Referring Medical Practitioners Experiences with Medical Imaging Services: Literature Review Findings and Implications for Zambia
Osward Bwanga
Midlands University Hospital Tullamore, Radiology Department, Ireland
Bornface Chinene
Harare Institute of Technology, Department of Radiography, Harare, Zimbabwe
Nchete Kapapa
Thomson District Hospital, Radiology Department, Zambia
DOI: https://doi.org/10.55320/mjz.51.4.607
Keywords:Experiences, Medical imaging services, Medical practitioners, Radiographer, Radiologist, Zambia
ABSTRACT
Background: Medical imaging examinations are essential in confirming, assessing and documenting the course of many diseases and response to treatment. It is estimated that half of the clinical decisions made by medical practitioners are based on imaging examinations. As internal service users, the experience of referring medical practitioners to medical imaging services can significantly impact patient safety and care. Patients will not be referred to this service if a referring medical practitioner does not find the service of good quality. There is no published review on this topic to consolidate the findings from previous studies and provide a basis for developing strategies to enhance the delivery of imaging services.
Aim of the study: To review the literature on the experiences of referring medical practitioners with medical imaging services and its implications for the Zambian healthcare system.
Methods: A narrative literature review was conducted from July to December 2024. The literature search was conducted via five databases: PubMed/MEDLINE, Scopus, Google Scholar, and Web of Science, as well as other sources. Research studies published in English from January 2000 to December 2024 were deemed eligible for inclusion. Data was extracted and re-analysed using thematic analysis.
Results:Six research studies met the inclusion criteria for this literature review. Limited studies exist on the experiences of referring medical practitioners to medical imaging services. Following data analysis, four themes were identified: medical imaging equipment and radiographic image quality, the shortage of imaging professionals, working relationships between referring medical practitioners and imaging professionals, and medical practitioners' interpretation of general radiographic images. The results show that medical practitioners in developing countries experienced more challenges than those in developed countries.
Conclusion:The review findings highlight significant challenges experienced by medical practitioners with medical imaging services. The main challenge that significantly affected the satisfaction of referring medical practitioners in developing countries was the lack of diagnostic imaging reports due to a shortage of radiologists. To fill this gap, it is recommended that the role of a radiographer be extended to include reporting on general radiographic images.
INTRODUCTION
Medical imaging services are essential in confirming, assessing and documenting the course of many diseases and response to treatment.[1 , 2] Globally, there is an increase in demand for medical imaging services. According to the World Health Organisation (WHO), since 2008, medical imaging examinations have risen from 3.6 million to 3.6 billion examinations performed annually. [2 ,3] 2, 3 This is due to the recent availability of a range of medical imaging examinations such as computed tomography (CT), magnetic resonance imaging (MRI), mammography, nuclear medicine, dual-energy X-ray absorptiometry (DEXA), and interventional radiology. Defensive medicine has also driven the increased usage of medical imaging services, resulting in unnecessary requests and increased workload for radiographers and radiologists. [4 ,5] As these services increase, patients and referring medical practitioners have complained about their quality.[6-8] The quality of medical imaging service is not just a concern, but a critical aspect that needs to be addressed. It includes timely access and delivery of appropriate medical imaging examinations and interventions in a safe and responsive facility.[7 , 8] It also consists of the crucial element of the delivery of accurate diagnostic reports promptly, a factor that cannot be overstated. [1 , 5] 1,5
It is estimated that half of the clinical decisions made by medical practitioners are based on medical imaging examinations.[9] 9 However, there is a considerable difference in the availability of medical imaging services between developed and developing countries. [2 , 9] This is due to challenges facing developing countries, such as a lack of advanced medical imaging modalities, affordability, shortage of radiologists, migration of radiographers to developed countries, and a lack of technical experts.[7,8, [11-13] It is important to note that medical practitioners play a pivotal role, as they are primarily responsible for requesting medical imaging examinations by completing a radiology request form (RRF) and adhering to radiation protection legislation and regulations on justification of medical exposures.[11 , 14]
The recommendations of the International Commission on Radiological Protection (ICRP) guide national legislation in different countries, such as Zambia's Ionising Radiation Protection Act of 2011.[15] Before each medical imaging exposure, the referring medical practitioner, a key player, must justify the imaging examination by demonstrating its benefits to the patient over any potential detriment.[14] 14 The radiographer then undertakes the imaging projections based on the information about the patient supplied on the RRF. [16] In return, the radiologist or reporting radiographer responds to the request with a written diagnostic report based on the imaging output.[11,17] The referring medical practitioner, as the primary user of the diagnostic imaging report, comprehends the report and utilises the findings in patient management of their medical condition.[11 ,17,18,19]
Given the above, it is imperative that referring medical practitioners have a comprehensive understanding of medical imaging examinations, including basic radiation protection and image interpretation. Equally important is establishing strong working relationships between referring medical practitioners and imaging professionals (radiographers and radiologists). Surprisingly, there is no published literature review on this topic to consolidate the findings from previous research studies and provide a basis for developing strategies to enhance the delivery of medical imaging services. As critical stakeholders, the experience of referring medical practitioners to medical imaging services can significantly impact patient safety and care.[5 ,20] The reviewers have heard medical practitioners complaining about the quality of medical imaging services in Zambia and beyond. Therefore, this study aimed to review the literature on the experiences of referring medical practitioners with medical imaging services and its implications for the Zambian healthcare system. These experiences are significant for radiology departments to improve the quality of medical imaging services.[6,18] The review findings can inform local medical imaging policy and practice in Zambia and beyond.
METHODS
A narrative literature review was conducted from July to December 2024 to answer the review question, “What are the experiences of referring medical practitioners with medical imaging services?”. This was developed based on the population, exposure and outcome (PEO) framework (Figure 1):[21,22]
Search strategy
The literature search was structured following the PEO framework to identify research studies conducted on the experiences of referring medical practitioners to medical imaging services. The search was performed via five databases: PubMed/MEDLINE, ScienceDirect, Scopus, Google Scholar, and Web of Science using five search terms: “experiences”, “medical practitioners”, “medical doctors”, “radiology services”, and “medical imaging services”. The search strategy involved combining search terms with Boolean operators “AND”, “OR”, and “NOT”. A free Google search and referencing lists were also conducted to supplement the database search and avoid missing relevant research studies.
Research studies focused on the experiences of referring medical practitioners with medical imaging services were deemed eligible for review. This includes qualitative, quantitative, and mixed-methods research. The publication date was restricted to research studies from January 2000 to December 2024. Since 2000, the delivery of medical imaging has changed following the introduction of digital radiography and associated Radiology Information Systems (RIS) and Picture Archiving and Communication Systems (PACS).[23,24] In addition, only research studies published in English were included. Reviews and commentary articles were excluded.
Study selection
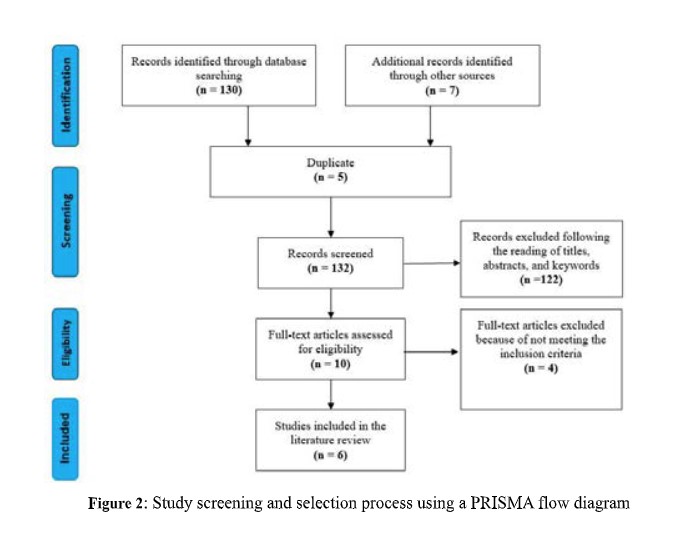
The two reviewers (OB and BC) dependably screened the titles, abstracts, and keywords to identify primary research studies that potentially met the inclusion criteria for this literature review. Disagreement between the two reviewers was resolved through the involvement of the third reviewer (NK). The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) framework was used to report the number of research studies identified, screened and selected for this review. The initial literature search yielded 137 records from both databases and other sources. After further screening, which included the removal of duplicates and records that did not meet the inclusion criteria, a total of six primary research studies 5 ,6 ,18,20,25,26] 5,6, 18, 20, 25, 26 were included in this review. Figure 2 shows the study selection process.
Data extraction and analysis
To avoid bias, data were extracted and analysed independently by two reviewers. Using the data extraction form, participants' quotes were extracted from qualitative studies, and descriptions of the experiences of medical practitioners with medical imaging services were obtained from quantitative studies. Other information extracted includes title, author details, year of publication, the aim of the study, study settings (country where the study was conducted) and main findings. The first (OB) and second reviewers (BC), all experienced in conducting narrative and systematic literature reviews, performed data analysis. The thematic analysis allowed the themes to emerge from the extracted data.[22,27,28] The themes were identified by reading and re-reading the extracted data.
Ethical considerations
No ethical approval was required as the reviewers used secondary public data. However, the reviewers eliminated bias by focusing on a single review question and describing all the processes involved in conducting this review. The first (OB) and second reviewers (BC) selected the studies and extracted and analysed the data to enhance the quality of the findings.
RESULTS
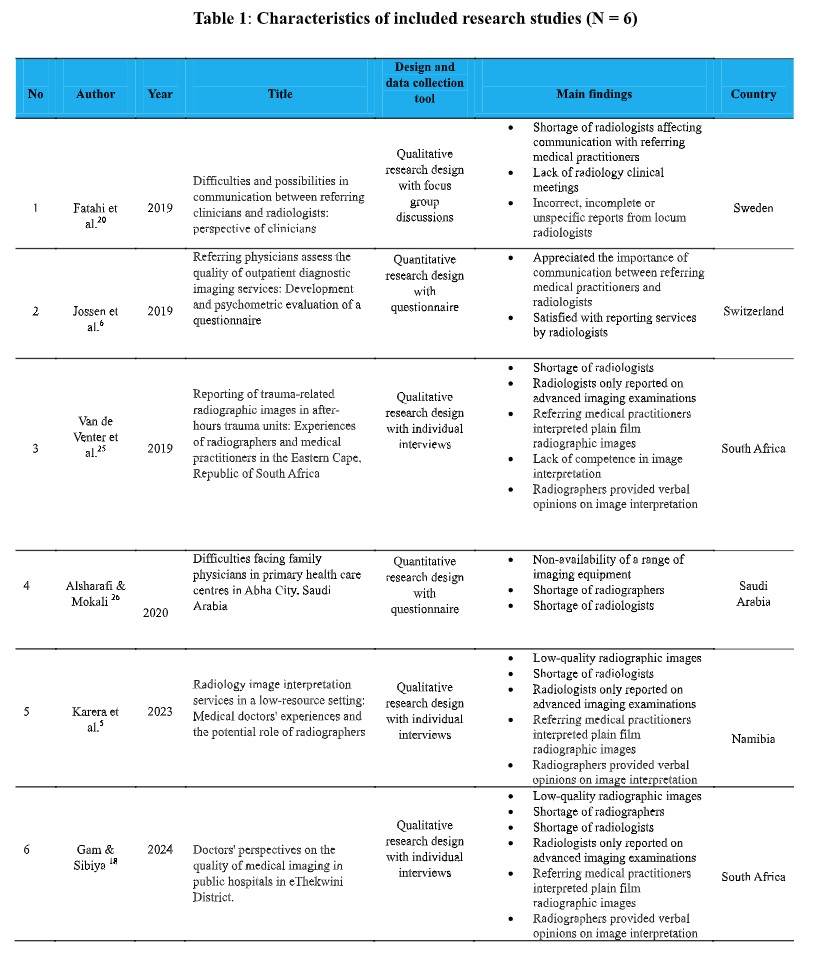
Description of included research studies Six research studies identified and included in this review were from South Africa (N=2), Namibia (N=1), Saudi Arabia (N=1), Switzerland (N=1), and Sweden (N=1). Four of the six research studies used qualitative[5,6,20,25] and two quantitative [6 ,26] research designs. Regarding data collection methods, one study [20] used focus group discussions (FGD), three studies [5,19,25] used individual semi-structured interviews and two studies [6,26] used a questionnaire. Other characteristics of the included research studies are shown in Table 1:
Themes
The data analysis for this review identified four thematic areas: medical imaging equipment and radiographic image quality, the shortage of imaging professionals, working relationships between referring medical practitioners and imaging professionals, and medical practitioners' interpretation of general radiographic images.
Medical imaging equipment and radiographic image quality
In a study conducted in Saudi Arabia, [26] the non-availability of a range of imaging equipment negatively affected the experiences of referring medical practitioners. No other study has reported on medical imaging equipment. Two research studies were conducted in Namibia [5] and South Africa, [19] emphasising the importance of producing high-quality radiographic images by radiographers to aid in diagnosing and treating patients. There were mixed experiences with the quality of the images. Some medical practitioners praised and were more satisfied with the quality of radiographic images in public hospitals than in private hospitals.[19] However, most medical practitioners complained that sometimes junior radiographers produced rotated, overexposed or underexposed images, making it difficult to interpret them.[5] Others were dissatisfied with the quality of images due to a lack of or incorrect image identification and imaging of unrequested body parts. [19] To overcome this challenge, referring medical practitioners suggested the supervision of inexperienced junior radiographers by their seniors.
Shortage of imaging professionals
The radiology department has two main imaging professionals: radiographers and radiologists. Two studies from Saudi Arabia [26] and South Africa [19] reported the impact of a shortage of radiographers on providing quality imaging services. Medical practitioners reported a shortage of radiographers, which resulted in a high workload for the available staff and long patient waiting times. This negatively affected their experience managing their patients and was identified as a significant contributing factor to poor service delivery. [19] To overcome this problem, medical practitioners suggested recruiting more radiographers, especially after hours when the demand for imaging does not match the available staff.
This review found that referring medical practitioners understood the role of radiologists in providing timely diagnostic imaging reports for decision-making, quality assurance and patient safety. [56,19,20,25] In a study conducted in Switzerland by Jossen et al.[6] referring medical practitioners were satisfied with reporting services by radiologists. The reports were on time, contained expected information, were clinically beneficial, answered the question asked by the referring medical practitioner and contained recommendations based on actual evidence for further investigations. However, three studies conducted in Namibia and South Africa reported a shortage of radiologists. [5,19,20] The Nambian study reported that it takes three months for a CT examination to be reported.[5] The shortage of radiologists was reported to affect communication and radiology clinical meetings where medical practitioners are taught about image interpretation.[20] However, some South African medical practitioners reported it unfair to expect one radiologist in the hospital to report on all medical imaging examinations. [19] For this reason, research studies from developing countries reported that radiologists only report on advanced imaging modalities such as CT and MRI, [5,19] while plain films images are interpreted by referring medical practitioners despite their limited training.
Working relationship between medical practitioners and imaging professionals
In the current review, three studies in Namibia [5] and South Africa [19,25] reported working relationships between referring medical practitioners and radiographers. In one study, 19 referring medical practitioners expressed concern about the lack of communication skills among radiographers. The main complaint was undertaking an examination not requested by the referring medical practitioners without discussing the request with them. This negatively affected the working relationships between the two professionals. However, in two studies, [5,25] referring medical practitioners were satisfied with working relationships with radiographers in providing verbal opinions on image interpretation when requested, especially after-hours when the radiologists are unavailable. The informal service provided by radiographers was reported as helpful in making a diagnosis.5 To overcome the shortage of radiologists, referring medical practitioners suggested extending the role of radiographers to include image reporting.
Two studies in Switzerland [6] and Sweden [20] reported the importance of communication between referring medical practitioners and radiologists. Although most referring medical practitioners were satisfied with the reporting system in their settings, few expressed concerns with incorrect, incomplete or unspecific reports from locum radiologists. [20] In the same Swedish study, another challenge was providing feedback to radiologists when the written diagnostic report conflicted with the medical practitioner's findings. Medical practitioners emphasised the importance of radiology conferences in improving the quality of imaging services. However, they reported a lack of time by both the medical practitioner and radiologists to provide and attend radiology educational sessions.
Medical practitioners’ interpretation of general radiographic images
In three studies conducted in Namibia [5] and South Africa, [19,25] referring medical practitioners were concerned about the unavailability of diagnostic imaging reports due to the critical shortage of radiologists. Unfortunately, this resulted in them interpreting plain film radiographic images themselves. Some medical practitioners reported struggling to interpret chest X-rays due to limited radiology training at medical school and a lack of continuous professional development (CPD) learning activities on image interpretation. [5] Some admitted their lack of competence in image interpretation.[25] Due to a shortage of radiologists and increased demand for advanced imaging examinations such as CT and MRI, radiologists only report on plain film radiographs upon special request from medical practitioners.5 These negatively affected their experiences with medical imaging services.
DISCUSSION
This study aimed to review the literature on the experiences of referring medical practitioners with medical imaging services and its implications for Zambia. The four themes identified were medical imaging equipment and radiographic image quality, the shortage of imaging professionals, working relationships between referring medical practitioners and imaging professionals, and medical practitioners' interpretation of general radiographic images.
This review identified a limited number of diagnostic imaging equipment as a factor negatively affecting medical practitioners and the delivery of quality healthcare services. This challenge mostly affects developing countries because of the high capital cost of medical imaging equipment.[29] For example, there is less than 1 CT scanner per million inhabitants in developing countries compared to 40 CT scanners per million inhabitants in developed countries.[30] In Zambia, there are 40 CT scanners, 8 MRI scanners, 16 mammographic units, 1 nuclear medicine scanner, and 2 dual-energy X-ray absorptiometry machines. Most of these advanced imaging services are in the two urban provinces of Lusaka and Copperbelt. However, the government has started installing advanced imaging equipment in the other eight provinces of Zambia. These advanced imaging modalities require specialised radiographers to operate them, radiologists to produce diagnostic reports, and medical physicists to ensure quality assurance (QA). Only five medical physicists work in Zambia and are responsible for QA for equipment in all 156 public hospitals nationwide. 31 Medical physicists apply both physics and medicine to assist healthcare professionals in diagnosing diseases and treating patients. To achieve the benefits of these advanced medical imaging modalities, there is a need to urgently look at the shortage of specialised radiographers, radiologists and medical physicists.
Although this review found a shortage of radiographers, Zambia has a moderate number of radiography workforce to serve a population of 19.6 million. In 2024, 908 radiography technologists/radiographers were registered with the Health Professions Council of Zambia (HPCZ). [32] The main challenge facing delivering quality medical imaging services is the shortage of specialised radiographers such as mammographers, sonographers, CT radiographers, and MRI radiographers. In addition, there is a shortage of radiologists in Zambia. [33-35] At the time of conducting this literature review,[22] radiologists were servicing a population of 19.6 million, giving a ratio of 1 radiologist to 890 people. This is a global problem, and developing countries are the most affected by it.[5] [19,25 36] In Africa, there is an average of 3.6 radiologists per one million people [37] compared with Europe, which has 13 radiologists per 100,000 people. [36]36 The shortage of radiologists affects not only the reporting service but also the training of medical students in image interpretation, as a few are overwhelmed with clinical and administrative duties.
The other factor identified in this review that affected referring medical practitioners' experiences is poor-quality radiographic images. Jossen et al. [6] noted that patients would not be referred to this service if a referring medical practitioner does not find a medical imaging service's technical and professional skills to be of good quality. Poor-quality radiographic images make interpreting difficult and lead to misdiagnosis. [5 ,19] The radiography training programmes have included radiographic image evaluation in Zambia. Immediately following image acquisition, the radiographer is responsible for reviewing the radiographic image to ensure it is of diagnostic quality before sending it to the radiologist or referring medical practitioner. [16 ,38] The image is reviewed using the “10-point plan”: patient identification, all areas of interest included, anatomical markers are present, correct projection, correct exposure indicator (EI), optimum definition, collimation, artefacts, any need for repeat or further projections, and any abnormality. [16] A recent literature review by Tonk et al. [38] revealed that radiographer image interpretation is a valuable strategy to optimise the quality of images. This is because radiographers understand the negative impact of poor-quality radiographic images on image interpretation. Another strategy to improve the quality of images is conducting periodical reject and repeat image analysis.39 This can be part of quality assurance programmes in the radiology department.
Our review found the communication and working relationships between imaging professionals and referring medical practitioners to be paramount in delivering quality services. Poor communication among health professionals has been identified as one of the primary causes of medical mistakes that adversely affect patient management. [20] In this review, some medical practitioners complained about poor communication skills among radiographers. Communication is exchanging information, thoughts, and feelings among people through speech or other means. [40]40 Two types of communication are used in the radiology department: written and verbal. [41 ,42] However, written communication is the most frequent communication between referring medical practitioners and imaging professionals. This includes the RRFs and diagnostic imaging reports. Therefore, imaging professionals are responsible for contacting the referring medical practitioner if the request is unjustified, the RRF is incomplete, or there are any issues related to the referral. This is why the name of the referring medical practitioner and contact number are included and completed on the RRF. 11,17 This communication enhances the working relationships between imaging professionals and referring medical practitioners.
This review found that image interpretation of general radiographic images in developing countries has been left to referring medical practitioners. Radiologists focus on reporting on complex imaging examinations such as CT and MRI and only report on general radiographic images upon special request. This practice has also been reported in the Zambian healthcare system. 33,35 The literature reports a lack of preparedness among medical students in image interpretation.[5,19,25 ,43] Due to the shortage of radiologists, responsibility for image interpretation is placed on inadequately trained medical practitioners, potentially resulting in misdiagnosis and mismanagement of patients. [5,33] To overcome this challenge, this review found the need to extend the scope of practice for radiographers to include image reporting. Image interpretation has been incorporated into the undergraduate radiography curriculum in the last decade. The aim is to help radiographers critically assess radiographic images for quality and provide verbal opinions on image interpretation when requested by referring medical practitioners. Our review found that in the absence of radiologists, referring medical practitioners consult radiographers on image interpretation. In a survey conducted in Zambia by Bwanga et al.[44] the majority (93%, N=76) of radiographers indicated offering verbal opinions on image interpretation when requested by referring medical practitioners. Establishing reporting radiographers has worked well in countries like the UK, Denmark, Australia and Uganda.
STRENGTHS AND LIMITATIONS OF THE STUDY
This narrative review has a few strengths and limitations. Firstly, the reviewers identified a well-focused review question using a PEO framework. This allowed other review aspects to flow directly from the question.[22,45] Secondly, the method included a clear aim with clearly stated inclusion and exclusion criteria, which provided transparency. Thirdly, a comprehensive and systematic literature search was conducted from different sources. This measure helped minimise the risk of study selections and publication bias.[22] Finally, study selection, data extraction and analysis were conducted by two reviewers. These measures increased the reliability and validity of the review findings.[22,45] However, there were also three notable limitations. Firstly, the scope of the review is limited, covering only five countries in the world: South Africa, Namibia, Saudi Arabia, Switzerland, and Sweden. Secondly, there were limited qualitative research studies that provided a deep understanding of the experiences of medical practitioners with medical imaging services. [22,46] The reviewers included quantitative research studies to increase the number of studies. Lastly, the search strategy excluded studies that were not published in English. This would have resulted in missing essential studies.
RECOMMENDATIONS FOR IMPROVEMENT
The following are recommendations on how this study's findings could be implemented in Zambia’s healthcare system and beyond:
- There is an increase in the number of advanced imaging services in Zambia. It is, therefore, recommended that more radiologists, clinical specialist radiographers, and medical physicists be recruited to improve the quality of medical imaging services. One of the possible solutions is to expand the enrolment of trainees in the recently introduced Specialised Training Programme (STP) in radiology in Zambia. In addition, postgraduate medical imaging programmes can be established to produce specialised radiographers in mammography, CT and MRI. This was also recommended in the review conducted by Bwanga et al.[47] on establishing postgraduate education and training in the specialised areas of diagnostic imaging in Zambia. Regarding medical physicists, Mulungushi University has introduced a bachelor’s degree in medical physics. There are also plans to introduce a bachelor’s degree in medical physics at the University of Zambia (UNZA).[31] This strategy will help to increase the number of medical physicists in the country.
- To enhance the working relationship between medical practitioners and imaging professionals, it is recommended that radiology clinical meetings be held, where issues such as radiographic image quality and the completion of RRFs can be discussed. These meetings can also include educational presentations.
- To fill the gap created due to the shortage of radiologists, it is recommended that the role of a radiographer be extended to include reporting on general radiographic images. Although the Ministry of Health in Zambia has recently introduced STP in radiology, it won't overcome the challenge of unreported radiographic images. Countries with more radiologists than Zambia, such as Uganda [N=80] [48] and the UK [N=4,000], [49] are still training and recruiting reporting radiographers. However, the main barriers are radiographers' limited scope of practice and possible resistance from radiologists. To overcome this, the Radiological Society of Zambia (RSZ) should intensify the advocacy and engagement of stakeholders on how reporting radiographers can improve the delivery of quality medical imaging services. This will require changes to the scope of practice for radiographers and the establishment of a postgraduate training programme in image interpretation and reporting.[33,35,48]
- There is a need to advocate for policy changes related to medical imaging, i.e., work with policymakers to address systemic issues affecting medical imaging services, including funding, resource allocation, and strategic planning in Zambian healthcare delivery.
- The reviewers suggest that research be conducted on the experiences of referring medical practitioners to medical imaging services in Zambia to gain a good understanding of the problem.
CONCLUSION
The review findings highlight significant challenges experienced by referring medical practitioners to medical imaging services. These included limited medical imaging equipment, poor radiographic image quality, a lack of diagnostic imaging reports, and poor communication between radiographers and referring medical practitioners. However, most of these challenges were identified in developing countries. The major challenge experienced by referring medical practitioners in managing and treating their patients in developing countries is a lack of diagnostic imaging reports due to a shortage of radiologists. It should be noted that the availability of a range of medical imaging equipment without enough radiologists to provide diagnostic reports compromises the quality of the imaging services. In developing countries such as Zambia, it is necessary to extend the scope of practice of radiographers to include reporting on general radiographic images. This will allow a few radiologists to focus on complex CT, MRI, and interventional radiology examinations. If implemented in Zambia and beyond, reporting radiographers and other recommendations made in this study can improve the quality of medical imaging services.
COMPETING INTEREST
The reviewers declare no conflict of interest.
REFERENCES
- Royal College of Radiologists and College of Radiographers. Standards for the education and training of reporting practitioners in musculoskeletal plain radiographs. London: RCR & COR; 2022.
- World Health Organization. To X-ray or not to X-ray; 2016. From https: //www. who.int/en/news-room/feature-stories/detail/to-x-ray-or-not-to-x-ray- (Assessed 10 October 2024)
- World Health Organization. Global initiative on radiation safety in healthcare settings. Geneva: WHO; 2008.
- Bwanga O, Nyanga I. Justification of imaging medical exposures: a review of literature to guide evidence-based practice in Zambia. Medical Journal of Zambia. 2020; 47(4): 318 - 326.DOI: https://doi.org/10.55320/mjz.47.4.129.
- Karera A, Engel-Hills P, Davidson F. Radiology image interpretation services in a low-resource setting: Medical doctors' experiences and the potential role of radiographers. Radiography. 2024;30(2):560-566. doi:10.1016/j.radi.2024.01.009
- Jossen M, Valeri F, Heilmaier C, Schwappach D. Referring physicians assess the quality of outpatient diagnostic imaging services: Development and psychometric evaluation of a questionnaire. Rofo. 2019;191(8):725-731. doi:10.1055/a-0805-1158
- Gadeka DD, Esena RK. Quality of care of medical imaging services at a Teaching Hospital in Ghana: Clients' perspective. J Med Imaging Radiat Sci. 2020a;51(1):154-164. doi:10.1016/j.jmir.2019.12.00
- Gadeka DD, Esena RK. Barriers to quality care in medical imaging at a Teaching Hospital in Ghana: Staff perspective. J Med Imaging Radiat Sci. 2020b;51(3):425-435. doi:10.1016/j.jmir.2020.05.002
- Tavakoli M, SeilanianToosi F, Saadatjou S. Knowledge of medical students on hazards of ionizing radiation. J Med Educ. 2003;3(1):3- 6.
- Kawooya MG, Kisembo HN, Remedios D, Malumba R, del Rosario Perez M, Ige T, et al. An Africa point of view on quality and safety in imaging. Insights into Imaging. 2022;13(1):1–10. doi: 10.1186/s13244-022-01203-w.
- Bwalya M, Bwanga O, Mvula JY, Munsanje F, Muntanga B. Adequacy of completion of radiology request forms at St. Francis' Hospital of Katete District: A clinical audit in Zambia. Malawi Med J. 2023;35(2):111-116. doi:10.4314/mmj.v35i2.7
- Nigatu AM, Yilma TM, Gezie LD. et al. Medical imaging consultation practices and challenges at public hospitals in the Amhara regional state, Northwest Ethiopia: a descriptive phenomenological study. BMC Health Serv Res. 2023:787 (2023). https://doi.org/10.1186/s12913-023-09652-9
- Ng'andwe EM, Bwanga O. Factors affecting the ability of radiographers to deliver imaging services in rural parts of Zambia. Radiography. 2022;28(3):758-765. doi:10.1016/j.radi.2022.03.005
- Republic of Zambia. Ionizing radiation protection act of 2011 (Amended). Lusaka: Government printers; 2011.
- Whitley AS, Jefferson G, Sloane KHC, Anderson G, Hoadley G. Clark’s positioning in radiography. 13th ed. London: CRC Press Ltd; 2015.
- Chanda E, Bwanga O, Sindaza N, Chipampe M, Chisha M. Audit of completion of computed tomography (CT) request forms at the Cancer Diseases Hospital (CDH) of Zambia. Medical Journal of Zambia. 2020; 47(4): 289 - 296. DOI: https://doi.org /10. 55320/mjz.47.4.122
- Gam NP, Sibiya MN. Doctors' perspectives on the quality of medical imaging in public hospitals in eThekwini District. Health SA. 2024;29:2389. Published 2024 May 7. doi:10.4102/hsag.v29i0.2389
- Mumenah SH, Al-Raddadi RM. Difficulties faced by family physicians in primary health care centers in Jeddah, Saudi Arabia. J Family Community Med. 2015;22(3):145-151. doi:10.4103/2230-8229.163027
- Fatahi N, Krupic F, Hellström M. Difficulties and possibilities in communication between referring clinicians and radiologists: perspective of clinicians. J Multidiscip Healthc. 2019;12:555-564. Published 2019 Jul 19. doi:10.2147/JMDH.S207649
- Munn Z, Stern C, Aromataris E, Lockwood C, Jordan Z. What kind of systematic review should I conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Med Res Methodol. 2018;18(1):5. Published 2018 Jan 10. doi:10.1186/s12874-017-0468-4
- Aveyard H, Payne S, Preston N. A post-graduates guide to doing a literature review in health and social care. London: Open University Press; 2021.
- International Atomic Energy Agency. Worldwide implementation of digital imaging in radiology. Vienna: IAEA; 2015.
- Kapapa N, Bwanga O, Sichone JM, Kafwimbi S, Ohene-Botwe B. Using a digital transformation framework to explore the experiences of radiographers in the use of digital radiography in a low-resource setting. Radiography. Published online November 13, 2024. doi:10.1016/j.radi.2024.10.024
- Van de Venter R, du Rand S, Grobler T. Reporting of trauma-related radiographic images in after-hours trauma units: Experiences of radiographers and medical practitioners in the Eastern Cape, Republic of South Africa. J Med Imaging Radiat Sci. 2017;48(2):128-136. doi:10.1016/j.jmir.2016.11.004
- Alsharafi HMA, Mokali BMK. Difficulties facing family physicians in primary health care centers in Abha City, Saudi Arabia. World Family Medicine. 2020; 18(10): 91-102 DOI: 10.5742/MEWFM.2020.93879
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008 Jul 10;8:45. doi: 10.1186/1471-2288-8-45. PMID: 18616818; PMCID: PMC2478656.
- Clark T, Foster L, Sloan L, Bryman A. Bryman’s social research methods (6th edition). Oxford: University Press; 2021.
- Hoe J. Quality service in radiology. Biomed Imaging Interv J. 2007;3(3) :e24. doi:10.2349/biij.3.3.e24
- Frija G, Blažić I, Frush DP, et al. How to improve access to medical imaging in low- and middle-income countries ?. EClinicalMedicine. 2021;38:101034. Published 2021 Jul 17. doi:10.1016/j.eclinm.2021.101034
- Bwanga O, Chanda E. Challenges in radiation protection in healthcare: A case of Zambia. EAS Journal of Radiology and Imaging Technology. 2020; 2(1):7-14.
- Chinene B, Mudadi LS, Bwanga O, et al. Sustainability in radiography: Knowledge, practices, and barriers among radiographers in Zimbabwe and Zambia. J Med Imaging Radiat Sci. 2024;55(3):101438. doi:10.1016/j.jmir.2024.101438
- Bwanga O, Mulenga J, Chanda E. Need for image reporting by radiographers in Zambia. Medical Journal of Zambia. 2019; 46(3): 215-220.DOI: https://doi.org/10 .55320/mjz.46.3.223
- Ministry of Health. National health strategic plan for Zambia 2022 to 2026. Lusaka: Ministry of Health; 2023.
- Chilambe E, Muller H, du Plessis J. Novel training approach to improve a cohort of radiographers' image interpretation skills of trauma chest radiographs. J Med Imaging Radiat Sci. 2024;55(2):244-257. doi:10.1016/j.jmir.2024.02.003
- Goh CXY, Ho FCH. The growing problem of radiologist shortages: perspectives from Singapore. Korean J Radiol. 2023;24(12):1176-1178. doi:10.3348/kjr.2023.0966
- Rosman DA, Bamporiki J, Stein-Wexler R, Harris RD. Developing diagnostic radiology training in low resource countries. Current Radiology Reports.2019; 7 (27): 1-8
- Tonks A, Jimenez Y, Gray F, Ekpo E. A stake in the game: Can radiographer image interpretation improve X-ray quality? A scoping review. Radiography (Lond). 2024;30(2):641-650. doi:10.1016/j.radi.2024.01.017
- Bwanga O. Causes of reject and repeat of digital radiographic images: a literature review to guide the practice of radiography in Zambia. Med J Zambia. 2020; 48 (1):38-45.
- Kourkouta L, Papathanasiou IV. Communication in nursing practice. Mater Sociomed. 2014;26(1):65-67. doi:10.5455/msm.2014.26.65-67.
- Vermeir P, Vandijck D, Degroote S, et al. Communication in healthcare: a narrative review of the literature and practical recommendations. Int J Clin Pract. 2015;69(11):1257-1267. doi:10.1111/ijcp.12686
- Ehrlich RA, Coakes DM. Patient care in radiography: with an introduction to medical imaging (10th ed). London: Elsevier; 2020.
- Chew C, Cannon P, O'Dwyer PJ. Radiology for medical students (1925-2018): an overview. BJR Open. 2020;2(1):20190050. Published 2020 Feb 4. doi:10.1259/bjro.20190050
- Bwanga O, Chanda E, Kafwimbi S, Sichone J. Opinions of Zambian radiographers on extending their role in the interpretation and reporting on general radiographic images: a cross-sectional survey. Medical Journal of Zambia. 2021; 48(3): 212 - 220.
- Bwanga O. How to conduct a qualitative systematic review to guide evidence-based practice in radiography. International Journal of Sciences: Basic and Applied Research. 2020; 52 (1): 205-213.
- Muchanga M. Critical approaches to research methodology and publishing. Lusaka: Gateway Publishers; 2024.
- Bwanga O, Mwansa E, Sichone J, Kafwimbi S. Establishment of postgraduate education and training in the specialised areas of diagnostic imaging in Zambia. African Journal of Health, Nursing and Midwifery.2020; 3(4):55-64.
- Mubuuke AG, Businge F, Kiguli-Malwadde E. Diagnostic accuracy of chest radiograph interpretation by graduate radiographers in Uganda. African Journal of Health Professions Education. 2019; 11(4):129-132.
- Royal College of Radiologists. The NHS does not have enough radiologists to keep patients safe, say three-in-four hospital imaging bosses: 2019. Available from: http: www.rcr.ac.uk/posts/nhs-does-not-have-enough-radiologists-keep-patients-safe-say-three-four-hospital-imaging (Accessed 10 December 2024).
Medical Journal of Zambia, Vol 51, 4
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.