Knowledge and awareness levels of radiation protection among final-year clinical officer students at Levy Mwanawasa Medical University of Zambia
Osward Bwanga
Midland University Hospital Tullamore, Radiology Department
Eves Bbabbi
Levy Mwanawasa Medical University, Department of Radiography
James Sichone
University of Zambia, Department of Radiography
Phanny Nankonde Sichone
Levy Mwanawasa Medical University, Department of Radiography
DOI: https://doi.org/10.55320/mjz.52.1.610
Keywords:Awareness, Clinical officer student, Knowledge, Medical exposure, Radiation Protection
ABSTRACT
Background: Using ionising radiation in medicine to diagnose and treat diseases and injuries is the most significant source of human exposure from man-made sources. Ionising radiation has biological effects on human tissue. For this reason, the referring clinician must show how the medical exposure will benefit the patient over any potential detriment. Clinical officer students are future referring clinicians, so understanding radiation protection is vital in educating patients, gaining informed consent, and justifying medical exposures.
Aim of the study: To assess radiation protection knowledge and awareness levels among final-year clinical officer students at Levy Mwanawasa Medical University (LMMU) of Lusaka. Methods: A cross-sectional descriptive study was conducted among final-year clinical officer students. All final-year clinical officer students (N=129) at LMMU were invited to participate in this survey. Data were collected using an online questionnaire in October 2024. Descriptive analysis using frequencies and percentages was used to present data. A Mann-Whitney test was performed to test the significant difference between clinical officer students who attended a presentation on radiation protection and those who did not. Results: The study found that the total number of respondents in the survey was 90. The distribution median was 45% (IQR 36-64), indicating that the average score for the group was below the pass criteria of 50% used for academic examinations in Zambia. However, the awareness of the justification process was high, with a median score of 100 (IQR 80-100). Interestingly, there was no significant difference in knowledge and awareness levels between clinical officer students with previous exposure to a presentation on radiation protection and those without. Most notably, the majority N=89 (98.9%) of clinical officer students expressed the need to integrate radiation protection into the clinical medicine curriculum at LMMU. Conclusion: The findings highlighted low knowledge levels about radiation protection and a high awareness of the justification process among clinical officer students. It is strongly recommended that radiation protection be incorporated into the clinical medicine curriculumINTRODUCTION
Medical imaging services have played an important role in diagnostic medicine since Professor Wilhelm Roentgen discovered X-radiation in 1895.[1] The reported benefits associated with medical imaging examinations include saving the patient’s life by providing the correct diagnosis and treatment, eliminating diseases that affect the management of the patient, and making a diagnosis with an examination that has less morbidity and mortality.[2][3] It is estimated that 30% to 50% of critical decisions in medicine are based on medical imaging examinations.[4] However, most of these examinations involve ionising radiation, which has biological effects on human tissue.[5] Radiation exposure may increase the risk of developing cancer, damage the skin, and cause radiation-induced cataracts.[3][6][7] Furthermore, radiation exposure can damage the deoxyribonucleic acid (DNA) in reproductive cells, leading to genetic mutations that can be passed on to future generations.[6] This risk of harm with the use of radiation led to the introduction of protective regulation worldwide.[1][3]
The legislation and regulations for requesting radiological examinations in each country are based on the recommendations of the International Commission on Radiological Protection (ICRP). The ICRP recommendations guide national legislation in different countries, such as Zambia's Ionising Radiation Protection Act of 2011.[8] Before each medical imaging exposure can occur, the referring clinician must justify the examination by showing benefits to the patient over any potential harm it may cause.[5][6] Currently, clinicians are requesting and relying on medical imaging more than ever.[1] This is evidenced by the significant rise in imaging examinations from 3.6 million in 2008 to 3.6 billion in 2016.[9][10] It is estimated that about 30% of these examinations are unjustified.[9] The ICRP has recommended integrating radiation protection into the curriculum of medical students and other health professionals who use radiation during the course of their work,[11] such as clinical officers.
In Zambia, clinical officers are among the clinicians who refer patients for limited medical imaging examinations.[12] A clinical officer is a title given to someone with a diploma in clinical medicine and surgery who is licensed to practice medicine.[12][13] According to Kamfwa,[13] clinical officers are among the major drivers of primary healthcare and handle a majority of up to 80% of all patients who visit health facilities in Zambia. At Levy Mwanawasa Medical University (LMMU), clinical officer students are introduced to radiology in the first year of their training programme.[14] Students are attached to the radiology department during their screening rotation and can request plain film and ultrasound examinations under supervision. However, the theory component does not include radiation protection; the students learn this during their clinical attachment. Clinical officer students represent future referring clinicians; unless they are taught about radiation protection, they cannot make appropriate, informed clinical decisions regarding the justification of medical exposures.[15] Therefore, this study aimed to assess radiation protection knowledge and awareness levels among final-year clinical officer students at LMMU of Lusaka.
METHODS
A cross-sectional descriptive study was conducted using an online survey questionnaire. This study design allowed the researchers to collect data on the knowledge and awareness levels of radiation protection among final-year clinical officer students, observing the variables without influencing them.[16] This study was conducted at LMMU in the School of Medicine and Clinical Sciences. LMMU was established in 2018 as a public university to offer educational programmes in various medical, nursing, and allied health professions.[17] One of the education and training programmes offered is a three-year diploma in clinical medicine and surgery for clinical officers. The university is affiliated with the Levy Mwanawasa University Teaching Hospital (LMUTH), which has an 850-bed capacity.[18] The radiology department at LMUTH offers medical imaging services in general (plain film) radiography, theatre radiography, fluoroscopy, ultrasound (US), computed tomography (CT), magnetic resonance imaging (MRI), and interventional radiology. Therefore, these academic and clinical settings provided an ideal environment for conducting this survey.
Study population and samplingGenerally, a sample of the population is required to conduct a survey for theoretical and practical reasons. Only part of the population is approached in a sample survey to participate in the research study, and this reduces the costs and time required to plan and conduct research.[16][19][20] However, all final-year clinical officer students (N=129) at LMMU were included in this survey due to the moderate population size involved. This enumeration of the whole population is called census sampling.[16] Conducting a census survey often results in enough responses to have a high degree of statistical confidence in the results, there are no sampling errors, and it provides universal coverage.[16][19][20] In this survey, universal coverage to include the whole population was necessary as the results and recommendations will affect future clinical officer students at LMMU.
Data collection tool and procedureThe data for this survey were collected using an online self-completion questionnaire. The researchers developed the questionnaire based on the European Union (EU) radiation protection curriculum for medical students[21] and previous research studies.[1][4][15][22][23][24] Literature from medical students was used because they have similar roles in referring patients for imaging examinations as clinical officers. The questionnaire had four sections. The first section dealt with respondents’ demographic information, including age, gender, and attending a presentation on radiation protection. The second section focused on respondents' knowledge of radiation protection. It contained ten multiple-choice questions on medical imaging modalities, the biological effects of radiation, the justification principle of radiation protection, and measures used to control external radiation exposure. The third section focused on awareness levels related to the justification process. It had five awareness statements with “Yes”, “No”, or “Not sure” answers. The last section had two questions: whether the respondents agreed to include radiation protection in clinical medicine curricula and the type of model delivery.
Following ethical approval and obtaining permissions, contact was made with the Head of Department and class representative. The pilot questionnaire created using Google Forms was tested on N=13 (10%) with potential respondents to ensure the feasibility of the data collection tool and detect any flaws or problems with the questions and statements.[16] After the pilot study, the online survey questionnaire was sent to the final-year clinical officer student class representative, who shared it on their class WhatsApp group. The total eligible respondents were 116, excluding those who participated in the pilot study. Data was collected in October 2024, and weekly reminders were sent to increase the response rate.
Data management and analysisTen multiple-choice questions assessed knowledge about radiation protection, and five statements with “Yes,” “No,” and “Not Sure” categories assessed awareness of the justification process. The correct answer or “Yes” was awarded one mark, whereas an incorrect answer, omission, “No”, or “Not sure” received zero marks.[15][22] The total score for each respondent was calculated by summing up all correct or “Yes” answers. The pass mark for knowledge questions was set at 50%, which is used for academic examinations in Zambia. The data was tested for normality using the Shapiro-Wilk test with a level of significance set at 0.05. Data that were not normally distributed were subjected to parametric tests, and those that were not subjected to nonparametric tests. A Mann-Whitney test was performed to test the significant difference between clinical officer students who attended a presentation on radiation protection and those who did not.
Ethical considerationsThe Levy Mwanawasa Medical University Research Ethics Committee (LMMUREC) committee granted ethical approval for the survey (LAMU-REC 0000329/24). Further clearance was obtained from the National Health Research Authority (Ref: NHRA6255/13 /08/2024). Permission was also obtained from the LMMU management through the office of the Dean of Students. Details about the survey were disclosed to potential respondents, and informed consent was obtained online before each respondent completed the questionnaire. The researchers adhered to the four ethical principles of research: autonomy, beneficence, non-maleficence, and justice, as well as the Data Protection Act of Zambia.[25]
RESULTS
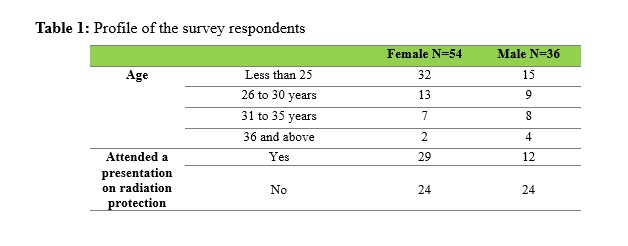
The total number of responses in the survey was 90, representing 78%. The females accounted for N=54 (60%), whilst the males constituted N=36 (40%), as shown in Figure 1 below. In terms of age, the majority N=47 (52.29%) of respondents were under 25.
Knowledge of radiation protection
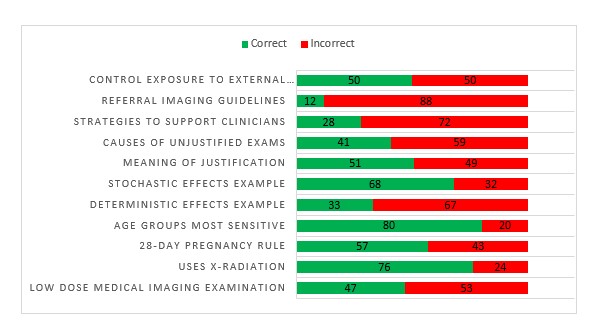
Ten questions were constructed to assess the clinical officer students' knowledge of radiation protection. The performance of each item is shown in Figure 1. The best performance was on questions that assessed the knowledge of respondents to the age group most sensitive to ionising radiation (N=72; 80%), medical imaging examinations that use X-radiation (N=68; 76%), and the stochastic effects of ionising radiation (N=61; 68%). The lowest performance was in referral imaging guidelines (N=18; 20.2%).
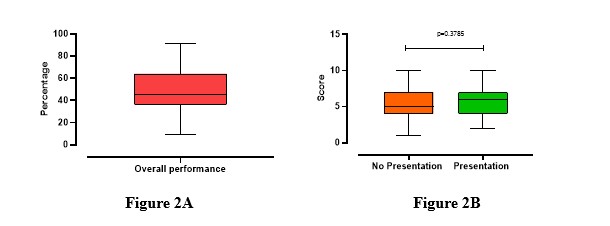
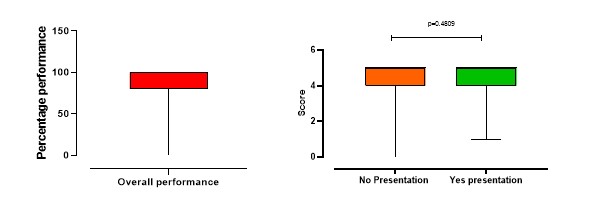
Overall radiation protection knowledge levels
The overall performance of knowledge questions was tested for normality using the Shapiro-Wilk test and was non-parametric (p= 0.0410). The distribution median was 45% (IQR 36-64). When compared to the pass mark used for academic examinations in Zambia (50%), it was noted that the average score for the group was below the pass criteria set for Zambian Higher Education Institutions (HEIs). When a comparison was made in the performance of those who had an opportunity to attend a radiation protection presentation and those who did not, it was found that no significant difference (p= 0.3785) was noted in their scores on the assessment for general knowledge of radiation protection. The figure below shows the overall performance (Figure 2A) and the comparison of the performance (Figure 2B).
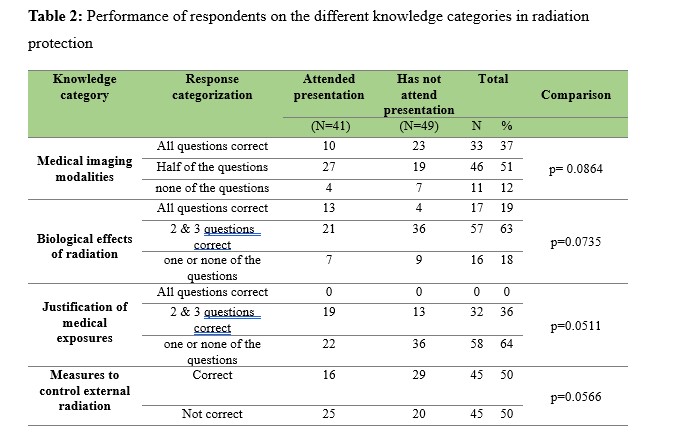
When a sub-analysis of the respondents' performance in the knowledge category subgroups was undertaken, it showed no significant difference in performance between individuals who had attended a presentation on radiation protection and their counterparts who had not. Table 2 shows the performance in the subgroups, and a Mann-Whitney test shows no significant difference, as depicted by the various p-values above the 0.05 set level.
Table 2: Performance of respondents on the different knowledge categories in radiation protection
Awareness of justification of process scores
Five statements were provided to establish the respondents' awareness levels regarding the justification process of medical imaging examinations. The responses to the five awareness statements are summarised in Table 3. The level of awareness of the justification process was generally high, and there was no difference between the individuals with previous exposure to a presentation on radiation protection and those who did not.
Table 3: Awareness of justification process scores
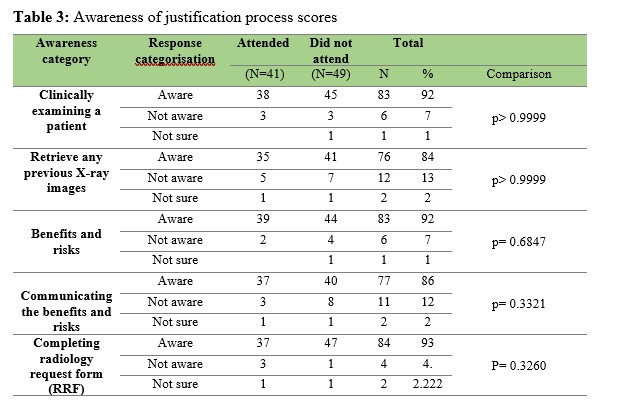
General awareness levels of the processes involved in the justification of medical exposure
The majority of the respondents demonstrated a high level of awareness regarding the justification process, as shown by a median score of 100 (IQR 80-100). When comparing those who attended the presentation with those who had not, the level of awareness of the justification process was not significantly different (p=0.4809).
Suggestions for training in radiation protection
The respondents were asked to make recommendations for the future. Almost all respondents, N=89 (98.9%), agreed that the radiation protection programme should be integrated into the primary curriculum for the diploma in clinical medicine programme at LMMU. The delivery model that was most preferred was the blended mode of delivery, N=49 (54%). This was followed by a second preference for a physical classes approach, which accounted for N=37 (41%).
DISCUSSION
This study assessed radiation protection knowledge and awareness levels among final-year clinical officer students at LMMU of Lusaka. To the authors' best knowledge, this is the first research to be conducted on clinical officer students on this subject. There was a scarcity of literature to discuss the findings. Therefore, literature from the medical profession is used since both professions play a similar role in referring patients for imaging examinations.
Knowledge of clinical officer students to radiation protectionThe first thematic area assessed in our survey was medical imaging modalities. Most N=48 (53.3%) clinical officer students did not know mammography is a low-dose imaging examination. CT and fluoroscopy are high-dose medical imaging examinations, while ultrasound and MRI have no radiation dose.[6][26][27] Dual-energy X-ray absorptiometry (DEXA) uses X-radiation and is a low-dose examination,[28] and the majority, N=72 (80.0%) of respondents answered correctly. Unfortunately, a few N=6 (6.7%) clinical officer students did not know that ultrasound and MRI do not use X-radiation. This is a lower percentage than that of medical students in an Ethiopian study conducted by Amare and Dagne,[22] where N=92 (19.5%) respondents incorrectly labelled MRI as an examination which uses X-radiation. This information helps referring clinicians choose the appropriate modality for a given condition and reduce medical exposures to ionising radiation.
The second thematic area focused on in this survey was the biological effects of ionising radiation on human tissue. The foetus is most radiosensitive due to rapid cell proliferation, migration, and differentiation.[29][30] For this reason, the pregnancy status of female patients of reproductive age should be determined before any medical exposure to the pelvic region.[2][30][31] The two approaches used are the 10- and 28-day pregnancy rules.[30] The rules state that whenever possible, one should confine the radiological examination of the lower abdomen and pelvis to the 10-day interval following the onset of menstruation for high-dose examinations such as CT, intravenous urography (IVU), and fluoroscopy, and 28-day interval for medium and low-dose examinations such as abdominal X-ray and DEXA.[30] However, a few N=18 (20%) and less than half of N=41 (44.3%) of clinical officer students did not know that a foetus is the most sensitive to ionising radiation among the age group (foetus, infants, adolescents, and elderly) and an examination which applies the 28-day pregnancy rule, respectively. A lack of knowledge may expose pregnant patients to unnecessary medical exposures[26] and put the foetus at risk of deterministic effects of ionising radiation. The majority N=69 (76.7%) and N=61 (68.5%) of clinical officer students knew the clinical examples (signs) of the deterministic and stochastic effects of ionising radiation, respectively. Deterministic effects typically have a threshold level that, when exceeded, will cause tissue damage.[2][5][6][32] Examples include hair loss, infertility, acute radiation syndrome, and cataracts. On the other hand, stochastic effects are random without a threshold, hence the need to limit exposure.[2][5][6][32] Examples include cancer and hereditary effects. Sometimes, a patient can present signs of ionising radiation effects to the medical facility. Therefore, clinical officers and other clinicians must know these signs to avoid missing the diagnosis.
The third thematic area focused on the justification of medical exposures. In our study, N=44 (48.9%) clinical officer students did not know the meaning of the justification principle. It means showing the benefits of medical exposure to the patient over any potential harm it may cause.[5][6] It should be mentioned that the goal of justification is to avoid unnecessary radiological examinations, resulting in patients being unnecessarily exposed to radiation and its potential risks.[3][5][33] Literature has identified three strategies to support referring clinicians in justifying medical exposures: education and training, developing and using imaging referral guidelines, and conducting clinical audits of the justification process.[33][34][35] In this survey, N=37 (41.6%), clinical officer students incorrectly indicated that communication between radiographers and referring clinicians was one of the main causes of unjustified imaging examinations. On the contrary, this communication resolves issues before the patient is exposed to ionising radiation and helps avoid unnecessary medical exposures. Clinical officer students were asked to identify the information that is found in the referral medical imaging guidelines. The majority of N=72 (79.8%) correctly answered that it provides referring clinicians with clinical and diagnostic problems, a list of possible imaging modalities with the band of radiation exposure involved, levels of radiation doses for each type of procedure, and recommendations on whether the investigation is appropriate. Unfortunately, Zambia has no imaging referral guidelines.[23]
Measures used to control external radiation exposure were the fourth thematic area assessed in this survey. Time, distance, and shielding are three measures to control exposure to external ionising radiation during theatre radiography.[6] Firstly, the amount of radiation dose by the patient and staff during theatre radiography is directly proportional to the exposure time.[3][18] Secondly, standing further away from the mobile fluoroscopic X-ray machine during exposure reduces the radiation dose received by staff.[3][18] Thirdly, wearing personal protective equipment (shielding) during theatre radiography protects staff from external radiation (scattered radiation).[18] In our survey, clinical officer students were asked to identify the measures used to control external radiation exposure during theatre radiography; half N=45 (50%) correctly identified the correct answer as time, distance, and shielding. Clinical officer students or clinical officers sometimes work in the operating theatre. Therefore, understanding these cardinal radiation protection rules is paramount to protecting themselves, other theatre staff, and patients.
This study found low knowledge levels about radiation protection among clinical officer students. This may be due to the unavailability of radiation protection in the diploma in clinical medicine and surgery at LMMU.[14] Literature revealed that radiation protection knowledge is best acquired through educational programmes.[1][11][21]
Awareness of clinical officer students to the justification processThe operationalisation of the justification principle starts with clinically examining a patient before requesting any imaging examination. In our survey, a few N=6 (6.7%) clinical officer students were unaware of this. This is not surprising and concurs with a study conducted in the UK by Bosanquet et al.[36] which revealed that medical doctors do not see patients before being sent for imaging examinations in a third of radiology requests. Clinical officer students were also asked if they knew that a referring clinician should try to retrieve any previous images or diagnostic reports before requesting another examination, with a few N=12 (13.7%) clinical officer students indicating that they were unaware that they should do so. These practices aim to avoid exposing patients to unnecessary radiation, as some conditions can be treated based on the physical assessment and information from the result of the previous imaging or the use of non-ionising examinations such as ultrasound and MRI.
Under Zambia's Ionising Radiation Protection Act of 2011, referring clinicians are responsible for justifying each medical exposure.[8][33] This process involves considering the benefits and risks of exposing the patient to radiation and communicating such with the patient. In our survey, a few N=6 (6.7%) and N=11 (12.5%) clinical officer students, respectively, were unaware of the responsibility given to referring clinicians for considering and communicating the benefits and risks of exposing the patient to ionising radiation. Communication of the benefits and risks of medical exposure is part of the informed consent process and promotes patient autonomy.[37] The Health Professions Council of Zambia (HPCZ) guidelines on informed consent[38] state that clinicians should inform patients of the benefits and risks associated with treating and managing their conditions, including medical exposures to ionising radiation.
From the referring clinician's perspective, the last stage of the justification process is completing a radiology request form (RRF). The RRF is a communication tool between the referring clinician and imaging professionals.[28] All the information on the RRF must be completed adequately and legibly.[39] However, a few N=4 (4.5%) clinical officer students were unaware that all relevant information must be provided on the RRF. This lack of awareness can result in incomplete filling in the RRF. For example, an audit conducted in Zambia by Chanda et al.[28] found that of all the variables (N=14) audited, only the names and genders of the patients were provided in all RRFs. Another recent audit by Bwalya et al.[31] revealed that most N=881 (90.5%) RRFs were incompletely filled by referring clinicians. If the RRF is not completely filled, it becomes a grave imaging error and can result in misunderstandings between the referring clinician and imaging professionals.[28][31][39][40] This can lead to unnecessary exposure of patients to radiation or repetition of an examination.
This study found that clinical officer students are highly aware of the justification process. Final-year clinical officer students request plain film and ultrasound examinations during clinical placements, which may increase their awareness of the steps involved in requesting medical imaging examinations. Another explanation may be due to response bias, where people do not answer questions or statements truthfully for some reason.[41][42]
Education and training in radiation protectionIn this survey, almost all clinical officer students indicated the need to integrate radiation protection into their curriculum. The development of the curriculum can be based on the EU[11] radiation protection curriculum for medical students and ICRP[21] recommended topics: biological effects of ionising radiation, radiation quantities and units, principles of radiation protection, radiological protection legislation, and the factors in practice that affect patient and staff doses (time, distance, and shielding). Previous studies have found that medical students' knowledge and radiation protection awareness improve following formal training.[1][43] For example, in a study by Hagi and Khafaji[44] in the Kingdom of Saudi Arabia (KSA), the average medical student score improved from 47% to 78% following radiation protection training. Our study found no significant difference in knowledge and awareness levels between clinical officer students who had previously attended a presentation on radiation protection and those who had not. This explanation may be that presentations are not formal courses that include a more significant study period, assessments, and longer knowledge retention.[11][21][45]
LIMITATIONS OF THE STUDYThis study had three limitations. Firstly, clinical officer students who participated in this survey were recruited from one HEI offering a clinical medicine and surgery diploma. Therefore, the sample was too homogenous to allow for the construction of more general conclusions. Secondly, being an online survey, some respondents may have googled the answers to knowledge questions. This would have made a high performance or score for the radiation protection knowledge questions. Thirdly, the answers to the awareness statements were self-reported. This may have resulted in some respondents presenting a favourable image or selecting a positive response option on awareness of the justification process. These social desirability and acquiescence response biases may lead to inaccurate self-reports and erroneous study conclusions.[41][42][46] Therefore, the results of this survey should be interpreted with these limitations in mind.
CONCLUSION
The study revealed that final-year clinical officer students at LMMU had low knowledge of radiation protection used in medicine, which was below average. However, they were highly aware of the justification process. This study highlights a critical need to integrate radiation protection education into the clinical medicine curriculum at LMMU. Addressing this educational gap will empower future clinicians to make informed decisions about medical exposures, enhancing patient safety and compliance with global best practices on radiation protection. A nationwide study is also recommended to survey all HEIs offering clinical medicine programmes in Zambia. This can give a good understanding of the problem.
COMPETING INTERESTThe researchers declare no conflict of interest.
ACKNOWLEDGEMENTThe researchers express gratitude to Ms Naomi Michelo, the class representative of final-year clinical officer students at LMMU, for her support throughout this research project and the contributions of all respondents who completed the questionnaire while writing their final examinations. This commitment from respondents is highly commendable. The researchers would also like to thank Lorna Mangan, Radiation Safety Officer of Midlands University Hospital Tullamore, Radiology Department, for her help in proofreading this article.
REFERENCES
- Mellis S, Zhang Y, McAteer D. Awareness of radiation risks by medical students and referrers requesting radiological examinations in the North of Scotland: an audit. BMC Med Educ. 2024;24(1):830. doi: 10.1186/s12909-024-05461-8. PMID: 39090574; PMCID: PMC11295379.
- Whitley AS, Jefferson G, Sloane KHC, Anderson G, Hoadley G. Clark’s positioning in radiography. 13th ed. London: CRC Press Ltd; 2015.
- Martin A, Harbison S, Beach K, Cole P. An introduction to radiation protection (7th ed). London: CRC Press; 2019.
- Tavakoli M, SeilanianToosi F, Saadatjou S. Knowledge of medical students on hazards of ionizing radiation. J Med Educ. 2003;3(1):3-6.
- International Commission on Radiation Protection. Recommendations of the international commission on radiological protection. London: SAGE Publication Ltd; 2007.
- Sherer MAS, Visconti PJ, Ritenour ER. Radiation protection in medical radiography. 9th ed. St. Louis: Mosby Elsevier; 2021.
- Bahadori P, Molina-Recalde AP, Saleh Alruwaili A, et al. Assessment of medical students' knowledge regarding radiation associated risk and its protection: finding from a cross-sectional study. Ir J Med Sci. 2024;193(3):1515-1519. doi: 10.1007/s11845-023-03583-4.
- Republic of Zambia. Ionizing radiation protection act of 2011 (Amended). Lusaka: Government printers; 2011.
- World Health Organization. Global initiative on radiation safety in healthcare settings. Geneva: WHO; 2008.
- World Health Organization. To X-ray or not to X-ray; 2016. From https://www.who.int/en/news-room/feature-stories/detail/to-x-ray-or-not-to-x-ray (Assessed 10 October 2024).
- International Commission on Radiation Protection. Education and training in radiological protection for diagnostic and interventional procedures. London: SAGE Publication Ltd; 2009.
- Health Professions Council of Zambia. Scope of practice for health practitioners registered under the Health Professions Council of Zambia. Lusaka: HPCZ; 2021.
- Kamfwa M. Zambia: The medical licentiates and the clinical officer duo. Social Innovation Journal; 2021. From https://www.socialinnovationsjournal.com (Accessed 10 November 2024).
- Levy Mwanawasa Medical University. Curriculum for diploma in clinical medical sciences. Lusaka: LMMU; 2020.
- O’Sullivan J, O’Connor OJ, O’Regan K, Clarke B, Burgoyne LN, Ryan MF. An assessment of medical students’ awareness of radiation exposures associated with diagnostic imaging investigations. Insights Imaging. 2010;1(2):86–92. doi: 10.1007/s13244-010-0009-8. PMID:22347909.
- Clark T, Foster L, Sloan L, Bryman A. Bryman’s social research methods (6th edition). Oxford: University Press; 2021.
- Levy Mwanawasa Medical University. University background; 2024. From https://lmmu.ac.zm/background.html (Accessed 10 November 2024).
- Bwanga O, Sindaza N, Chipulu M, Kinda PM, Mulenga J. A review of orthopaedic theatre radiography services in Zambia. Medical Journal of Zambia. 2023;50(2):169-179. doi: 10.55320/mjz.50.2.351.
- Australian Bureau of Statistics. Basic survey designs; 2023. From https://www.abs.gov.au/websitedbs/d3310114.nsf/home/Basic+Survey+Design+-+Samples+and+Censuses (Accessed 10 November 2024).
- Martínez-Mesa J, González-Chica DA, Duquia RP, Bonamigo RR, Bastos JL. Sampling: how to select participants in my research study? An Bras Dermatol. 2016 May-Jun;91(3):326-30. doi: 10.1590/abd1806-4841.20165254. PMID: 27438200; PMCID: PMC4938277.
- European Commission. Guidelines on education and training in radiation protection for medical exposures. Luxembourg: EC; 2001.
- Amare DE, Dagne H. Knowledge and associated factors of medical students regarding radiation exposure from common diagnostic imaging procedures at the University of Gondar, Ethiopia. Ethiop J Health Sci. 2020;30(4):589-598. doi: 10.4314/ejhs.v30i4.14.
- Siwila BD, Chipeya L.N.R, Mdletshe S, Sichone JM. Medical students' knowledge on the use of ionising radiation during medical imaging procedures in Zambia. Medical Journal of Zambia. 2021;48 (1): 31- 31. doi: 10.55320/mjz.48.1.50.
- Bahadori P, Molina-Recalde AP, Saleh Alruwaili A, et al. Assessment of medical students' knowledge regarding radiation associated risk and its protection: finding from a cross-sectional study. Ir J Med Sci. 2024;193(3):1515-1519. doi: 10.1007/s11845-023-03583-4.
- Republic of Zambia. The Data Protection Act, 2021. Lusaka: Government printers; 2021.
- Bwanga O. Knowledge, attitudes, and practices of referring medical practitioners regarding the justification of radiological examinations at the Ndola Teaching Hospital of Zambia. EAS Journal of Radiology and Imaging Technology. 2019; 1 (3): 78-88. doi: 10.36349/easjrit.2019.v01i03.002.
- Ehrlich RA, Coakes DM. Patient care in radiography: with an introduction to medical imaging (10th ed). London: Elsevier; 2020.
- Chanda E, Bwanga O, Sindaza N, Chipampe M, Chisha M. Audit of completion of computed tomography (CT) request forms at the Cancer Diseases Hospital (CDH) of Zambia. Medical Journal of Zambia. 2020; 47(4): 289 - 296. doi: 10.55320/mjz.47.4.122.
- International Commission on Radiation Protection. Pregnancy and Medical Radiation. London: SAGE Publication Ltd; 2000.
- International Atomic Energy Agency. Radiation protection of pregnant women in radiology; 2024. From https://www.iaea.org/resources/rpop/health-professionals/radiology/pregnant-women (Accessed 02 October 2024).
- Bwalya M, Bwanga O, Mvula JY, Munsanje F, Muntanga B. Adequacy of completion of radiology request forms at St. Francis' Hospital of Katete District: A clinical audit in Zambia. Malawi Med J. 2023;35(2):111-116. doi: 10.4314/mmj.v35i2.7.
- Hamada N, Fujimichi Y. Classification of radiation effects for dose limitation purposes: history, current situation and future prospects. J Radiat Res. 2014;55 (4):629-640. doi: 10.1093/jrr/rru019.
- Bwanga O, Nyanga I. Justification of imaging medical exposures: a review of literature to guide evidence-based practice in Zambia. Medical Journal of Zambia. 2020; 47(4): 318 - 326. doi: 10.55320/mjz.47.4.129.
- Remedios D. Justification: How to get referring physicians involved. Radiation Protection Dosimetry. 2011; 147: 47-51. doi: 10.1093/rpd/ncr263.
- Bwanga O, Chanda E. Challenges in radiation protection in healthcare: A case of Zambia. EAS Journal of Radiology and Imaging Technology. 2020; 2(1):7-14. doi: 10.36349/EASJRIT.2020.v02i01.00.
- Bosanquet D, Cho J, Williams N, Gower D, Thomas KG, Lewis M. Requesting radiological investigations - do junior doctors know their patients? A cross-sectional survey. JRSM Short Rep. 2013 Jan;4(1):3. doi: 10.1258/shorts.2012.012043. PMID: 23413405; PMCID: PMC3572658.
- Cardinal JS, Gunderman RB, Tarver RD. Informing patients about risks and benefits of radiology examinations: a review article. J Am Coll Radiol. 2011;8(6):402-408. doi: 10.1016/j.jacr.2010.09.007.
- Health Professions Council of Zambia. Guidelines for good practice in the health care profession- obtaining patients' informed consent. Lusaka: HPCZ; 2016.
- Royal College of Radiologists. Making the best use of clinical radiology services: referral guidelines (8th ed). London: The Royal College of Radiologists; 2017.
- Agi C, Alagoa PA, Fente BG. A simple audit of radiological request forms at the University of Port Harcourt Teaching Hospital. Niger Health J. 2015; 15:151-154. doi: 10.60787/tnhj.v15i4.240.
- Mazor KM, Clauser BE, Field T, Yood RA, Gurwitz JH. A demonstration of the impact of response bias on the results of patient satisfaction surveys. Health Serv Res. 2002;37(5):1403-1417. doi: 10.1111/1475-6773.11194.
- Hinz A, Michalski D, Schwarz R, Herzberg PY. The acquiescence effect in responding to a questionnaire. Psychosoc Med. 2007;4:Doc07. Published 2007 Jun 20.
- Hankin RA, Jones SP. The impact of educational interventions on clinicians' knowledge of radiation protection: An integrative review. Radiography. 2020;26(3):e179-e185. doi: 10.1016/j.radi.2020.01.008.
- Hagi SK, Khafaji MA. Medical students' knowledge of ionising radiation and radiation protection. Saudi Med J. 2011;32(5):520-524.
- Harden RM, Laidlaw JM. Essential skills for a medical teacher- introduction to teaching and learning in medicine (3rd edition). London: Elsevier;2020.
- Latkin CA, Edwards C, Davey-Rothwell MA, Tobin KE. The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore, Maryland. Addict Behav. 2017;73:133-136. doi: 10.1016/j.addbeh.2017.05.005.
Medical Journal of Zambia, Vol 52, 1
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.