Sudden Infant Death Syndrome an infantile death-bed misadventure
K Saasa
Principal General Practitioner, Emeritus
MSS Patel
Consultant Pathologist, Emeritus
Sanana Phillips
Primary Care Practitioner, Optum Serve, Arizona USA
DOI: https://doi.org/10.55320/mjz.52.1.627
Keywords:Sudden Infant Death Syndrome, cot-death, safe-sleeping position, maternal bed-sharing, suffocation, maternal overlaying
ABSTRACT
A case of Sudden Infant Death Syndrome, aka cot-death is reported. The significance of Sudden Infant Death Syndrome in Zambia is highlighted. The objective is to shine the spotlight on a preventable cause of death in Africa, and the research work and public health campaigns to reduce infant mortality. Sudden Infant Death Syndrome has been defined as an unexpected death of an infant under twelve months old whilst asleep and which remains unexplained after reviewing the clinical history, performing an adequate thanatopsy investigation and examining the scene of death. The aetiopathogenesis is yet to be determined and the cause of death remains elusive. The clinical features are non-specific, and typically an asymptomatic healthy baby is found dead whilst asleep. The diagnosis is reached by excluding any other cause of death. This may pose a diagnostic challenge when there is a concomitant disease which might be a coincidental finding but not the cause of death.
In the case reported, a thanatopsy examination followed up by ancillary investigations assisted in determining the cause of death. A suspicion of suffocation by maternal overlaying may not be substantiated without distinguishing signs of trauma. A concealed infanticide may be overlooked and misdiagnosed as a cot-death. There is no legal definition of a cause of death, and it is at best an informed clinical opinion, not a medical fact. It is important to be accurate and interpret the subtle findings carefully. It may be ethically wise to err on the side of caution and not risk a miscarriage of justice. Since Sudden Infant Death Syndrome is due to a natural cause for registration purpose, there were no judicial proceedings. The bereaved family were consoled and the essentials of the cause of death were sensitively explained to bring about a satisfactory outcome.
There has been an assortment of hypothetical causes of Sudden Infant Death Syndrome ranging from the sublime to the ridiculous, published in the medical literature but lacking any conclusive evidence. The outstanding risk factors have been identified as prone sleeping position and sharing maternal bed. The public health campaigns in the Western world have reinforced the supine safe-sleeping position for infants and significantly lessened the incidence of infant deaths. The research studies on the incidence and prevalence, and risk factors of Sudden Infant Death Syndrome in Africa have been minimal. They are a prerequisite for the development and implementation of a standardized thanatopsy protocol for investigating deaths in infancy. An international thanatopsy guideline has been developed but its non-African orientation may overwhelm under-resourced African nations. A public health campaign in Africa has to compete with the challenges of cultural rituals and traditions of infant sleeping position and maternal bed-sharing, perpetuated by community elders. Recommendations are made for the provision of accurate data for research work and development of a health awareness programme to reduce the risk factors of Sudden Infant
INTRODUCTION
Sudden Infant Death Syndrome (SIDS) must have existed from time immemorial. There is a possible cot-death in the background of the biblical judgement of King Solomon (1 Kings 3: verses 16-28). It is unlikely that there would have been a thanatopsy investigation to ascertain whether the infant could have been smothered by overlaying in a shared maternal bed. SIDS can be potentially misdiagnosed as concealed infanticide, and it may be ethically wise to err on the side of caution and not risk a miscarriage of justice.[1]
SIDS has been defined as an unexpected death of an infant under twelve months old whilst asleep and which remains unexplained after i) reviewing the clinical history; ii) performing an adequate thanatopsy investigation; iii) examining the scene of death. It is listed under Symptoms, Signs and Ill-Defined Conditions in the WHO International Classification of Disease.
The pathophysiological causation of SIDS is yet to be determined ever since it was characterised over five decades ago. There is no pathognomonic pathology and a careful and accurate interpretation of the subtle findings in SIDS is paramount. There is no legal definition of a cause of death, and it is at best an informed clinical opinion; not a medical fact.[1] There tends to be an overestimation of the prevalence of SIDS when thanatopsy investigations are inadequate for ascertaining the cause of death. The International Standardized Protocol jointly developed by SIDS International and National Institute of Child Health and Development group (United States) has made a thanatopsy examination more consistent. It is intended to improve diagnostic accuracy of SIDS and enhance the data available to researchers. The inconsistency in the management of infant deaths in Africa and the consequential less reliable epidemiological data specifically impact on diagnostic challenges in SIDS.
There has been an assortment of hypothetical causes of SIDS published in the medical literature but lacking conclusive evidence. The current knowledge of risk factors of SIDS, known as the Triple Risk Model, consists of i) critical infant developmental immaturity or a genetic basis; ii) environmental factors, such as prone sleeping position and maternal bed-sharing; iii) intrinsic factors, such as impaired cardiopulmonary arousal. The theoretical consensus on the outstanding risk factors is the sharing of maternal bed and prone sleeping position which affects a chemotactic respiratory response to hypoxia / hypercapnia. It has been likened to Ondine's Curse (Congenital Hypoventilation Syndrome) which compels mortals to stay awake to breathe.
There have been very few studies on the incidence and prevalence and the risk factors of SIDS in sub-Saharan Africa, and the subject is under reported in the medical literature.[2] In a Zambian study which asked mothers about best practice, the majority chose maternal bed-sharing and opted for the baby to sleep sideways but most mothers were willing to adopt a supine sleeping position.[3] A sizeable minority had never been advised on the safe-sleeping position by a child health-care service provider in Zambia.[3]
In socio-economically advanced countries, SIDS is a leading cause of infant mortality. It is well recognised as a major preventable cause of infant deaths in the Western world in contrast to the less-known burden of SIDS in Africa.[4] It has been on the decline over the last two decades, due to successful public health campaigns targeting the outstanding risk factors identified as infants sleeping in the prone position and sharing the maternal bed.[5] The prophylactic rewards are unpredictable and a cohort of infants with be prone to SIDS. It is important for mothers to know that reducing the risk factors will not completely prevent babies from SIDS. A public health campaign in Zambia may have to compete with the challenges of African cultural rituals and traditions of infant sleeping position and sharing maternal bed, perpetuated by community elders.[6][7]
In the Western world, mothers usually carry babies in a variety of infant carriers or baby slings, and it is considered to be a safe practice.[8] It has been linked to a risk of suffocation in babies under three months old.[8] There are no reports of a similar risk factor, or overheating in Zambia where mothers traditionally carry babies in a marsupial-pouch wrap on the back, and slide it to the front for breast feeding [Figure 1]. Mothers are advised to keep the baby under constant observation during hands-free breastfeeding, and check that the infant is in a comfortable semi-upright position to avoid the risk of suffocation. It is an ideal piggy-back opportunity for child health-care service providers to promote safeguarding habits for mothers to prevent SIDS.

CASE REPORT
Clinical history:
A healthy three-month-old female baby was bottle fed in the evening as usual and put in her carrycot to sleep on her back. She was found unresponsive early in the morning by her mother who shared the same bedroom. The mother could not recall the sleeping position of the baby when she was discovered moribund. The standard resuscitation attempts by an ambulance crew were unsuccessful. She was taken to the hospital where life was pronounced extinct.
There were no suspicious circumstances. However, the attending doctor had remarked “cot suspended” baby. This was misconstrued as suspension of the infant by the head entrapped in the guard rails of a cot-bed, and it instituted a medico-legal death investigation.
The obstetric and paediatric history was uneventful. She was delivered by Caesarean section at 34 weeks gestation without complications and weighed 3.0Kg. The baby was breast fed for the first 10 weeks. Her developmental milestones were unremarkable. There was no family history of SIDS or any hereditary disease.
There were no prior clinical symptoms or any concerns for the baby. There was no requirement for medical consultancy, intervention or observation.
Thanatopsy investigation:
i) An external examination showed a well-nourished and well cared-for baby dressed in a hospital shroud. She weighed 5.4Kg and her anthropometric indices were C-H 59cm, C-R 42cm and foot length 9cm (below 50th percentile), and head circumference 42cm (90th percentile). There were no facial or conjunctival petechiae.
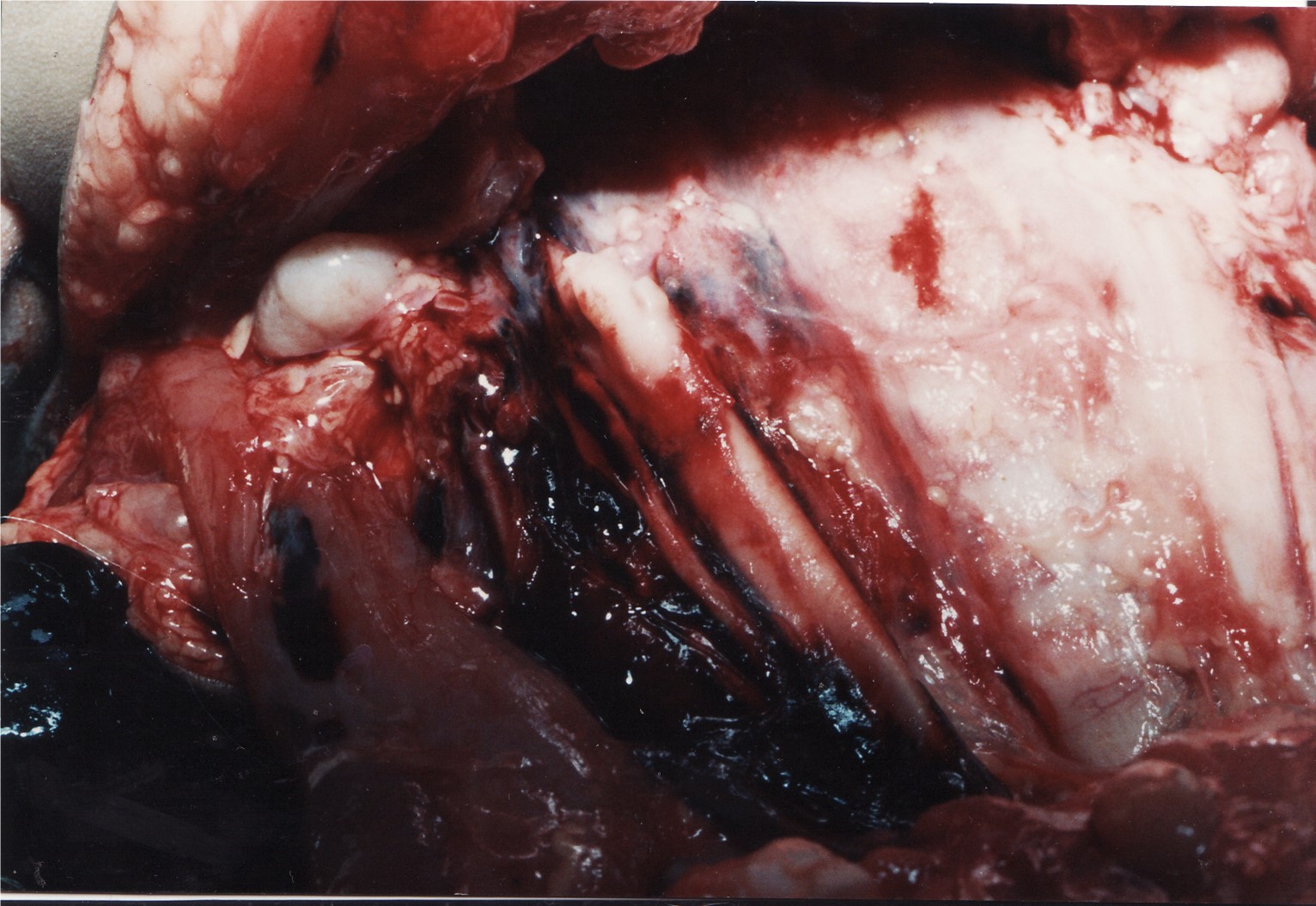
There was a grooved pallid impression partly encircling the neck [Figure 2].

The marks of injuries consisted of a midline small rectangular bruise on the nape and a slightly larger similar bruise at the front of the neck, and a minor abrasion on the left lower eyelid aligned with ipsilateral minor scratch marks on the nose.
There were multiple therapeutic needle puncture marks on the right side of the neck, precordium and hands and feet. The venepuncture marks were created by the ambulance crew during unsuccessful resuscitation attempts.
Xray radiography was unremarkable and showed no fractures.
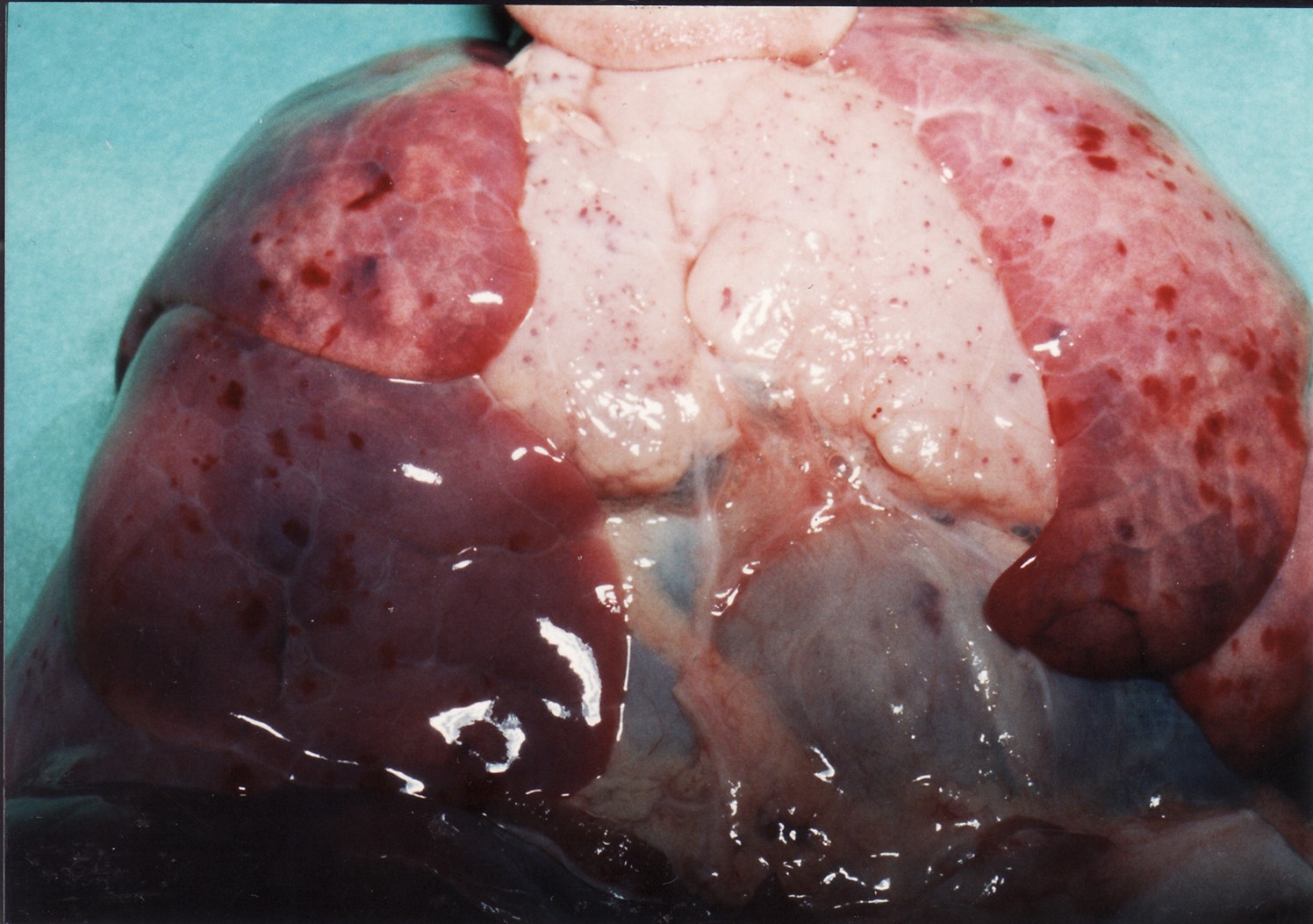
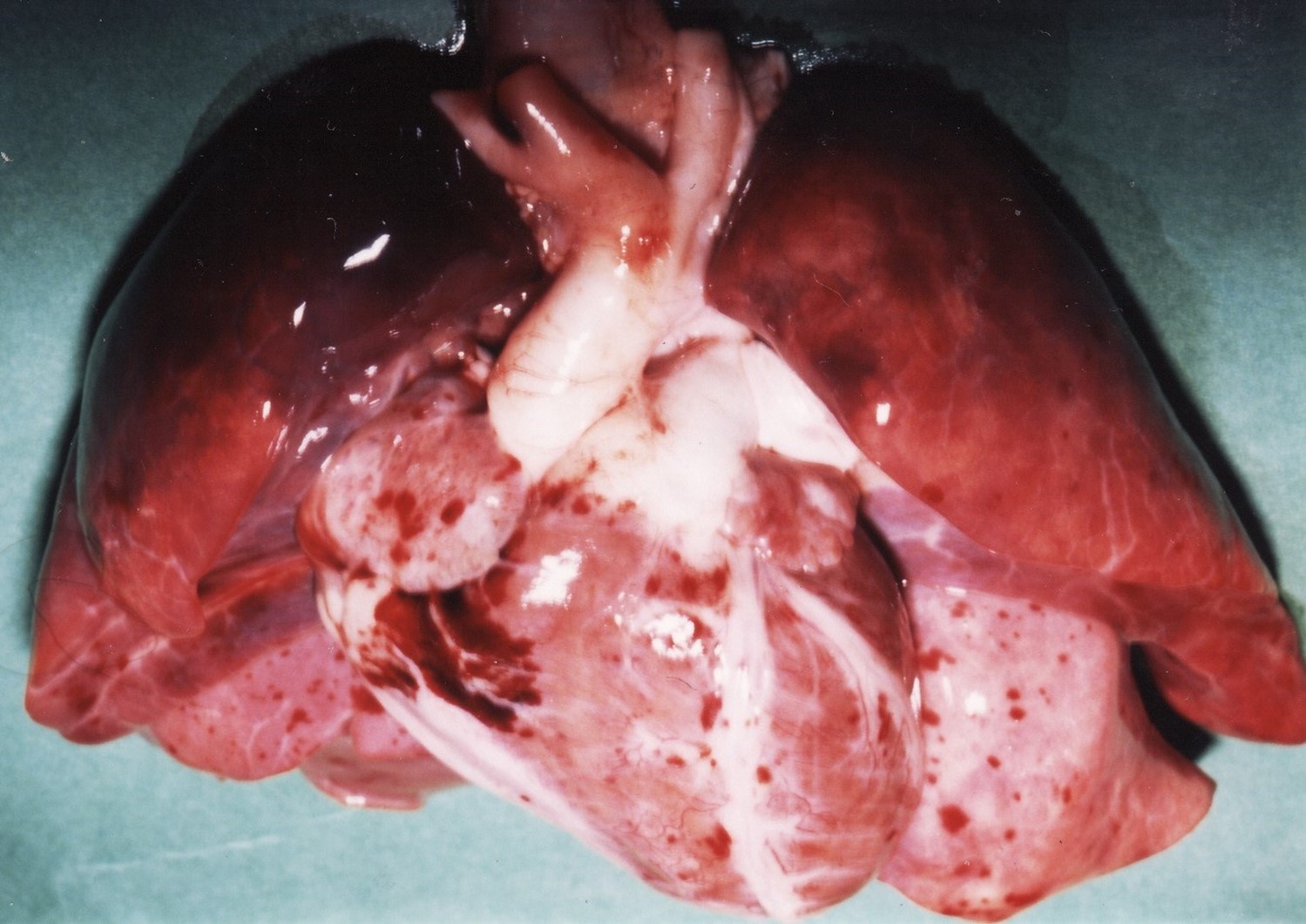
ii) An internal examination showed a large, diffused contusion around the right jugular vein [Figure 3]. A deeper dissection of the soft tissue underneath was unremarkable and showed no injury to the neck structures. The thoracic viscera showed extensive petechial haemorrhages over an enlarged thymus gland and were confluent on the epicardial and pleural surfaces [Figures 4, 5].
iii) The systemic examination showed no abnormality of the brain and there was no evidence of sepsis or haemorrhage. The heart and great blood vessels were of normal appearance and showed no congenital anomaly. The lungs showed oedema and congestion and no evidence of infection. The alimentary, urogenital, endocrine, lymphoreticular and musculoskeletal systems were unremarkable. There was a small amount of semi-fluid milky gastric content.
The weights of the organs were 540g (brain); 26g (heart); 90g (lungs); 122g (liver); 42g (kidneys); 16g (spleen); 11g (thymus).
iv) A preliminary conclusion was that the overall appearance was non-specific and consistent with SIDS. There was no evidence of significant natural or congenital disease, and no sign of maltreatment or non-accidental trauma that could have caused or contributed to death. The iatrogenic injuries were consistent with recent therapeutic resuscitation.
A diagnostic challenge was in differentiating between SIDS and an asphyxial mode of death from compression of the neck. It turned out to be relatively simple to exclude asphyxiation and any other cause of death. It is specifically impacted upon when thanatopsy investigations are inadequate and fall short of the definition of SIDS. There will be sensitivity when the bereaved family perceives an invasive investigation of the dead as socio-culturally inappropriate and have strong moral objections.
v) A scene of death examination, histopathology and microbiology were followed up. A toxicological analysis was kept on hold, and a haematological investigation was deemed not necessary.
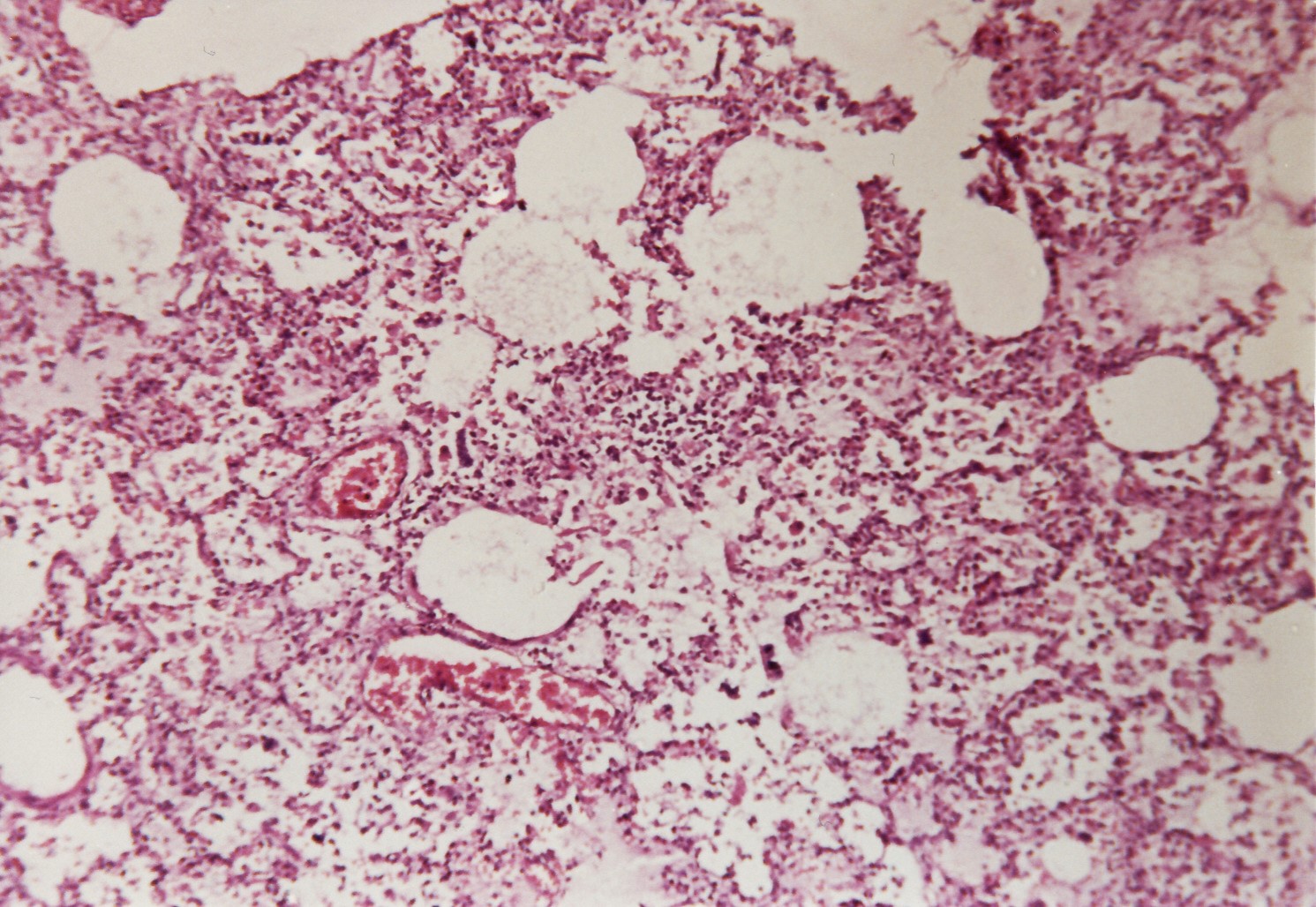
The microscopy examination of the lungs showed foci of chronic inflammatory cells [Figure 6]. The cellular infiltrate imitating a viral infection was a non-specific finding. The lymph nodes and thymus showed non-specific hyperplasia and thymic parenchymal petechial haemorrhages. The rest of the organs were unremarkable.
The microbiological viral screening and bacterial cultures were negative.
The standardized protocol for a Medico-Legal Death Investigation (MLDI) under the National Forensic Act, 2020 (Zambia) provides for an examination of the scene of death for the completion of the definition of SIDS. It complements the recommendation of the Centre for Disease Control (USA), in conjunction with the Zambia National Public Health Institute, to strengthen public health surveillance of non-communicable diseases.
The thanatopsy findings along with ancillary and scene of death investigations were discussed with the Police authority followed by a report for the Coroner. All interested parties were satisfied with SIDS being the cause of death. There was no inquest since SIDS is treated as a natural death for legal purposes.
The bereaved family were consoled and briefed with the essentials of SIDS. The mother declined further family support but consented to an anonymous publication in a medical journal for educational and research purposes.
DISCUSSION
The diagnostic challenges of SIDS due to an elusive cause of death in the absence of an aetiopathogenesis are discussed. The significance of SIDS in Zambia is highlighted. The objectives are to shine the spotlight on a preventable cause of death, and the research work and public health campaigns in Africa to reduce the burden of infant mortality.
SIDS was originally defined in the late 1960s, and it replaced an outdated diagnosis of cot-death {Anglo-Indian etymon}. It is included under Symptoms, Signs and Ill-Defined Conditions in the WHO International Classification of Disease. The definition has been modified and re-evaluated, and it was upgraded in 2020 by CJ Foundation (United States) to help improve research work.
The current definition of SIDS stands as sudden and unexpected death of an infant under one year old with the apparent fatal episode occurring during sleep, and it remains unexplained after a thorough investigation which includes a thanatopsy examination, and a review of the circumstances of death and the clinical history. Sub-categories have been added, and they include near-miss SIDS when death has been paused by therapeutic intervention. A universal definition of SIDS facilitates consistency and uniformity in the provision of data for research work.[8]
Infant deaths from SIDS are synonymously covered by the terms Sudden Unexpected Infant Death or Sudden Unexplained Infant Death (SUID). Those who are over the age of 12 months are separated from SIDS and designated as Sudden Unexplained Death in Children.
A thanatopsy examination in cases of SIDS has been standardized by the International Standardized Protocol which was jointly developed by SIDS International and National Institute of Child Health and Development group (United States). It should improve diagnostic consistency, accuracy and enhance the statistical data for researchers. Its non-African orientation may prove to be overwhelming for under-resourced nations like Zambia. A standardized protocol for investigating SIDS is paramount in providing reliable data, which are necessary for developing a public health campaign to increase awareness of the risk factors in SIDS. It can be restructured without compromising an acceptable minimum standard if constrained by limited resources in Africa.
The features of SIDS are heterogeneous and non-specific, and the diagnosis is made by exclusion of any other cause of death.[10] A suspicion of suffocation by maternal overlaying may not be differentiated from SIDS without signs of non-accidental trauma. It is important to proactively exclude any indication of the Syndrome of Child Abuse and Neglect or Non-Accidental Trauma.[1] Technically SIDS should be in the category of a semi-suspicious deaths with forensic ramifications. Nonetheless, SIDS is regarded as death due to a natural cause for registration purposes, and in the interest of the welfare of the bereaved family.
From the perspective of the bereaved family in the case reported, there was nothing refractory about the healthcare provision. The mother had an urbane persona and as such there was no socio-cultural conflict. She had complied with safe-sleeping position for the baby and refrained from maternal bed-sharing.
There is no pathognomonic pathology in SIDS and a careful and accurate interpretation of the subtle findings is paramount. A finding of concomitant disease which is coincidental and not the cause of death may pose a diagnostic challenge without ancillary investigations. A microscopy of histology tissue is essential for differentiating causative and coincidental findings.[10] Microscopy in SIDS are usually unremarkable, otherwise the cause of death must be reconsidered.[10]
A frequent non-specific finding in SIDS is petechiae over the thymus, pleurae and epicardium as in the case reported [Figures 4, 5]. Lungs may show chronic inflammatory cells imitating viral pneumonia [Figure 6]. Petechial haemorrhages are not indicative of asphyxia from suffocation, and foci of inflammatory cell infiltrate do not indicate an infection.[9]
The misconstrued clinical history of entrapment of the head in a cot-bed was dispelled after a scene visit. The baby slept in a carrycot which had no hazardous bars or structural defects. The circumferential grooved impression found on the neck is not an uncommon postmortem artefact produced by an uneven hypostatic pressure in the skinfold and not caused by compression of the neck [Figure 2]. The case illustrates the importance of fulfilling the definition of SIDS by reviewing the circumstances of death and examining the scene of death.
There is an assortment of hypothetical causes of SIDS, and various theories ranging from the sublime to the ridiculous have been published in the medical literature. The pathophysiological causation of SIDS remains elusive and various theories lack conclusive evidence. The Triple Risk Model postulates i) a genetic polymorphism; ii) poorly developed autonomic control; iii) cardiopulmonary immaturity causing impairment of the chemotactic arousal response to sleep apnoea or hypoxia / hypercapnia.[5] It has been likened to Ondine's Curse from Greek mythology, which compels mortals to stay awake to breathe.
SIDS is a leading cause of infant mortality in socio-economically advanced countries. It has been on the decline over the last two decades due to the success of health awareness programmes, highlighting the risks of infants sleeping in the prone position and sharing the maternal bed.[5] It has been estimated that the preventive strategy has reduced the incidence of SIDS by 50-90%.[5] The other risk factors are maternal smoking or intoxication, and co-sleeping on soft sofa but maternal room-sharing was beneficial. The prophylactic rewards are unpredictable, leaving a cohort of infants prone to SIDS.
A par excellence public health campaign to reduce the burden of SIDS has been run by UNICEF in association with the Lullaby Trust, originally known as the Foundation for the Study of Infant Deaths. The phenomenal success may be attributed to resourceful dissemination of infographics on the risk factors of SIDS, giving concise advice on safe habits for mothers to adopt while providing emotional support for the bereaved family and funding research work.
SIDS is well recognised as a major preventable cause of infant mortality in the Western world in contrast to the less-known burden of infant deaths in Africa. There have been very few studies on the incidence and prevalence, and the risk factor of SIDS in sub-Saharan Africa such that the subject is under reported in the medical literature.[2] A systematic review of the medical literature was undertaken to assess the prevalence of SIDS and the risk factors in Africa.[4] It was largely centred in South Africa where the prevalence of SIDS was 2.5 to 21% compared to 11.3% in Zambia. The risk factors were estimated to be 60 to 91.8% for maternal bed-sharing and 26.7 to 63.8% for prone sleeping position. A high rate of SIDS is estimated to be between 0.2 and 3.7 per 1000 live births in Africa.[4] The distribution pattern was not homogeneous, and it limited a generalisation of the burden of SIDS in Africa.
The health awareness programmes targeting outstanding risk factors, i.e. unsafe prone sleeping position and maternal bed-sharing have been significantly successful in the Western world. The poorly recognised significance of SIDS in Africa is blamed on the lack of resources for the investigation and introduction of public health campaigns to reduce the burden of SIDS.[2] In a Zambian study mothers were asked about best practice and 70.1% opted for the baby to sleep sideways and 60.5% chose maternal bed-sharing.[3] There were 24.1% of the mothers who had never been advised on the supine sleep position by a child health-care service provider but 65.5% were willing to adopt a safe-sleeping position.[3]
A lesson for Zambia, and other African nations in general is to allocate governmental resources for a health awareness programme to reduce the burden of SIDS. An inconsistent management of infant deaths owing to limited resources in Africa has contributed to less satisfactory epidemiological data required for reliable research work. For optimal compliance with a public health campaign, it must have an educational strategy for gen Z {Zoomers} mothers challenged by African cultural rituals and traditions about infant sleeping position and sharing maternal bed.[6] It can be achieved by childcare classes at antenatal clinics since there is near-100% attendance by new generation of mothers, and supplemented by information booklets, pictorial posters and radio and television broadcasts.
In a verbal qualitative analysis of the circumstance of death in infants under 6 months old who were found sleeping in bed, SIDS was classified as SUID if there were no antecedent medical conditions or clinical symptoms.[7] The verbal free-text of the bereaved Zambian mothers identified 7.4% of such cases, of which 90% were deemed consistent with SUID with the majority of infants being under 2 months old.[7] The results supported SUID as an important cause of infant mortality in Zambia. It is acknowledged by researchers in SIDS that a reliance on the so-called verbal autopsy has significant limitations. The methodology of so-called verbal autopsy serves well as a surveillance tool, but the statistical data based on hearsay evidence may not reflect the true incidence of SIDS.
There is overestimation of the prevalence of SIDS when thanatopsy investigations are inadequate for ascertaining a cause of death. A retrospective case audit of medico-legal death investigation (MLDI) in South Africa found that it differed widely within the country.[11] It showed that 8.7% of infant deaths were ascribed as SIDS compared to 14.8% which were determined as unascertainable when satisfactory postmortem and ancillary investigations were performed.[11]
The accuracy of data is prerequisite to a national awareness programme targeting the sleeping position of the infant and maternal bed sharing to reduce the burden of a preventable cause of infant deaths in Zambia.[6][7] It necessitates the development and implementation of a standardized thanatopsy protocol for investigating deaths in infancy, akin to the standardization of MLDI under the National Forensic Act 2022 in Zambia.[1][11]
CONCLUSION
SIDS is well recognised as a major preventable cause of infant deaths in the socio-economically advanced countries in contrast to the less-known burden of SIDS in sub-Saharan Africa. There are very few studies reported in the medical literature on the incidence and prevalence and the risk factors of SIDS in Africa. The researchers in Zambia have relied on hearsay evidence obtained from bereaved mothers via so-called verbal autopsy for the surveillance of risks factors in SIDS. An accurate source of data is more likely to be derived from inclusion of a thanatopsy examination. It is a prerequisite for planning public health campaigns to reduce the burden of SIDS.
It is strongly recommended that all suspected cases of SIDS are subjected to a MLDI, which is likely to provide a more accurate source of data from the thanatopsy examination.[1] The State Forensic Pathologist Office in Zambia should begin the process as soon as practicable. The international thanatopsy guideline for improving diagnostic accuracy and enhancing the statistical data for researchers should be considered. The Zambia Paediatric Association and Zambia Association of Gynaecologists and Obstetricians could jointly establish a taskforce on SIDS in liaison with the Ministry of Health to consider developing and implementing a health awareness programme in Zambia, and worthy of a pan-African model.
A public health campaign to reduce the burden of infant mortality in Zambia is also highly recommended. The publicity on infant sleeping position and sharing the maternal bed should use all media platforms available for communication. It must be disseminated in all the major dialects by means of information booklets, pictorial posters, social media network, radio and television broadcasts, and at fundraising events for optimal compliance. Child health-care service providers could contribute by organising training and holding symposia on current scientific knowledge and the latest research work on SIDS. It may require a socio-political impetus from a Zambian charitable organisation with an agenda to canvass a general awareness of SIDS whilst offering emotional support for the bereaved family, like the Lullaby Trust in our defunct colonial motherland. It is understandable that it may be overwhelming for an under-resourced nation like Zambia.
In the meantime, the child welfare and health service providers must carry on according to trusted experience and current knowledge of infant deaths.
REFERENCES
- Saasa K. and Patel M.S. Battered Baby Syndrome: a good medico-legal denouement. Medical Journal of Zambia. 2024;51:405-14.
- Ndu I.K. Sudden infant death syndrome: an unrecognised killer in developing countries. Pediatric Health, Medicine and Therapeutics. 2016;7:1-4.
- Osei-Poku G.K. Mwanayanda L. et al. Assessing infant sleep practices and other risk factors of SIDS in Lusaka, Zambia: a cross-sectional survey of mothers in Lusaka, Zambia. https://doi.org/10.1186/s12887-022-03712-5
- Osei-Poku G.K. Thomas S. et al. A systematic review of the burden and risk factors of sudden infant death syndrome (SIDS) in Africa. Journal of Global Health. 2021; 11:1-14.
- Moon R.Y. Horne R.S. and Hauck F.R. Sudden infant death syndrome. Lancet. 2007; 370:1578-87.
- Osei-Poku G.K. Mwanayanda L. et al. Qualitative assessment of infant sleep practice and other risks factors of sudden infant death syndrome (SIDS) in Lusaka, Zambia. https://doi.org/10.1186/s12887-023-04051-9
- Osei-Poku G. Mwanayanda L. et al. The apparent burden of unexplained sudden infant deaths in Lusaka, Zambia: Findings from analysis of verbal autopsies. https://doi.org/10.12688/gatesopenres.14303.1
- Bergounioux J. Madre C. et al. Sudden deaths in adult-worn baby carrier: 19 cases. European Journal of Pediatrics. 2015;175:1665-70.
- Byard R. Sudden Infant Death Syndrome: definitions. In: Duncan J.R. and Byard R.W. (editors) SIDS Sudden Infant and Early Childhood Death: The Past, the Present and the Future. Adelaide: University of Adelaide Press, 2018, chapter 1.
- Byard R.W. The Autopsy and Pathology of Sudden Infant Death Syndrome. In: Duncan J.R. and Byard R.W. (editors) SIDS Sudden Infant and Early Childhood Death: The Past, the Present and the Future. Adelaide: University of Adelaide Press, 2018, chapter 24.
- du Toit-Prinsloo L. Dempers J. et al. Toward a standardized investigation protocol in sudden unexpected deaths in infancy in South Africa: a multicenter study of medico-legal investigation procedures and outcomes. Forensic Science, Medicine, and Pathology. 2013;9:344-50.
Medical Journal of Zambia, Vol 52, 1
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.