Determinants of Curative Service Utilization and Therapeutic Pathways in Mbuji-Mayi, DRC
Crispin Tshishimba Kamuandjenda
Faculty of Public Health, Official University of Mbujimayi, Mbujimayi, DR. Congo
Pamela Mbuyi Mushiya
Faculty of Public Health, Official University of Mbujimayi, Mbujimayi, DR. Congo
Felly Kazadi Tshiaba
Faculty of Public Health, UPCC, Mbujimayi, DR. Congo
Chadrack Kabeya Diyoka
School of Public Health, University of Lubumbashi, Lubumbashi, DR. Congo
, Leatitia Ngongo Mwanvua
School of Public Health, University of Lubumbashi, Lubumbashi, DR. Congo
Criss Koba Mjumbe
School of Public Health, University of Lubumbashi, Lubumbashi, DR. Congo
André Mutombo Kabamba Lumanyisha
5Department of Pediatric, Faculty of Medicine, Official University of Mbujimayi, Mbujimayi, DR. Congo
DOI: https://doi.org/10.55320/mjz.52.1.612
Keywords:: Determinants- use, therapeutic itineraries, Mbujimayi.
ABSTRACT
Background The DRC has demonstrated its commitment to progress towards universal health coverage (UHC). The functioning of health facilities in Mbujimayi city is limited by several factors that must be considered if universal health coverage is to be achieved.
Objective The objective of this study is to determine the use of curative services and therapeutic path in Mbuji-Mayi, DRC.
Methods We conducted a cross-sectional study on 05 September 2022 in the city of Mbuji-Mayi. We used stratified probabilistic sampling and the 10 health zones were composed in strata. The minimum sample size was calculated using Epi Info, version 7.2.6.0 (n=409 households, including 10% error margin). Data were analysed in SPSS version 23. A univariate analysis was performed using the Pearson chi-square test, OR (95% CI) and bottom-up logistic regression to examine the association between independent variables and use of curative services.
Results Most cases (67.7%) involved male heads of household (sex ratio = 2.1). The average age was 38.07 ± 16.14 years with a secondary level, heads of households accounted for 47.9%. Overall utilization of curative care services was 45.5%. In our series, as a first resort, 21.03% and 20.05% of heads of household opted for pharmacy and self-medication. The second most common choice being HGR (60.75%), only 32.80% of respondents reported using Health Centre. Most heads of households (33%) paid for care in full, and 65.8% said that it was expensive. Regression analysis identified factors that are associated with the use of curative services, after adjustment. The profession, the perception of the cost of care, the economic level of the household and the distance health education-home were associated with the use of curative services.
Conclusion This study underscores the need for targeted interventions to improve healthcare utilization in Mbuji-Mayi, including the regulation of informal health sectors, financial support mechanisms, and improved accessibility through UHC initiatives.
INTRODUCTION
The concept of universal healthcare coverage is currently being promoted on a global scale with the objective of guaranteeing that all individuals have access to the healthcare services they require without this resulting in financial difficulties for users.[1] In 2008, the World Health Organization (WHO) published two significant reports: the Global Report on Primary Health Care Renewal [2] and the Global Report on Health Financing.[3] The two reports enabled the WHO to draw lessons from the past and establish a pathway to universal health coverage (UHC) by implementing reforms and strategies that can be adapted to the specific conditions of each nation.
The Democratic Republic of Congo (DRC) has signalled its commitment to advancing along this trajectory by implementing the 2016-2020 and 2019-2022 health development plans.[4] This determination assumed particular significance in 2020, with the formulation of a strategic plan for universal health coverage in the DRC. The provision of essential, high-quality health services to communities is a crucial element of UHC, the status of which is currently unsatisfactory on a global scale.
Over the past two decades, there has been a notable decline in the accessibility of health services, as evidenced by numerous instances across the globe.[5] Globally, over 400 million individuals lack access to fundamental healthcare services. In numerous countries, many people receive care that is frequently inadequate or of poor quality. Consequently, the healthcare system fails to meet expectations, with healthcare services often deemed unsatisfactory.[5] The criteria for utilising healthcare services reflect the performance of the healthcare system, but they are shaped by various factors, both intrinsic and extrinsic to the system.
Research conducted in numerous countries on the treatment pathway has revealed a multitude of variations and complexities in the utilisation of healthcare services, particularly within urban contexts. The variety of care use observed includes instances of patients not seeking care, self-medication, the use of traditional medicine, prayer rooms and the utilisation of contemporary health services. The latter may be conventional primary healthcare services, private for-profit or not-for-profit services, or hospital services.[6][7][8][9][10]
The studies published in the DRC illustrate unconventional care pathways that call into question the conventional structure of health services.[6][10][11] In Kasai Oriental, the available field data indicate that access to curative services has remained relatively low over the past three years, with estimated figures of 40% for 2019, 43% for 2020 and 41% for 2021.[12] Mbujimayi, the capital of Kasai province, is a landlocked town characterised by a proliferation of private health establishments, a high unemployment rate and a system of decentralisation that has not been respected. The operation of health facilities in the town is constrained by several factors that must be addressed if universal health is to be achieved. Objective 'Three' of the 17 Sustainable Development Goals chosen by the DRC by 2030 is to provide better overall management of the health needs expressed or felt by the community.
An examination of the utilisation of curative services and the patient treatment pathway, which encompasses the progression of medical interventions throughout the course of treatment, can facilitate the identification of organisational inconsistencies that exist within urban health services. The objective of this study is to determine the utilisation of curative services and the therapeutic itinerary in Mbuji-Mayi, DRC.
MATERIALS AND METHODS
We conducted a cross-sectional study over a period of one and a half months, from July 20 to September 5, 2022, in 10 Health Zones in the city of Mbuji-Mayi. The city of Mbujimayi is located in the Province of Kasai Oriental and has 10 Health Zones.

The study population consisted of households in all 10 Health Zones. We proceeded using the stratified probability sampling technique and all 10 Health Zones constituted strata. Based on a 95% confidence interval, a power of 90%, an expected odds ratio (OR) of 2, an unexposed report on presentations of 1, a proportion of 41% use of curative services in Mbuji-Mayi for the year 2021, the minimum sample size calculated with Epi Info, version 7.2.6.0. The calculated sample size was determined to be 371.68 households, with a margin of error set at 10%. The sample size was revised to 409 households.
We included in this study, heads of households or their representatives over the age of 18 who have been living in the city of Mbuji-Mayi for more than 6 months and who have consented to participate freely in the survey. Excluded from this study were heads of households or their representatives over the age of 18 who resided in the selected health zone for more than 6 months and who did not consent to the investigation.
The collected data was entered into Excel and subsequently transferred to SPSS version 23 for analysis. The mean was employed to present the results in the form of frequency tables, and univariate analysis was conducted by applying Pearson's chi-square test, the odds ratio (OR) and their 95% confidence intervals to investigate the association between the independent variables and the dependent variable (use of curative services). Variables with a significance level of less than 0.10 in the univariate analysis were included in a multivariate model using ascending logistic regression, a mathematical model that allowed us to describe the use of curative services as a function of several explanatory variables (X1, ..., Xn). Statistical significance was set at p < 0.05.
The research protocol was submitted to the Ethics Committee of the Official University of Mbujimayi for approval before its execution.
RESULTS
Sociodemographic and economic characteristics of households that have used curative services and their therapeutic pathway
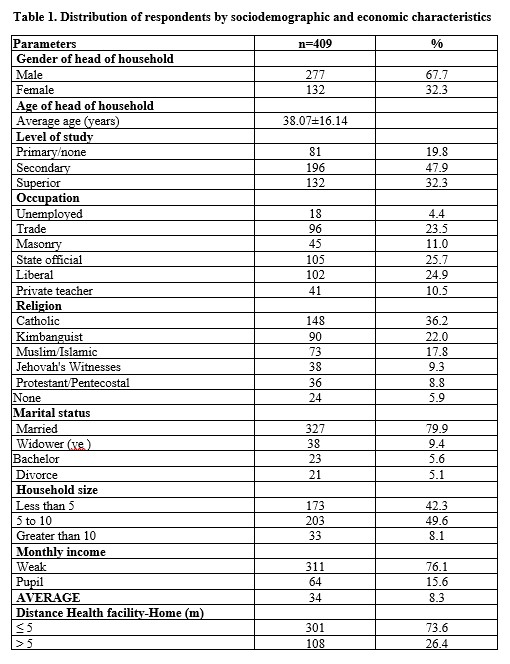
The total number of households visited was 409 that were included in our study (Table 1). The heads of households were in the majority male at 67.7% and the average age was 38.07±16.14 years. Most of our respondents had a secondary education level (47.9%) and nearly 25.7% were civil servants. The Catholic religion in our series was in the majority at 36.2%. Three-quarters of the heads of household were 79.9% married and the average number of people living in a household between 5 and 10 people was 49.6%. In 76.1% of households there was a low monthly income, it should be noted that 73.6% of households would travel in 5 km to reach a health training (distance between the house and the health centre).
Table 1. Distribution of respondents by sociodemographic and economic characteristics
Rate of use of curative services and therapeutic pathway
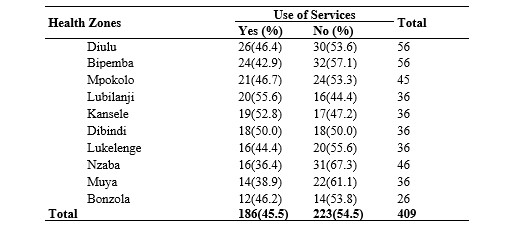
The lowest rate of utilization of curative care services was 36.4% in the Nzaba ZS. The overall rate of utilization of curative care services was 45.5% (Table 2).
Table 2. Distribution of health zones according to the rate of use of curative services and therapeutic itinerary by households
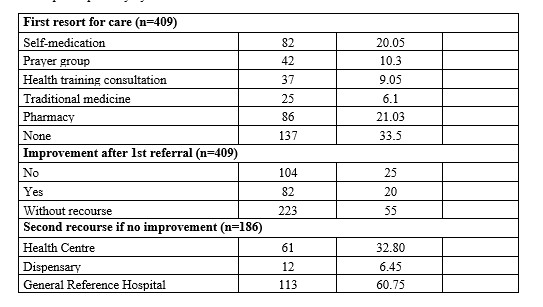
In Table 3, the distribution of health zones is contingent upon the utilisation of curative services and the therapeutic itinerary by households. As the table illustrates, firstly, the majority of heads of household (20.05%) resorted to self-medication, utilising the General Reference Hospital as a secondary option if there was no improvement in 60.75% and 32.80% resorted to the Health Centre, with only 10% stating that they used these places because they found adequate care there.
Table 3. Distribution of health zones according to the rate of use of curative services and therapeutic pathway by households
Method of payment for care and collection of the cost
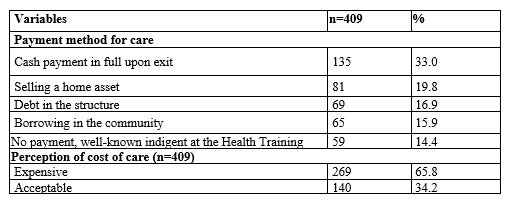
In Table 4, the distribution of households is depicted according to the manner in which care was financed and their perception of the cost in health facilities. The majority of heads of household (33%) paid in full for care on discharge, and 65.8% of respondents expressed that care was expensive (compared with 34.2% who said it was acceptable).
Table 4. Distribution of households according to the method of payment of care and the perception of cost in the health facilities
Factors associated with the use of curative services and therapeutic itineraries
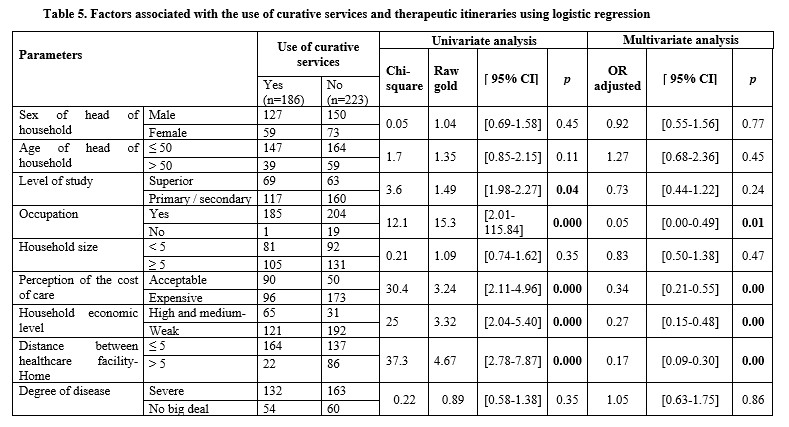
In univariate analysis (Table 5), heads of households with a higher level of education, occupation, those who perceive the cost of care as acceptable, high and medium economic level of the household, and distance between health education and home of less than or equal to 5 were, respectively, 1.49, 15.3, 3.24, 3.32, and 4.67 times more likely to use curative services. This difference was statistically significant (p < 0.05). The results of the multiple logistic regression analysis. We included the following variables in the regression model: age, sex, education level, household head occupation, household size, perceived cost of care, household economic level, distance health training-Home and the degree of illness and use of curative services. Regression analysis identified factors that are associated with the use of curative services, after adjustment. The profession, the perception of the cost of care, the economic level of the household and the distance health education-home were associated with the use of curative services.
DISCUSSION
The utilisation of health services constitutes a pivotal component in enhancing the health status of the population. In a health system organised based on health districts, the initial point of contact with the health system in cases of illness is the primary level of the health district (or health zone). The objective of this study is to ascertain the utilisation of curative services and the therapeutic trajectory in Mbuji-Mayi, DRC. The regression analysis revealed that occupation, perception of the cost of care, household economic level and distance from the health facility were associated with the utilisation of curative services. These findings are consistent with those reported by Kahindo et al.[12] in Goma, a similar urban environment, and contrast with the results of Mozart[14] and Karamoko Dédeou[15], who identified an association between the educational level of the heads of household.
The present study revealed a notable preference for informal pharmaceutical services and self-medication in the urban community of Mbuji-Mayi (21.05 and 20). In the first case, 9.05% of respondents had used a health facility, while 186 said they had consulted health facilities as a second resort. Within the primary level of the health district, 32.80% of respondents visited a health centre, while 6.45% went to a dispensary. At the secondary level, 60.75% of respondents utilised a health facility, indicating a notable shift in the pattern of utilisation. It is noteworthy that a significant proportion of respondents did not use any facility in the initial instance (33.5%), underscoring the need for further investigation into the reasons for this behaviour. The combined use of pharmacies and self-medication in the first instance (41.1%) is like the results obtained by Chenge et al.[11] and Kahindo et al.[12] in urban and rural areas, by Philippe et al.[16] in the DRC and by Nkomo[17] in Cameroon.
The frequent and simple use of self-medication, prayer groups and traditional medicine may be associated with the sector's lack of regulation, low purchasing power, the proximity of pharmacies and the poor integration and supervision of options for finding solutions to health problems by the population, which is a valid aspect of community health in the health system. However, this phenomenon has been well documented in the literature[9]-[11] in our environment and throughout the world.[18]-[24] Despite the country's experience of community medicine in the 1970s, particularly in Bwamanda (Equateur province), Kisantu (Bas-Congo province), Katana (South Kivu province), Kasongo (Maniema province) and Vanga (Bandundu province)[25],[26] there is a paucity of research on the topic.
The considerable frequency of self-medication among patients in urban areas, largely due to the unavailability of adequate health services, particularly at the primary care level, calls for a reassessment of the current organisation and regulatory framework governing health services in urban areas. The findings of this study underscore the significance of comprehensive and integrated health service delivery. Moreover, the study emphasises the incorporation of the concept of proximity in urban environments, such as Mbujimayi, where accessibility to services may be limited. This underscores a notion of interconnectedness that transcends mere physical proximity, emphasising instead the presence of affinities, regular interactions, or common interests among patients and service providers.
The World Health Organisation (WHO)[29] asserts that direct household payments remain the predominant health financing modality, with no indication of a decline.[30] The Health Financing Strategy aspires to progressively diminish the role of out-of-pocket payments in medical financing, as this modality constitutes the primary contributor to catastrophic and degrading expenditure in the DRC[30], thereby reflecting constrained financial protection against disease-related hazards.[31],[32] This is problematic as it hinders progress towards the objectives set by the CSU and reflects a lack of political commitment. As asserted by Nauleau et al.[33], 'the implementation of the UHC goal is contingent on national public policy frameworks'. In their study, Tangcharoensathien et al.[34] draw on examples of countries that have achieved their targets and demonstrate that the transition to UHC is first and foremost a political decision. Furthermore, a study conducted in Kenya emphasised that strategic leadership from the top is essential to ensure clear political implementation and consistent and logical conduct of UHC, in line with one of the core values of public health (equity).[35]
Research undertaken in Canada by Pineault and Daveluy has demonstrated that factors influencing the utilisation of healthcare services are influenced by gender and age.[36] Regarding educational attainment, 47.9% of heads of household had obtained secondary education, which is lower than the figure reported by Mozart M.[14], who found that 61.1% of heads of household in Central Kongo had achieved secondary education. Karamoko Dédeou[15] found that 60% of cases involved heads of household with no education. The survey yielded valuable insights from a representative sample of households. The application of the methodology, adherence to data collection procedures and techniques, and the processing and analysis of the data yielded reliable information, thereby facilitating the assessment of the study's validity. However, the risk of memory bias in the answers to questions requiring recall is acknowledged as a potential constraint of the study. Pineault and Daveluy's Canadian research on the factors influencing the use of healthcare services demonstrates that both gender and age have a significant impact on the utilisation of healthcare services.[36] With respect to educational attainment, the study found that 47.9% of heads of household had attained secondary education. This figure is lower than that reported by Mozart M., who found that 61.1% of heads of household in Central Kongo had achieved secondary education. Karamoko Dédeou found that 60% of cases involved heads of household with no education. The survey yielded valuable insights from a representative sample of households. The application of the methodology, adherence to data collection procedures and techniques, and the processing and analysis of the data yielded reliable information, thereby facilitating the assessment of the study's validity. Nevertheless, the risk of memory bias in the answers to questions requiring recall was identified as one of the study's constraints.
CONCLUSION
The findings indicate that, when confronted with illness, most of the urban population initially sought self-medication, prayer groups, or traditional medicine. This decision was primarily influenced by financial constraints associated with accessing healthcare services. This study underscores the need for targeted interventions to improve healthcare utilization in Mbuji-Mayi, including the regulation of informal health sectors, financial support mechanisms, and improved accessibility through UHC initiatives.
Funding
There were no external funds for this research.
Getting the data and materials
The datasets produced/analysed in this study can be found in the Determinants of the low rate of use of curative services and therapeutic itineraries in Mbuji-Mayi repository.
Ethics approval and consent to participate
Prior to its implementation, the research protocol was submitted to the Ethics Committee of the Official University of Mbujimayi for approval […].
Prior to their inclusion in the study, participants were provided with a detailed explanation of the study's objectives, potential advantages, and disadvantages. The participants were at liberty to provide their consent, either verbally or in writing, in an informed and voluntary manner. Accordingly, the confidentiality of the information collected will be guaranteed in accordance with the attached model of free and informed consent.
Consent for publication
None.
Authors' contributions
All authors read and approved the final manuscript to supervision.
CTK, CKM, PMM, and AMLK: Study concept and design.
CTK, CKM, FKT, CKD, and BKI: Data collection.
CTK, PMM, FKT: Contributed to data analysis, data interpretation, and drafting of the original manuscript.
CTK, CKM, and CKD: Contributed to data curation.
PMM, FKT, and CKM: Contributed to writing-review and editing.
CKM, CKD, and AMM: Final manuscript for critical revision and approval.
REFERENCES
- World Health Organization (WHO). Couverture sanitaire universelle (CSU) [Internet]. WHO: Geneva; 2023 oct [cité 15 déc 2024]. Disponible sur: https://www.who.int/fr/news-room/fact-sheets/detail/universal-health-coverage-(uhc)
- Organisation Mondiale de la Santé (OMS). Rapport sur la santé dans le monde 2008: les soins de santé primaires - maintenant plus que jamais [Internet]. Geneva: WHO; 2008 [cité 31 déc 2022]. Disponible sur: https://iris.who.int/handle/10665/43951
- Organisation Mondiale de la Santé (OMS). Rapport sur la santé dans le monde 2010: Le financement des systèmes de santé. Le chemin vers une couverture universelle. Geneva: WHO; 2010.
- Organisation Mondiale de la Santé (OMS), Banque Mondiale. Rapport mondial de suivi 2017: la couverture-santé universelle. Genève: WHO et Banque Mondiale; 2018.
- World Health Organization (WHO). Statistiques sanitaires mondiales 2014 [Internet]. WHO: Geneva; 2014 mai [cité 15 déc 2024]. Disponible sur: https://www.who.int/fr/publications/i/item/9789240692671
- Tape YB. Analyse économétrique de l’itinéraire thérapeutique des ménages de Côte d’Ivoire. 2007 [cité 15 déc 2024]. Disponible sur: https://corpus.ulaval.ca/bitstreams/c1e5a7df-4216-4760-9038-617ece65f8e3/download
- Ouendo EM et al. Itinéraire thérapeutique des malades indigents au Bénin. Trop Med Int Health. 2005;10(2):179‑86.
- Ouédraogo M et al. Itinéraire thérapeutique des tuberculeux bacillifères au Burkina Faso. Int J Tuberc Lung Dis. 2006;10(2):184‑7.
- Manzambi Kuwekita J. Les déterminants du comportement de recours à la polyclinique conventionnée en milieu urbain africain. Rev Psychol Société Nouv [Internet]. 2009 [cité 15 déc 2024]. Disponible sur: https://orbi.uliege.be/handle/2268/141338
- Chenge MF et al. Health-seeking behaviour in the city of Lubumbashi. BMC Health Serv. Res. 2014;14:173. https://doi.org/10.1186/1472-6963-14-173
- Kahindo JB et al. Itinéraire Thérapeutique du Patient en Milieu Urbain Africain. Int. J. Innov. Sci. Res. 2021;53.
- Division provinciale de la santé KASAI-ORIENTAL. Rapport annuel. Mbuji-Mayi; 2022.
- Mairie de Mbujimayi. Cartographie du territoire Urbain de la Ville de Mbujimayi. 2019.
- Mozart M. Déterminants de l’utilisation des services curatifs à l’Hôpital Général de Reference Gombe-Matadi. 2017.
- Karamoko Simaga. Facteurs déterminants de la faible utilisation des soins curatifs du CS Communautaire de Lassa. 2017.
- Philippe CM et al. Facteurs déterminants la faible utilisation des services curatifs en RDC. Pan Afr. Med. J. 2015;21. https://doi.org/10.11604/pamj.2015.21.173.6554
- Nkoma PP. Itinéraires thérapeutiques des malades au Cameroun. Johannesburg, 2015.
- White KL et al. The Ecology of Medical Care. N Engl J Med. 1961;265:885–92.
- White KL. The ecology of medical care: origins and implications. Health Serv Res. 1997;32:11–21.
- Godwin M et al. Need for an institute of primary care research. Can Fam Physician. 1999;45:1405.
- DeFriese GH. A brief symposium: In honor of Kerr L. White. Health Serv Res.
- McWhinney IR. An introduction to family medicine. 1981.
- Harmon RG. The National Primary Care Conference–executive summary. Wash. DC Dep. Health Hum. Serv. 1992.
- Green LA et al. The Ecology of Medical Care Revisited. N Engl J Med. 2001;344:2021–5.
- Equipe du Projet Kasongo. Utilisation du personnel auxiliaire dans les services de santé ruraux. WHO Bull. 1976;54:625–32.
- Lamboray JL. La zone de santé rurale de Kisantu, Zaïre. Ann Soc Belge Med Trop. 1979;15–32.
- Ngolo Kwete. Accessibilité financière aux soins curatifs. 2018-2019.
- Ministère du plan. Enquête Démographique et de santé (EDS-RDC). 2013-2014.
- WHO. Spending on health: A global overview [Internet]. WHO: Geneva. 2024. Disponible sur: https://www.who.int/news-room/fact-sheets/detail/spending-on-health-a-global-overview
- Ibanda Mvunzi E. Progrès vers la Couverture Santé Universelle. 2021.
- Banque Mondiale. Améliorer l’accès aux soins de santé primaires. Rapport 2023.
- Ministère de la Santé RDC. Plan Stratégique National pour la Santé 2022-2026.
- Kone P et al. Impact des politiques de santé sur l’accessibilité financière aux soins. Santé Publique. 2018.
- UNICEF. Rapport sur la santé des enfants en Afrique Centrale. 2023.
- OMS. Évaluation des systèmes de santé en Afrique subsaharienne. 2020.
- Zoungrana A. Les défis de l’assurance maladie en Afrique. 2019.
Medical Journal of Zambia, Vol 51, 4
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.