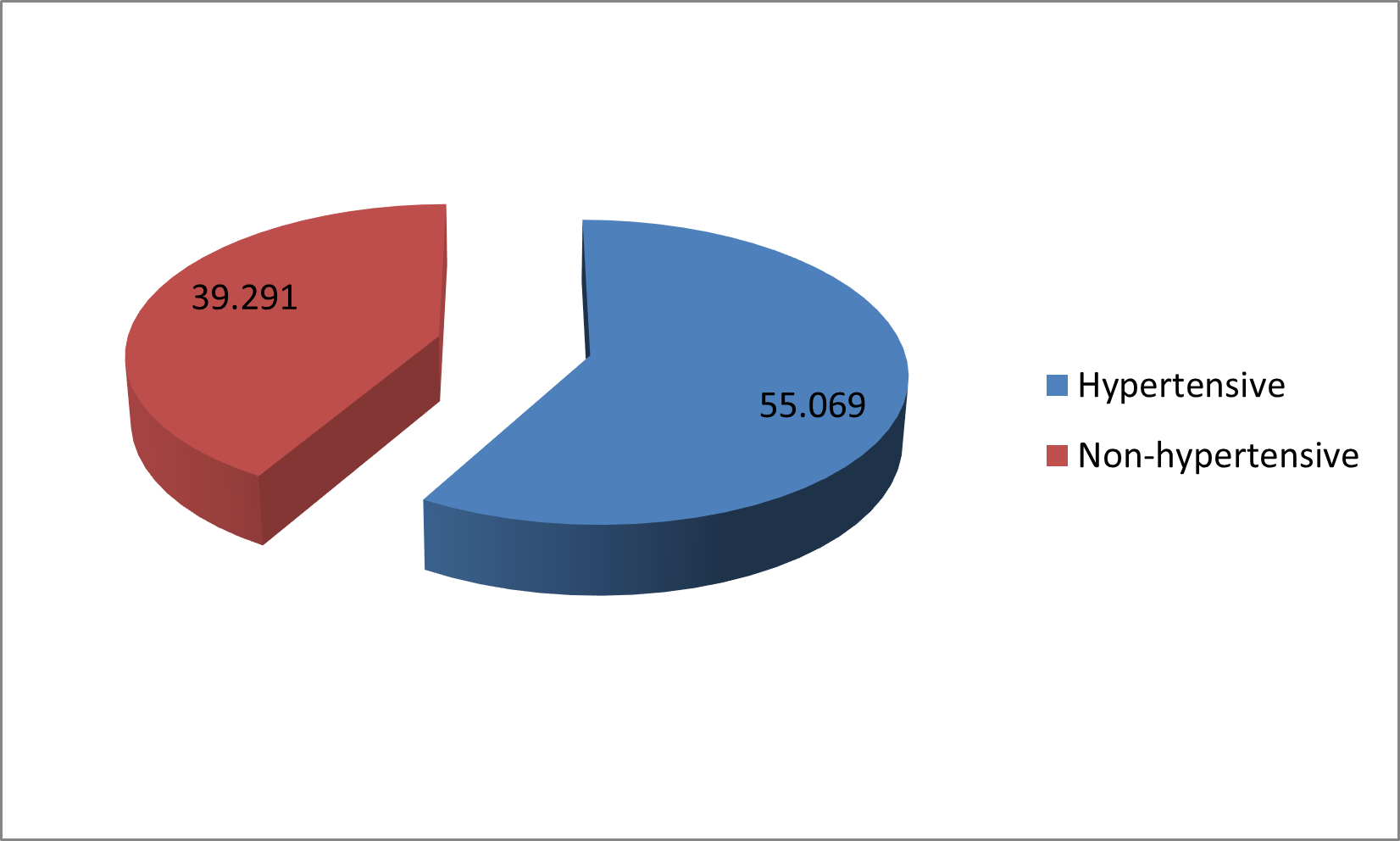
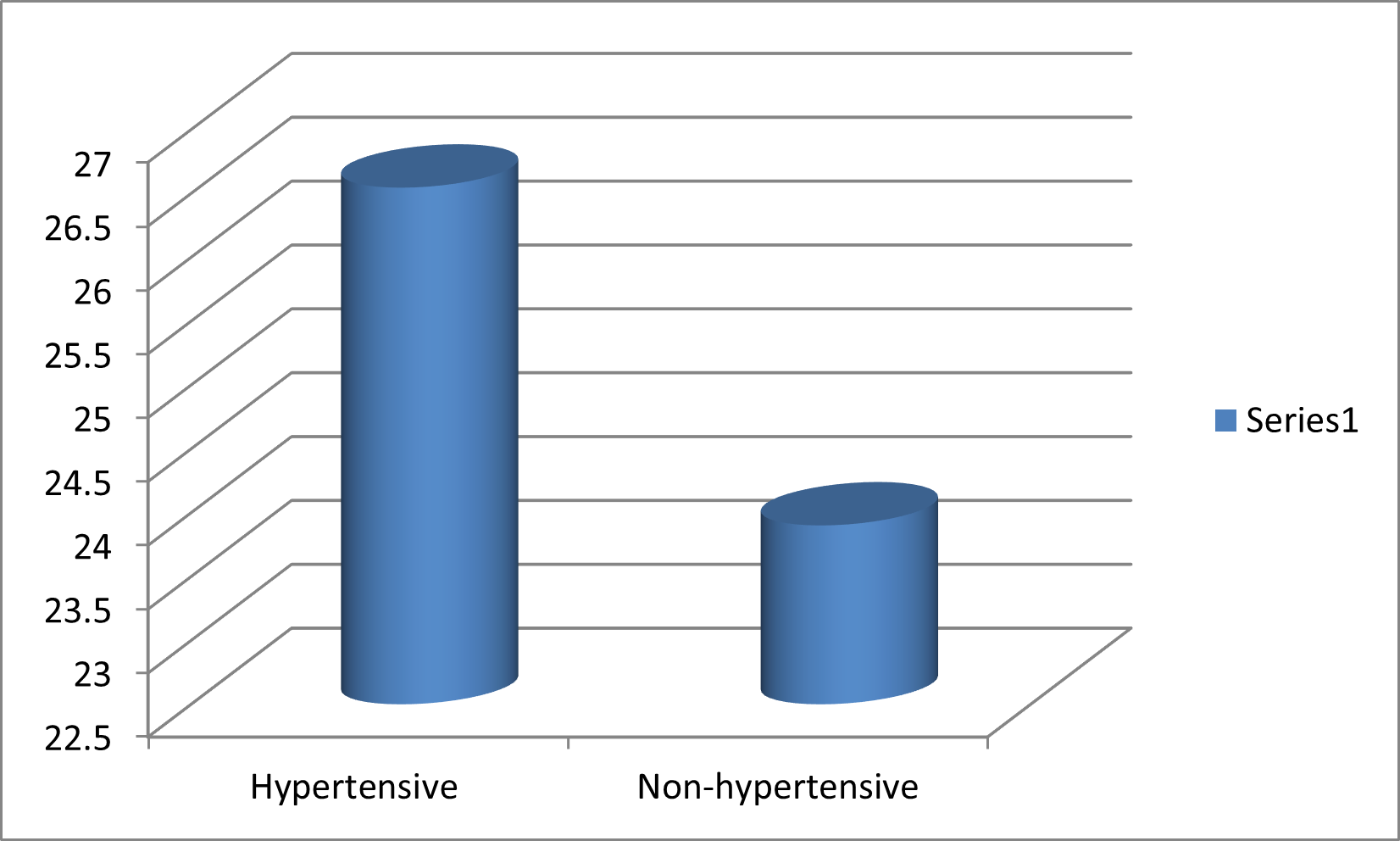
Presence of Hypertensive DiseaseFifty-eight (23.58%, 95% confidence interval 0.1828 – 0.2888) patients presented with hypertension, while 188 (76.42%, 95% confidence interval 0.7112 – 0.8172) did not. Of the 58 patients with hypertension, 39 (67.24%, 95% confidence interval 0.5516 – 0.7932) had no other medical disease, while 19 (32.76%, 95% confidence interval 0.2068, 0.4484) had other medical diseases. Sixteen males were hypertensive, which is 20% of the 80 males in the study population, while 42 (25.30%) females of the 166 in the population had hypertension. The gender difference was not statistically significant (p = 0.359). The patients with hypertension had a significantly higher mean age (p = 0.00001) (fig 1) and mean BMI (p = 0.000088) (fig 2) than those without hypertension. There were ten (17.24%) new diagnoses of hypertension, with 48 (82.76%) previously diagnosed patients. Of the 58 patients with hypertension, 50 (86.21%) were currently on medication, while eight (13.79%) were not. Only 25 (43.10%, 95% confidence interval 0.3036 – 0.55841) of those with hypertension had a normal blood pressure during preoperative assessment; 33 (56.90%, 95% confidence interval 0.4416 – 0.6964) had elevated blood pressure. Twenty-four (41.38%, 95% confidence interval 0.1944 – 0.4332) had blood pressure in the Stage 1 range (140–159/90–99 mm Hg), and nine (15.52%, 95% confidence interval 0.0620 – 0.2484) had blood pressure in the Stage 2 range (160–179/100–109 mm Hg). No patient had a blood pressure above 180/110 mmHg.
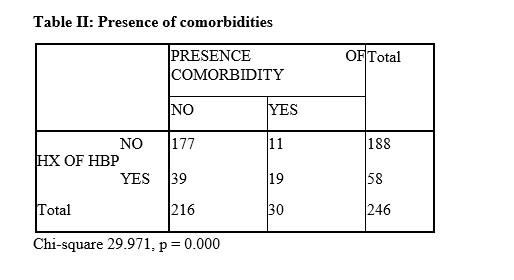
Presence of Other ComorbiditiesOf the 58 patients with hypertension, 19 (32.8%) also had other comorbidities. When compared to the 188 patients without hypertension, 11 (5.8%) had comorbidities. The difference was statistically significant (p = 0.000).
Case PostponementThree surgeries were postponed; they were all in hypertensive patients, consisting of 5.17% of all hypertensive patients (95% confidence intervals -0.0053 – 0.10871). Those with normal blood pressures did not have any surgeries postponed.
DISCUSSION
The study population had 246 surgical patients out of which 58 (23.58%) either had a previous diagnosis of hypertension or had a measured blood pressure of 140/90mmHg or higher. Hypertension presents additional risks to surgical patients during anaesthesia. Stiffening of the arterial vasculature and a depleted intravascular volume which may both occur because of chronic hypertension may result in hypotension during induction of anaesthesia.[11] During laryngoscopy and intubation, hypertensive patients may demonstrate greater exaggeration of the pressor response than normotensive patients.[12] They may also have exaggerated responses to anaesthetic agents and surgical stimulus leading to fluctuations in blood pressures[13] and are more likely to have perioperative myocardial infarction.[6] When the elevation in blood pressure is controlled preoperatively, morbidity is reduced. However, hypotension is more dangerous than hypertension therefore overly aggressive blood pressure control should be discouraged.
Identifying patients at risk preoperatively is important as it would allow for appropriate treatment of hypertension and risk reduction. Hypertensive patients scheduled for elective surgical procedures are usually prescribed oral antihypertensive medication to control blood pressure. While this is expected to reduce the risk associated with anaesthesia and surgery, the impact of these medications on the intraoperative course and their interaction with anaesthesia medication must be taken into consideration. Hypertensive agents such as angiotensin converting enzyme inhibitors[14] and angiotensin receptor blockers[15] are associated with intraoperative haemodynamic instability which may require the administration of fluids and vasopressors for control. Failure to control perioperative hypertension can result in complications like myocardial infarction[6] and renal dysfunction[7] in the intraoperative or postoperative period.
The prevalence rate of preoperative hypertension of 23.58% in this study is slightly lower than the prevalence rate of hypertension in the Nigerian general population of 28.9%[2] (but within the range of 2.1-47.2% for crude prevalence rate of hypertension in adult Nigerians.[16] However, it is much lower than the rate of 51.8% reported in South Africa[4] and higher than 6.9% reported from southern Ethiopia.[17] This may be because the average age of participants in the South-African study was higher at 50years compared to 43years in our study.
Our study did not find a statistically significant difference in gender distribution though, in Nigeria, hypertension has been found to be more common in males.[2] Our study had a higher proportion of females presenting for surgery. This may have masked the impact of gender in the hypertensive patients.
The study also found that hypertensive patients were of older age and had a higher BMI than those without hypertension. Age-related changes leading to stiffness of arterial walls has been implicated as a factor in the increasing prevalence of hypertension in the elderly. Another study found that 71% of patients with preoperative hypertension had an elevated BMI.[18] Hypertension in the obese may be due to activation of the sympathetic nervous system (SNS), increase in the amount of intra-abdominal and intra-vascular fat, sodium retention and activation of the renin-angiotensin system.[19]
The pre-anaesthesia evaluation is not only an avenue for the anaesthetist to establish a rapport with the patient and assess the effectiveness of control of comorbid medical diseases but also an opportunity to diagnose previously undetected diseases. Ten (17.24%) of the hypertensive patients in this study were diagnosed during the current admission. The rate of newly diagnosed hypertension among patients presenting for elective surgery in South Africa is 9.9%.[4] Surgical or anaesthesia evaluation may be the only opportunity patients in a developing country get to check their blood pressure as access to healthcare may be limited. A thorough evaluation of the surgical patient is therefore vital for the detection of comorbid medical diseases that can negatively impact the conduct of anaesthesia or outcome of surgery.
Nineteen (32.8%) of the hypertensive patients had other comorbidities. This was statistically higher than the 11 (5.8%) non-hypertensives with comorbidities (p 0.000). Pre-anaesthesia evaluation is useful in the detection of previously undetected comorbid disease.[20] Therefore, it would be prudent to search for the presence of other medical diseases through history, physical examination and relevant laboratory investigations in all hypertensives scheduled for surgery.
Only 25 (43.10%) of the hypertensive patients had a normal blood pressure before surgery, 56.9% of the hypertensive patients had blood pressures in the stage 1 or 2 ranges. Thus, more than half of the patients had poorly controlled blood pressure. A previous study also found inadequately controlled blood pressure in 36.9%[4] of preoperative hypertensive patients. This poor control in some preoperative hypertensive patients should not be taken lightly as stages 1 and 2 hypertensive patients were at 34.7% moderate, 33.3% high and 16.7% very high risk for a cardiovascular event in the following 10 years.[18] Therefore, when these patients present for surgery, additional care has to be taken to monitor for adverse perioperative events and manage them. The poor blood pressure control we found in our study was even though 50 (86.21%) were on hypertensive medication when they presented for surgery. Anaesthetists must consider the appropriateness of the choice, dosage and compliance with therapeutic regimen when evaluating hypertensive patients in the preoperative period as change of medication or dose adjustments may be required.
Our study found that surgical case postponements were more likely among hypertensive patients than non-hypertensives. This is most likely due to the poorly controlled blood pressure in about 56% of our patients. Poorly controlled hypertensives are exposed to greater risks perioperatively such as a higher incidence of myocardial ischaemia[21], myocardial infarction[6] and renal dysfunction.[7] Despite these risks, the cancellation of surgical procedures in patients with elevated blood pressure must not be arbitrary. Blood pressure measurements in our study were within the stage 1 or 2 ranges. While the anaesthetist should be wary of the complications that may occur in a patient with stage 1 or 2 hypertension, cancellation or postponement of these procedures would be inappropriate as possible complications can be prevented or effectively managed. In a study with predominately stage 1 and 2 hypertensive patients; no association was found between the stage of pre-operative hypertension and peri-operative haemodynamic changes that could cause major morbidity and mortality.
Perioperative administration of beta-blockers in hypertensive patients undergoing non-cardiac surgeries reduced 30-day and one year mortality while withdrawal of these medications resulted in an increase in mortality.[22] The availability of intravenous antihypertensives such as sodium nitroprusside and nitroglycerin have made it possible to effectively manage intraoperative blood pressure elevations. Perioperative risk seems to be more pronounced in patients with stages 3 and 4 hypertension and case cancellation is not recommended with a blood pressure of 180/110 mmHg or below[23] while other authors suggest that a diastolic pressure below 110 mmHg is safe. Compared to hypertension, intraoperative hypotension had a stronger association with myocardial injury, acute kidney injury, and death.[24] It should be considered more problematic than intraoperative blood pressure elevations.
LIMITATIONSInvasive measurement of intraoperative blood pressure is more accurate and may have detected a larger statistical difference. However, this monitoring modality was not indicated as part of the anaesthetic management of these patients, therefore it was not employed; non-invasive methods were used in all participants. The exclusion of ASA class III and higher could have created a bias in the sample population. The authors were trying to avoid a possible cofounding effect from the increased severity of the surgical pathology. Also a reliance on the recall of the patients during questioning about medication compliance may be fraught with bias as they may be prone to answer in the affirmative.
CONCLUSION
Based on our findings, we conclude that the prevalence of hypertension makes it an important peri-operative comorbidity in our environment. Surgical patients with preoperative hypertension are more likely to be of older age, higher BMI and to have other comorbidities than other patients. Surgical case postponements were also found to be more likely in the hypertensive than in the non-hypertensive subjects. Public health interventions to improve hypertension awareness among the general population are likely to be beneficial in improving the diagnosis of hypertension and patients’ compliance with prescribed medication. Perioperative protocols designed to optimize the perioperative management of the hypertensive surgical patient are also likely to improve perioperative care.
RECOMMENDATIONS
We advocate for more public engagements by relevant stakeholders to improve awareness relating to identification and management of hypertension among potential surgical patients in the population.
We also recommend the establishment and strengthening of pre-anaesthesia evaluation clinics, which may help to facilitate early identification and better control of blood pressure peri-operatively.
Additionally, a multidisciplinary approach that encourages early referral of hypertensive patients to cardiologist will prevent unnecessary surgical case cancellations.
ACKNOWLEDGEMENTS
The authors appreciate the contribution of the resident doctors in the Department of Anaesthesia during data collection for this study.
Competing interest
The authors declare that they have no competing interests.
Funding
The authors did not obtain any funds for the conduct of this study.
Author’s contributions
All authors contributed to the conception and design; acquisition, analysis and interpretation of data; drafting and revising the article and final approval of the version to be published.
REFERENCES
- Ferdinand KC. Uncontrolled hypertension in sub‐Saharan Africa: Now is the time to address a looming crisis. Journal of Clinical Hypertension (Greenwich). 2020; 22(11): 2111–2113. doi: 10.1111/jch.14046.
- Adeloye D, Basquill C, Aderemi A.V, Thompson JY, Obi FA. An estimate of the prevalence of hypertension in Nigeria: a systematic review and meta-analysis. Journal of Hypertension. 2015;33(2):230-42. doi: 10.1097/HJH.0000000000000413.
- Orji IA, Baldridge AS, Omitiran K, Guo M, Ajisegiri WS, Ojo TM, et al. Capacity and site readiness for hypertension control program implementation in the Federal Capital Territory of Nigeria: a cross-sectional study. BMC Health Serv Res. 2021;21(1):322. doi: 10.1186/s12913-021-06320-8.
- van der Spuy K, Crowther M, Nejthardt M, Roodt F, Davids J, Roos J, et al. A multicentre, cross-sectional study investigating the prevalence of hypertensive disease in patients presenting for elective surgery in the Western Cape Province, South Africa. South African Medical Journal. 2018;108(7):590-595. doi: 10.7196/SAMJ.2018.v108i7.13022.
- Soni S, Shah S, Chaggar R, Saini R, James E, Elliot J, et al. Surgical cancellation rates due to peri-operative hypertension: implementation of multidisciplinary guidelines across primary and secondary care. Anaesthesia. 2020;75(10):1314-1320. doi: 10.1111/anae.15084.
- Wilcox T, Smilowitz NR, Xia Y, Beckman JA, Berger JS. Cardiovascular Risk Factors and Perioperative Myocardial Infarction After Non-Cardiac Surgery. Canadian Journal of Cardiology. 2021; 37(2): 224–231. doi: 10.1016/j.cjca.2020.04.034.
- Aronson S, Fontes M, Miao Y, Mangano DT, Investigators of the Multicentre Study of Perioperative Ischaemia Research Group and Ischaemia Research and Education Foundation. Risk index for perioperative renal dysfunction/failure: critical dependence on pulse pressure hypertension. Circulation. 2007;115:733–42. doi: 10.1161/CIRCULATIONAHA.106.623538.
- Anaesthesia for Patients with Cardiovascular Disease. In: Butterworth JF, Mackey DC, Wasnick JD. Morgan and Mikhail’s Clinical Anaesthesiology. 5th ed. New York: McGraw-Hill; 2013.
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217-23. doi: 10.1016/S0140-6736(05)17741-1.
- Fisher AA, Laing JE, Stoeckel JE, Townsend JW. Handbook for Family Planning Operations and Research. 1991. New York, Population Council. doi: 10.31899/RH10.1039.
- Miller RD, Pardo M. Basics of Anaesthesia. Philadelphia, Pa: Elsevier Health Sciences; 2011.
- Dabu-Bondoc S, Shelly KH. Management of comorbidities in ambulatory anaesthesia: a review. Ambulatory Anaesthesia. 2015;2:39–51. doi: 10.2147/AA.S64924.
- Kovac AL. Controlling the hemodynamic response to laryngoscopy and endotracheal intubation. Journal of Clinical Anaesthesia. 1996 Feb;8(1):63-79. doi: 10.1016/0952-8180(95)00147-6.
- Behnia R, Molteni A, Igic R. Angiotensin converting enzyme inhibitors: mechanism of action and implications in anaesthesia practice. Current Pharmacological Design. 2003;9(9):763-776. doi: 10.2174/1381612033455413.
- Nabbi R, Woehick HJ, Riess ML. Refractory hypotension during general anaesthesia despite preoperative discontinuation of an angiotensin receptor blocker. F1000Res. 2013;2:12. doi: 10.12688/f1000research.2-12.v1.
- Akinlua JT, Meakin R, Umar AM, Freemantle N. Current Prevalence Pattern of Hypertension in Nigeria: A Systematic Review. PLoS One. 2015; 10(10): e0140021. doi: 10.1371/journal.pone.0140021.
- Mengistu K, Geleta D. Prevalence of preoperative hypertension and its intraoperative anesthetic management among patients undergoing elective surgery at Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia. International Journal of Medicine and Medical Sciences. 2019;11(2):11-19. doi: 10.5897/IJMMS2018.1390.
- Govender S, Pfister C, Rayner B, Dyer RA, Flint M, Roodt F, et al. A multicentre cross-sectional descriptive study evaluating the cardiovascular risk profile of preoperatively identified patients with hypertension. South African Medical Journal. 2020;111(1):74-79. doi: 10.7196/SAMJ.2020.v111i1.14640.
- Jiang SZ, Lu W, Zong XF, Ruan HY, Liu Y. Obesity and hypertension. Exp Ther Med. 2016 Oct; 12(4): 2395–2399. doi: 10.3892/etm.2016.3667.
- Haq ZA, Murthy P, Malik I, Lahori VU, Chaudhary S, Ahuja S. Detection of comorbid illnesses during pre-anaesthesia evaluation in a university teaching hospital: A prospective observational study. The National Medical Journal of India. 2014;27(5):256-8. PMID: 26037424.
- Venkatesan S, Myles P, Manning H et al. Cohort study of perioperative blood pressure and risk of 30-day mortality after elective non-cardiac surgery. British Journal of Anaesthesia. 2017;119:65-77. doi: 10.1093/bja/aex056.
- Wallace AW, Au S, Cason BA. Association of the pattern of use of perioperative blockade and postoperative mortality. Anaesthesiology. 2010;113:794-805. doi: 10.1097/ALN.0b013e3181f1c061.
- James MFM, Dyer RA, Rayner BL. A modern look at hypertension and anaesthesia. Southern African Journal of Anaesthesia and Analgesia. 2011:17(2), 168-173. doi: 10.1080/22201173.2011.10872770.
- Sessler DI, Bloomstone JA, Aronson S, Berry C, Gan TJ, Kellum JA, et al. Perioperative Quality Initiative consensus statement on intraoperative blood pressure, risk and outcomes for elective surgery. British Journal of Anaesthesia. 2019;122:563-574. doi: 10.1016/j.bja.2019.01.013.
Medical Journal of Zambia, Vol 52, 1
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.