Comparison of Manuka Honey Dressing versus Normal Saline Dressing on the outcome of Diabetic Foot Ulcers in Lahore, Pakistan
Muhammad Kashif Malik
Services Hospital, Services Institute of Medical Sciences Lahore Pakistan
Nauman Ismat Butt
Department of Medicine & Allied, Azra Naheed Medial College, Superior University Lahore Pakistan
Amin Mazhar Chaudhry
Services Hospital, Services Institute of Medical Sciences Lahore Pakistan
Syed Muhammad Bilal
Services Hospital, Services Institute of Medical Sciences Lahore Pakistan
Syed Zain Haider Kazmi
Services Hospital, Services Institute of Medical Sciences Lahore Pakistan
Haleema Amjad
Services Hospital, Services Institute of Medical Sciences Lahore Pakistan
Roshan Butt
Services Hospital, Services Institute of Medical Sciences Lahore Pakistan
DOI: https://doi.org/10.55320/mjz.51.4.606
Keywords:Diabetic Foot Ulcer, Manuka Honey Dressing, Normal Saline Dressing, Wagner Scoring System, Diabetes Mellitus.
ABSTRACT
Objective: Diabetic foot ulcers (DFUs) are common complications of diabetes, leading to infections and potential amputations. The Wagner Classification system is used to assess the severity of DFUs. Various dressing methods, including honey-impregnated dressings, have been explored for wound healing. However, high-quality research comparing honey dressings to conventional treatments is limited. This study aimed to compare the efficacy of Manuka honey-impregnated dressings with conventional saline dressings for DFUs, using the Wagner Classification.
Methodology: An observational cross-sectional study was conducted at Services Hospital Lahore from January 2023 to December 2023, with ethical approval. Diabetic patients aged 12-65 years with Grade 1 or 2 DFUs were included. A total of 90 patients were randomly assigned to two groups: Group A received Manuka honey dressings, and Group B received conventional saline dressings. After 4 weeks of follow-up, wound cultures were taken, and efficacy was determined based on the presence of bacterial growth. Data was analysed using SPSS, with a chi-square test for post-stratification.
Results: The honey dressing group showed a higher efficacy rate, with 44 (97.8%) patients achieving sterile cultures, compared to 37 (82.2%) in the saline dressing group (p = 0.014). Stratification analysis revealed the difference was significant in male patients.
Conclusion: Manuka honey dressings significantly improve the healing of diabetic foot ulcers compared to conventional saline dressings, particularly in male patients. Honey-impregnated dressings could be a valuable alternative for DFU management, promoting faster healing and reducing infection risk.
INTRODUCTION
Diabetes mellitus is a chronic disorder of metabolism. It is characterized by elevations in the level of blood glucose which may result from defects in insulin secretion, insulin action or both. Over an extended period of time, it leads to damage to both micro and macro vessels resulting in pathologies of the eyes, nerves, kidney, limbs, brain and heart. At present 422 million people mostly belonging to the low- and middle-income countries have diabetes with the number expected to rise. In Pakistan, WHO estimates that 15 % of the adult population is now expected by diabetes with more than 40,000 deaths every year due to it.[1]
Nearly 6% of the diabetics are affected by foot disease. It may manifest as infection, ulceration or necrosis. Diabetic foot disease may lead to disastrous consequences for the patient including loss of mobility, loss of livelihood and loss of limb; 1.5% of all diabetic foot patients end up in amputation.[2] Diabetic foot problems are responsible for nearly 50% of all diabetes related hospital bed-days.[3,4] According to International Diabetes Foundation data, there are 6.9 million diabetic patients in Pakistan with prevalence of 6.8% in adults while number of deaths due to diabetes amounted to 87,548.[5] Cost per person with diabetes is 52.7 US Dollars (USD), where most population belong to lower and middle socio-economic strata, so they are at risk of poor management owing to disease burden which further worsens once complications develop, like diabetic foot ulcers in 10-15% of diabetics.[6] These may lead to lower limb amputation and death in diabetic patients. Diabetic foot ulcers once developed are difficult to treat and multiple strategies have been used including nanocrystalline silver and honey[7] , negative pressure wound therapy in conjunction with collagenase ointment,[8] royal jelly[9] , berry-honey impregnated dressing[10] , silver dressing[11] , vacuum assisted closure[12] , leech therapy[4] , wireless micro-current stimulation [13] etc.
Honey has been used since the beginning of documented history. It has been shown to act against bacteria thereby preventing infection. Furthermore, resistance is usually not developed to honey.[14] Various wound classification systems are used with one of the most common ones being Wagner system. The Wagner system assesses ulcer depth and the presence of osteomyelitis or gangrene by using the following grades: grade 0 (pre-or post-ulcerative lesion), grade 1 (partial/full thickness ulcer), grade 2 (probing to tendon or capsule), grade 3 (deep with osteitis), grade 4 (partial foot gangrene), and grade 5 (whole foot gangrene).[15]
Although studies have examined the role of honey in wound healing but quality research on the clinical role of honey in the treatment of diabetic foot ulcers is limited. Furthermore, research on this subjected is hindered by problems of research on wound care, difficult in blinding and recruiting enough patients with similar pathology in adequate time. Therefore, we carried out a study on the effect of honey on diabetic foot ulcers. The rationale of this study is to compare the efficacy of honey impregnated dressings vs conventional dressing for management of diabetic foot ulcers making use of Wagner Classification to access both methods.
MATERIALS AND METHODS
We carried out an observational cross-sectional study in Department of Surgery, Unit 2, Services Hospital, Lahore after securing ethical approval from Institutional Review Board. The study period was from January 2023 to December 2023. Diabetic patients between ages of 12 to 65 years presenting with Diabetic foot ulcers were evaluated for inclusion in our study. Ulcers were classified according to Wagner Classification. Grade 1 and Grade 2 ulcers were included in our study. We excluded other grades from the study. Ninety patients presenting to Surgical OPD who fulfilled the inclusion criteria were included in the study. After taking informed consent, demographic variables (age, sex, gender, duration of symptoms, HbA1c and contact) were recorded. Wound debridement as required was done, after which the patients were randomly allocated into two groups A and B by using random number table.
In group A, patients received manuka honey impregnated dressings. In group B, patients received conventional dressing with normal saline. Patients were followed-up in OPD for 4 weeks at which time swab cultures were taken from all patients. A charcoal swab stick was used which was placed immediately after swabbing in Stuart’s transport medium and sent to the laboratory. If culture showed the cotton swabs to be sterile, then efficacy of dressing was labelled to be positive but if any aerobic or anaerobic growth was obtained it was labelled as negative. Complications if any were also recorded at follow-up visits.
Data was entered and analysed using SPSS version 23. Quantitative variables like age, duration of symptoms and HbA1c were presented as mean and SD. Qualitative variables like gender and efficacy were presented as frequency and percentage. Both groups were compared by using chi-square test. P-value ≤ 0.05 was taken as significant. Data was stratified for age, gender, duration of symptoms and HbA1c. Post-stratification, chi-square test was done by taking P-value ≤ 0.05 as significant.
RESULTS
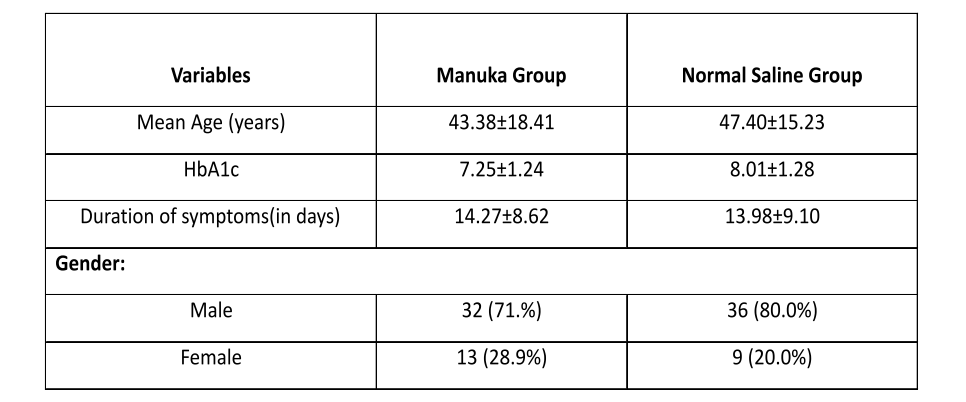
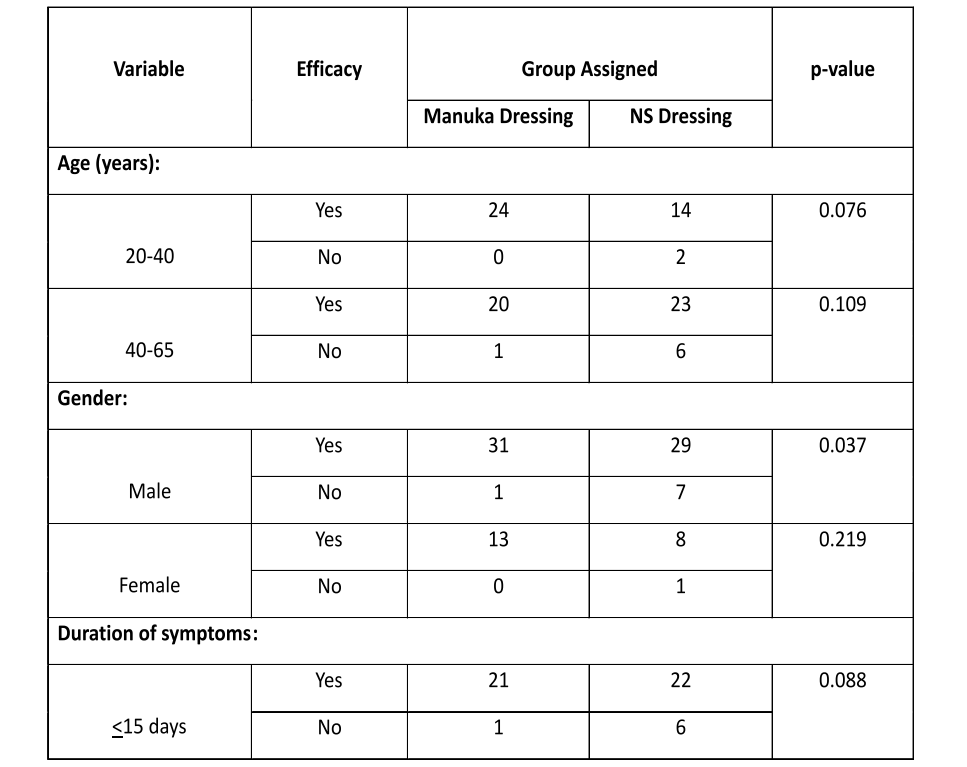
The mean age of patients was 43.38±18.41years in manuka honey group and 47.40±15.23years in conventional dressing group. Majority of patients in both groups were male. The duration of symptoms at presentation in both groups was similar. In manuka honey group, the mean HbA1c was 7.25±1.24% while it was slightly higher in conventional dressing group (HbA1c 8.00±1.28%) as shown in Table 1. Efficacy was seen in 44 (97.8%) cases in the honey group while in conventional dressing group, efficacy was achieved in 37 (82.2%) cases. This difference was significant (p 0.014) as demonstrated in Table 2. When stratifying was done it was only significant for gender as shown in Table 3.

DISCUSSION
Diabetes mellitus is an increasing global public health disease especially affecting the Asian population at an alarming rate causing significant poor quality of life, disease complications, morbidity and mortality.[16] In this study we compared the effect of manuka honey dressing and normal saline dressing on the management of diabetic foot ulcer. It was seen that manuka honey dressing led to a significant reduction in bacterial load as compared to normal saline dressing. Our results agree with those of previous studies and thus strengthen clinical evidence for increased use of honey dressing for diabetic foot ulcer. It was shown that the application of manuka honey was associated with clearance of the bacteria from the diabetic ulcer. This should lead to a reduction in the need for hospitalization and antibiotic use. Similar effect has also been noted by other researchers.[17] Honey is being used to treat many types of wounds. However as discussed before the results of the studies are variable with high powered trails wanting.[18,24] In our study it was seen that in the manuka honey group, efficacy was achieved in 44 (97.8%) cases while in conventional dressing group, efficacy was achieved in 37 (82.2%) cases The difference was significant (p<0.05). Kamaratos et al., reported that the efficacy was achieved in 100% cases with Manuka honey impregnated dressings while 87.1% with conventional dressing in the treatment of diabetic foot ulcers within 4weeks of treatment. The difference was significant (P<0.05).[14] Similarly in a study of 30 infected diabetic foot wounds by Moghazy which made use of honey dressings for three months. Healing was achieved in 43.3% ulcers while another 43.3% showed decrease in size and granulation. Almost all ulcers showed a reduction in the bacterial load.[19] 6 patients with infected diabetic ulcer was treated by honey-based products and evaluated for their outcomes by Harikrishna. Infections were rapidly resolved without need for antibiotics.[20] These findings corroborate the findings of our study.
The mean age of patients was 43.38±18.41 years in manuka honey group and 47.40±15.23 years in conventional dressing group. Similar findings were also noted by other researchers who also noted that most patients of diabetic foot ulcers belonged to 4th and 5th decade of life.[21,22] Data was stratified for age of patients. The difference was insignificant (p>0.05). Data was stratified for gender of patients. Majority of the patients in our study were male. Other researchers also found that male gender had a preponderance for diabetic foot ulcers.[22,23] In male patients, efficacy was achieved in 31 (96.9%) cases with manuka honey while in 29 (80.6%) cases with conventional dressing. The difference was significant (p<0.05). The difference was insignificant (p>0.05) for females. When data was stratified for duration of symptoms, no significant difference was seen between the two groups. Similarly, when stratification was done for mean HbA1c there was no difference between the two groups (p > 0.05). There were no complications in either group.
The main limitations of our study include a small sample size, the inclusion of only Wagner Grade 1 and 2 ulcers, and the single-centre nature of the research, which may limit the generalizability of the findings. Additionally, the short 4-week follow-up period restricts our ability to assess the long-term effects of honey dressings, and the challenge of blinding in wound care studies could have introduced observer bias. Despite these limitations, our study has several strengths, including a randomized controlled design, standardized assessment using the Wagner Classification, and clear inclusion/exclusion criteria, which ensure a more accurate comparison between honey-impregnated and conventional saline dressings. To address these limitations, further research with larger, multi-centre trials and longer follow-up periods is recommended to confirm the long-term efficacy of honey dressings. Future studies should also include patients with more severe ulcers (Wagner Grade 3 and above) and explore objective measures such as histological wound healing and quality of life outcomes. Additionally, investigating the underlying mechanisms of honey's effectiveness could provide valuable insights into its clinical applications for diabetic foot ulcers.
CONCLUSION
In conclusion, our study indicates that Manuka honey-impregnated dressings significantly improve the healing outcomes of diabetic foot ulcers compared to conventional saline dressings. The honey dressings were more effective in promoting wound healing, as evidenced by a higher percentage of patients achieving sterile cultures at follow-up. These findings suggest that Manuka honey may offer a promising alternative to conventional wound care, particularly for diabetic foot ulcer patients. However, further research with larger sample sizes, longer follow-up periods, and multi-centre trials is needed to confirm the long-term efficacy and generalizability of this treatment. Additionally, exploring the mechanisms underlying honey's healing properties could further enhance its clinical application in managing diabetic foot ulcers.
REFERENCES
- World Health Organization. Diabetes [Internet]. Geneva: World Health Organization; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/diabetes.
- Mishra SC, Chhatbar KC, Kashikar A, Mehndiratta A. Diabetic foot. BMJ. 2017;359: j5064. Doi: 10.1136/bmj. j5064.
- Ahmad J. The diabetic foot. Diabetes Metab Syndr. 2016;10(1):48-60. doi: 10.1016/j.dsx.2015.04.002.
- Zaidi SM. Unani treatment and leech therapy saved the diabetic foot of a patient from amputation. Int Wound J. 2016;13(2):263-4. doi: 10.1111/iwj.12285.
- International Diabetes Federation. Pakistan [Internet]. 2015. Available from: http://www.idf.org/membership/mena/pakistan.
- Schwartz SI, Brunicardi FC. Schwartz's principles of surgery: ABSITE and board review. New York: McGraw-Hill Medical; 2011.
- Tsang KK, Kwong EW, Woo KY, To TS, Chung JW, Wong TK. The Anti-Inflammatory and Antibacterial Action of Nanocrystalline Silver and Manuka Honey on the Molecular Alternation of Diabetic Foot Ulcer: A Comprehensive Literature Review. Evid Based Complement Alternat Med. 2015; 2015:218283. doi: 10.1155/2015/218283.
- Stryja J, Staffa R, Říha D, Stryjová K, Nicielniková K. Cost-effectiveness of negative pressure wound therapy in outpatient setting. Rozhl Chir. 2015;94(8):322-8.
- Miller JD, Carter E, Hatch DC, Zhubrak M, Giovinco NA, Armstrong DG. Use of collagenase ointment in conjunction with negative pressure wound therapy in the care of diabetic wounds: a case series of six patients. Diabet Foot Ankle. 2015; 6:24999. doi: 10.3402/dfa. v6.24999.
- Siavash M, Shokri S, Haghighi S, Shahtalebi MA, Farajzadehgan Z. The efficacy of topical royal jelly on healing of diabetic foot ulcers: a double-blind placebo-controlled clinical trial. Int Wound J. 2015;12(2):137-42. doi: 10.1111/iwj.12063.
- Imran M, Hussain MB, Baig M. A Randomized, Controlled Clinical Trial of Honey-Impregnated Dressing for Treating Diabetic Foot Ulcer. J Coll Physicians Surg Pak. 2015;25(10):721-5. doi: 10.2015/JCPSP.721725.
- Günal Ö, Tuncel U, Turan A, Barut S, Kostakoglu N. The Use of Vacuum-Assisted Closure and GranuFoam Silver® Dressing in the Management of Diabetic Foot Ulcer. Surg Infect (Larchmt). 2015;16(5):558-65. doi: 10.1089/sur.2014.093.
- Wirsing PG, Habrom AD, Zehnder TM, Friedli S, Blatti M. Wireless micro current stimulation--an innovative electrical stimulation method for the treatment of patients with leg and diabetic foot ulcers. Int Wound J. 2015;12(6):693-8. doi: 10.1111/iwj.12204.
- Kamaratos AV, Tzirogiannis KN, Iraklianou SA, Panoutsopoulos GI, Kanellos IE, Melidonis AI. Manuka honey-impregnated dressings in the treatment of neuropathic diabetic foot ulcers. Int Wound J. 2014;11(3):259-63. doi: 10.1111/j.1742-481X.2012.01082. x.
- Oyibo SO, Jude EB, Tarawneh I, Nguyen HC, Harkless LB, Boulton AJ. A comparison of two diabetic foot ulcer classification systems: the Wagner and the University of Texas wound classification systems. Diabetes Care. 2001;24(1):84-8. doi: 10.2337/diacare.24.1.84.
- Butt NI, Ghoauri MSA, Waris U, Sabeh D, Qaisar F. Frequency of Restless Legs Syndrome in Pakistani Patients with Type 2 Diabetes Mellitus. Cureus. 2024;16(6): e62624. doi: 10.7759/cureus.62624.
- Minden-Birkenmaier BA, Bowlin GL. Honey-Based Templates in Wound Healing and Tissue Engineering. Bioengineering (Basel). 2018;5(2):46. doi: 10.3390/bioengineering5020046.
- Labban L. Honey as a promising treatment for diabetic foot ulcers (DFU). J Med Soc. 2014;28(2):64.
- Moghazy AM, Shams ME, Adly OA, Abbas AH, El-Badawy MA, Elsakka DM, et al. The clinical and cost effectiveness of bee honey dressing in the treatment of diabetic foot ulcers. Diabetes Res Clin Pract. 2010;89(3):276-81. doi: 10.1016/j.diabres.2010.05.021.
- Nair HKR, Tatavilis N, Pospíšilová I, Kučerová J, Cremers NAJ. Medical-Grade Honey Kills Antibiotic-Resistant Bacteria and Prevents Amputation in Diabetics with Infected Ulcers: A Prospective Case Series. Antibiotics (Basel). 2020;9(9):529. doi: 10.3390/antibiotics9090529.
- Makhdoom A, Khan MS, Lagahari MA, Rahopoto MQ, Tahir SM, Siddiqui KA. Management of diabetic foot by natural honey. J Ayub Med Coll Abbottabad. 2009;21(1):103-5.
- Jan WA, Shah H, Khan M, Fayaz M, Ullah N. Comparison of conventional pyodine dressing with honey dressing for the treatment of diabetic foot ulcers. J Postgrad Med Inst. 2012;26(4):402-7.
- Dos Santos Tavares DM, Dias FA, Araújo LR, Pereira GA. Perfil de clientes submetidos a amputações relacionadas ao diabetes mellitus [Profile of patients submitted to amputation related to diabetes mellitus]. Rev Bras Enferm. 2009;62(6):825-30. Portuguese. doi: 10.1590/s0034-71672009000600004.
- Asamoah B, Ochieng BMN, Meetoo D. The clinical role of honey in treating diabetic foot ulcers: a review. Diabet Foot J. 2014; 17:25–8.
Medical Journal of Zambia, Vol 51, 4
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.