Battered Baby Syndrome: a good medico-legal denouement
K Saasa
Principal General Practitioner
MSS Patel
Chief Forensic Pathologist
DOI: https://doi.org/10.55320/mjz.51.4.579
Keywords:battered baby, shaken baby syndrome, syndrome of child abuse and neglect, non-accidental trauma, forensic pathology, medical jurisprudence, National Forensic Act 2020, Children's Code Act 2022
ABSTRACT
A long case of fatal battered baby syndrome is discussed. The objectives are to emphasise the diagnostic challenges in child abuse cases and to recommend adherence to the provisions of the law relating to children's welfare in Zambia. The syndrome is classed under the category of a less emotive 'syndrome of child abuse and neglect' or 'non-accidental trauma' in children. There are many variations of maltreatment of children, and child cruelty is a major medico-social problem. There are characteristic features of the syndrome, but clinical findings can be variable. A considerable diagnostic challenge is posed by conflicting clinical opinions. Children sustain unintentional bruises during abrasive playtime, and they must be differentiated from non-accidental trauma. Medical opinions of expert witness are often tested in a court of law to preserve factual evidence. A guilty verdict based on unsafe clinical opinions can be detrimental to good practice in forensic medicine. A careful collation of all evidential pieces may complete a forensic jig-saw puzzle. A good medico-legal denouement is recognised when there is incontestable medical evidence of guilt and and it is backed up by a self-confession of the accused.
Zambia is not immune from the global pandemic of corporal punishment administered to children at home or school. Child welfare in Zambia is legislated under the Children's Code Act 2022 and provides for reforms and consolidation of the laws relating to children. It includes parental responsibility and protection of children, as well as prosecution of culpable offenders. The forensic pathology service in Zambia has been transformed under the National Forensic Act 2020. It provides for the regulation of the practice of forensic pathology and allied science. The Act establishes the National Forensic Authority, the Office of the State Forensic Pathologist and the National Forensic Science and Biometric Department and provides for their function and connected matters. It includes standardization of the performance of medico-legal death investigation and licensing of forensic service providers. All sudden and unexpected or unnatural deaths or when a medical certificate of the cause of death [MCCD] cannot be issued, ought to be referred for thanatopsy in accordance with the National Forensic Act 2020.
INTRODUCTION
An undergraduate course in forensic medicine was first introduced in the School of Medicine at UNZA (University of Zambia) by Dr Sashi Gore, consultant histopathologist based at University Teaching Hospital (UTH) in Lusaka, circa 1970. The first State Forensic Pathologist (SFP) in Zambia was Dr Nat Patel who was seconded from the department of Forensic Medicine at the Royal London Hospital and occupied an office at UTH.
The forensic pathology service in Zambia has since been transformed by the National Forensic Act 2020 [NFA] enacted by Parliament of Zambia. It replaced the coroner system under the Inquest Act 1939. The NFA establishes the National Forensic Authority in Part II, National Forensic Authority under s. 3; the Office of the State Forensic Pathologist (OSFP) in Part V, OSFP under s. 24, and the National Forensic Science and Biometric Department in Part VI, National Forensic Science and Biometric Department under s. 27 with provision for their functions and connected matters in s. 4, 26, 28 respectively. The Act has regulated the practice of forensic pathology and allied forensic science. The forensic service providers are licensed, and the performance of medico-legal death investigation [MLDI] is standardized. MLDI has ushered in public accountability under a legal system for forensic pathologists and allied scientists, which should prevent miscarriage of justice in suspicious deaths and homicides.[1]
Medical jurisprudence is about clinical and pathological medico-legal investigations. There is no legal definition of a medico-legal death. A cause of death is an informed opinion and not a medical fact.
A multidisciplinary involvement of sub-specialities in forensic medicine such as psychiatry, neuropathology, cardiopathology, paediatric pathology, histopathology, odontology, radiology is permitted by the NFA in Part V, OSFP, under s. 26.
A collaboration with a wide range of ancillary forensic laboratory investigations such as toxicology, entomology, serology, haematology, DNA (deoxyribonucleic acid) 'finger printing', ballistics, photography is provided for by the NFA in Part VI, National Forensic Service and Biometric Department under s. 28-29. A licensed forensic pathologist would gather the evidence gleaned from thanatopsy and submit the forensic exhibits to the State Forensic Analyst (SFA) as in Part V, OSFP under s. 26. The SFA is responsible for the collection, packaging, preservation and custody chain as in Part VI, National Forensic Science and Biometric Department under s. 28. An additional duty of the SFA is to provide for the management of a crime scene. All evidential pieces are carefully collated like jig-saw pieces to complete a medico-legal puzzle.
Medical evidence produced for the prosecution by the forensic pathologist acting as an expert witness will often be challenged in a court of law. This is expected from the defence counsel guided by a medical report produced by the defence expert witness. It is a built-in legal mechanism for the quality assurance of factual evidence in the administration of justice. Lawyers, forensic pathologist and scientists, the police and parliamentarians are now aware that criminal proceedings can go badly wrong if sensible question are not asked by Counsels, and careful answers not given by expert witnesses.[2]
A side-effect of an adversarial judicial litigation as opposed to an inquisitorial type is the risk that the whole truth may get buried deep within the admissible evidence. Medical witnesses may stray outside the limit of expertise, or misfit a biased diagnosis to clinical signs and symptoms. Some jurors may be swayed enough to tip the scales of justice by the witness box performance of a charismatic medical expert. The muchness of a congregation of medical witnesses counteracting less popular evidence based medical opinions may impart a similar effect on the jurors. The judge can use the prerogative to rebuke an expert witness and instruct the jury to disregard expert opinions which are misleading or based on medical uncertainties. The NFA makes it a criminal offence to submit a false or misleading report or withhold materially factual information in Part VII, General Provision under s. 31.
The Children's Code Act 2022 [CCA] legislates for child welfare in Zambia. It has reformed and consolidated the laws governing children by providing for parental responsibility and care and protection of minors. A child is entitled to protection from maltreatment and any other form of exploitation in Part II, The Rights and Responsibility of Child under s. 17. It also prohibits corporal punishment of children as well as subjecting a child to torture and cruel treatment under s. 22-23 respectively. There is added provision for prosecution of culpable offenders. The health care providers have an obligatory role in protecting children in accordance with the CCA.
CASE REPORT
Clinical history:
A female infant aged 9 months was an unwanted baby and put into foster care. She was reported to be doing well apart from some difficulty in feeding. She appeared to have retarded developmental milestones but otherwise all investigations were unremarkable. She was later returned to her mother with close involvement of the social worker. The parents continued to find her difficult to feed.
A fortnight prior to her death she was noticed to have lost weight. The health visitor recorded a loss of 100g and had observed that there were no signs of maltreatment. About forty-eight hours thereafter she became unwell and the following day she had become drowsy and seriously ill. She collapsed with twitching and her mother sought urgent medical attention. The mother had witnessed the father slap the baby and throw her against a soft sofa for refusing her feed.
She was rushed to hospital in a state of shock. A provisional diagnosis was an overwhelming infection, possibly meningococcal meningitis. She was moderately dehydrated and received blood transfusion and antibiotic (Cefuroxime and Gentamicin), whereupon her condition improved slightly. She suffered left sided seizure which was treated with anticonvulsant (Phenytoin) and sedative (Diazepam) drugs. She developed apnoea and was transferred to an intensive care unit at a children's hospital and put on an intermittent positive pressure ventilator.
She was extremely unwell with a gallop rhythmic tachycardia, blood pressure 80/30 mmHg and hypothermia 35oC. She was hypotonic in all limbs with no elicitable reflexes. Her pupils were equally dilated and unreactive. The anterior fontanelle was bulging. Her chest and abdomen were clinically normal. Bruising was noted on her limbs and lower back.
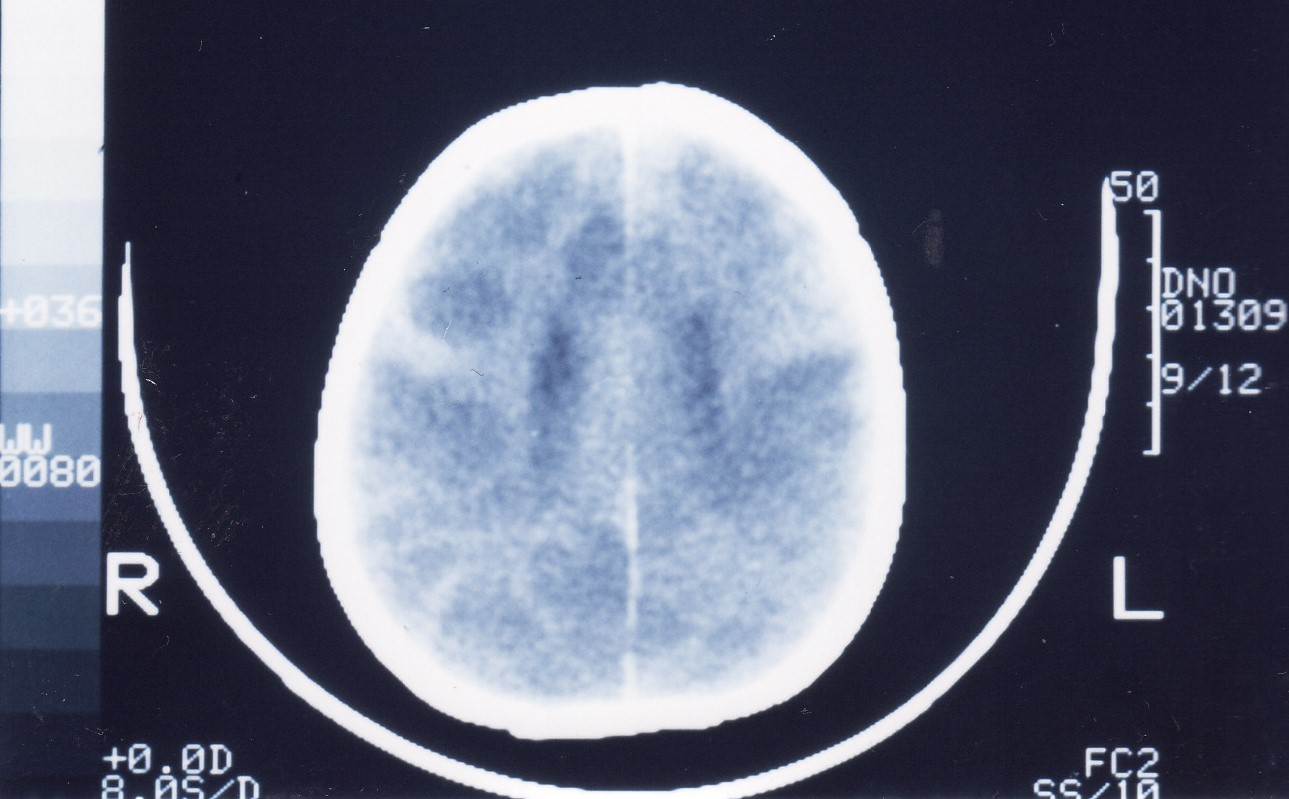
Ophthalmoscopy revealed left retinal and right subhyaloid haemorrhages. A full skeletal x-ray survey showed no abnormality. An enhanced computed tomography scan of the brain showed bilateral low density grey and white matter due to raised intracranial pressure [Figure 1]. There was no detectable subdural haemorrhage.
Hospital laboratory investigations showed normal biochemical and haematological parameters apart from raised white cell count 28.8 (neutrophils 23) x109/l. A bacteriological examination of cerebrospinal fluid obtained by a ventricular tap was normal, and meningitis could be ruled out.
She was hyperventilated overnight, and her fluid intake was restricted, Her anticonvulsant and antibiotics drug were continued. She suffered multiple seizures. Electroencephalogram (EEG) showed phasic cerebral activity. By next post-admission day, she developed irreversible cerebral function loss. EEG recorded a flat line and there were absent doll's eye movement, corneal reflex, and gag or cough reflex and a negative response to caloric stimulation and apnoea test. She was declared brain dead after the brain stem examination.
Thanatopsy:
- External examination essentially showed a well-nourished and generally well-cared for baby girl dressed in a hospital shroud. The eyes were of normal appearance.
- She weighed 5.7Kg having lost 250g since last checked by the health visitor. Other anthropometric indices were head circumference 43cm in 10th percentile; crown-heel length 63cm and crown-rump length 38cm below 3rd percentile.
- Marks of recent injury consisted of resolving brownish-yellow grip-type bruise and a faint horizontal bruise around the upper right elbow; three parallel resolving brownish-yellow grip-type bruises on the inner aspect of mid right forearm; minor bruises around the back of right wrist associated with overlapping several fingernail marks; a resolving diffused yellowish-blue grip-type bruise above a brownish-yellow bruise with three parallel faint marks on the outer aspect of right thigh; an intradermal small resolving brownish-yellow bruise on right buttock and yellowish-blue bruise in para-midline left lower and mid-back. There were no signs of recurrent injuries. There were numerous hospital therapeutic marks which included multiple needle marks around the anterior fontanelle. A postmortem skeletal survey in child abuse cases constitutes an appropriate investigation related to the cause of death as provided for by NFA in Part V, OSFP under s.26. It was deemed not necessary as the antemortem hospital x-rays revealed no fractures or congenital abnormality.
- Systemic examination showed the anterior fontanelle was bulging and tense. There was a massive right subdural haemorrhage with a 5mm thick layer of dark red blood clot adherent to the dura [Figures 2-3].
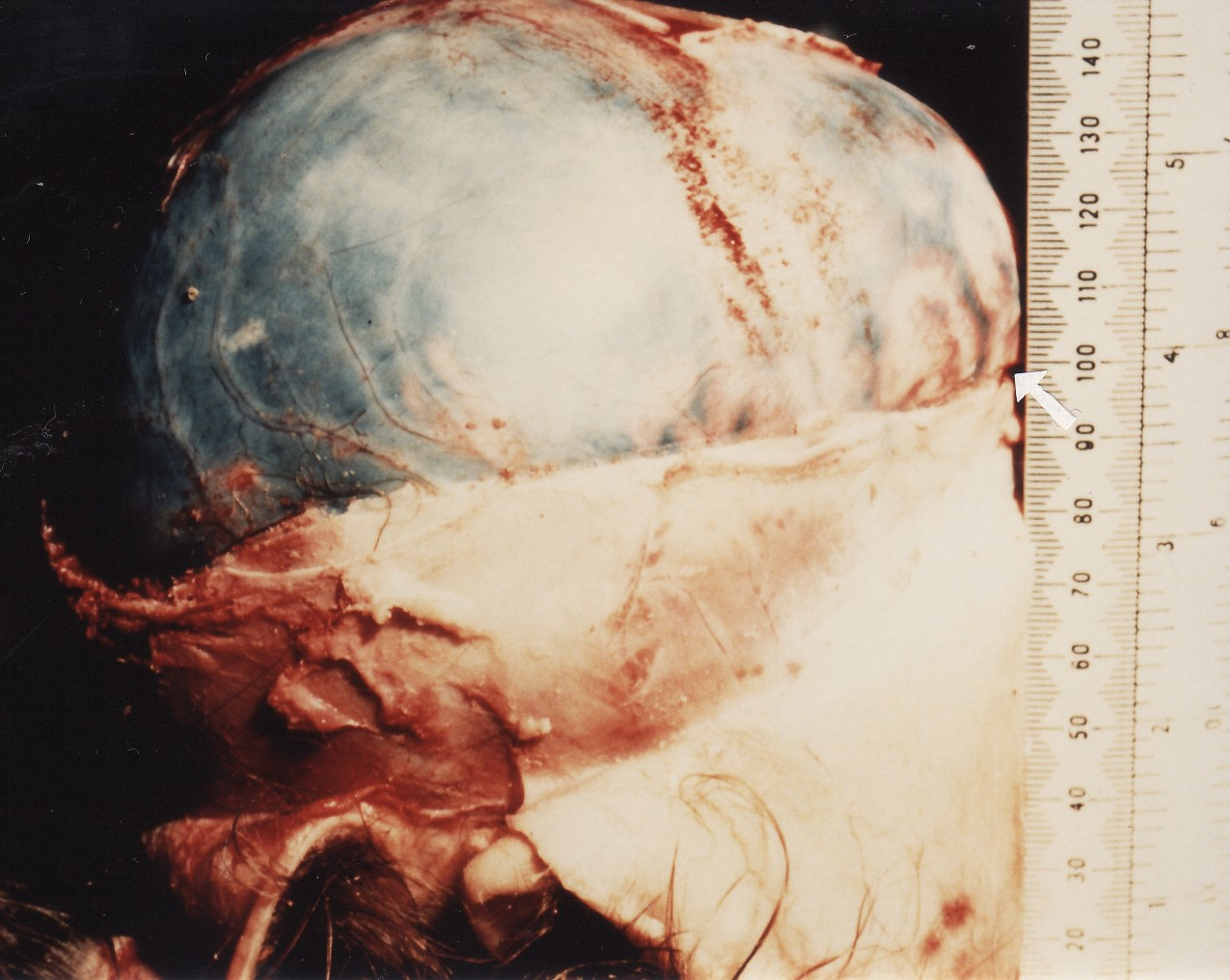
Fig 2. Subdural haematoma with cerebral overflow (arrowed) from intracranial pressure 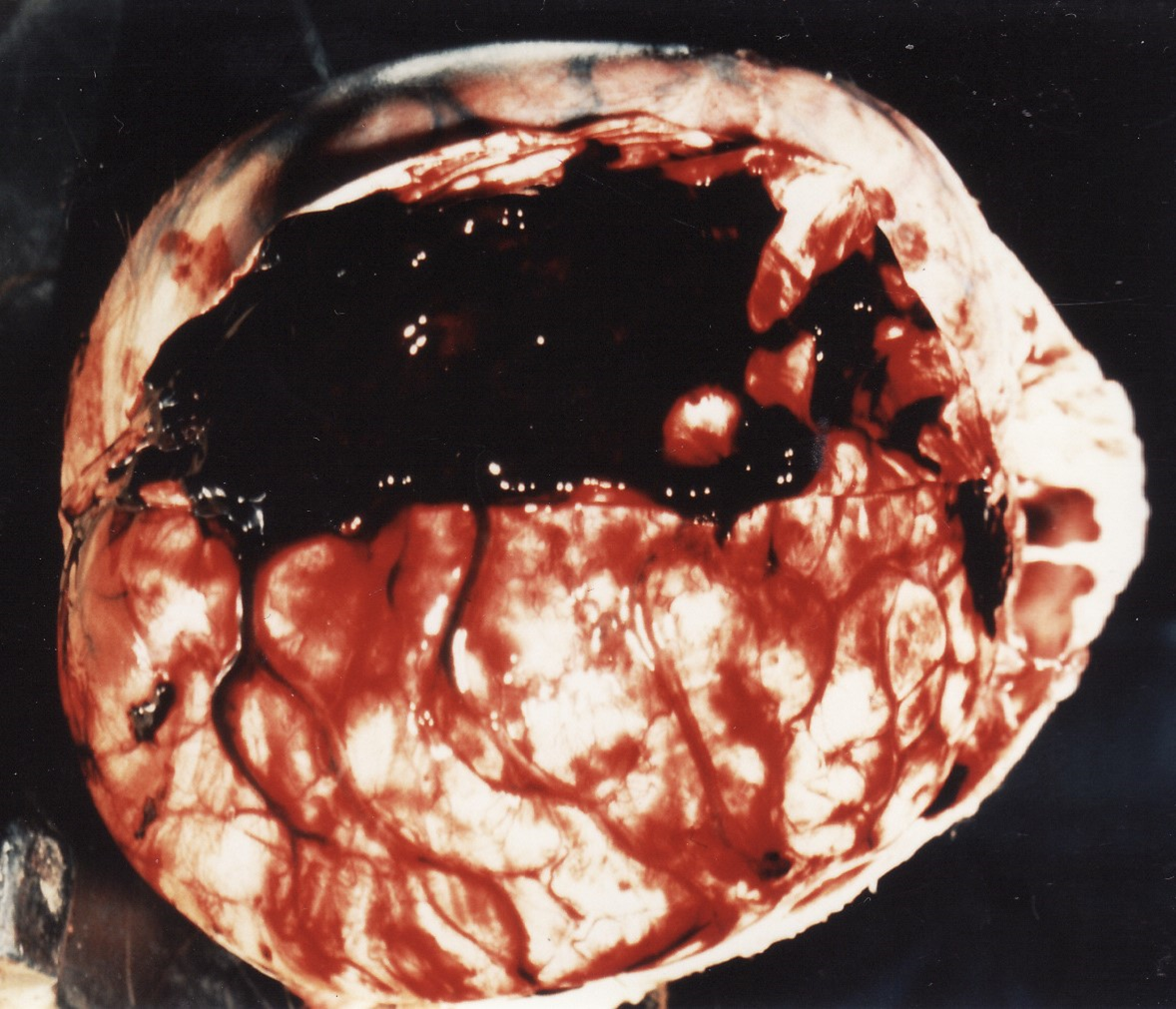
Fig. 3 Subdural haematoma adherent to dural flap Leptomeninges were congested and showed no sign of sepsis. Cerebral hemispheres were grossly oedematous and showed flattened gyri and obliterated sulci due to raised intracranial pressure. Falx cerebri, cerebellar tentorium and brain stem were normal. The vascular sinuses were unremarkable and superior sagittal sinus was devoid of antemortem thrombus. Brain weighed 950g. The brain and both eyes were retained for further examination as provided for by NFA in Part V, OSFP under s.26.
The cardiovascular, respiratory, alimentary, urogenital, lymphoreticular, endocrine and musculoskeletal systems were unremarkable apart from atelectatic lower pulmonary lobes. There was no trauma of the viscera and no bone fractures.
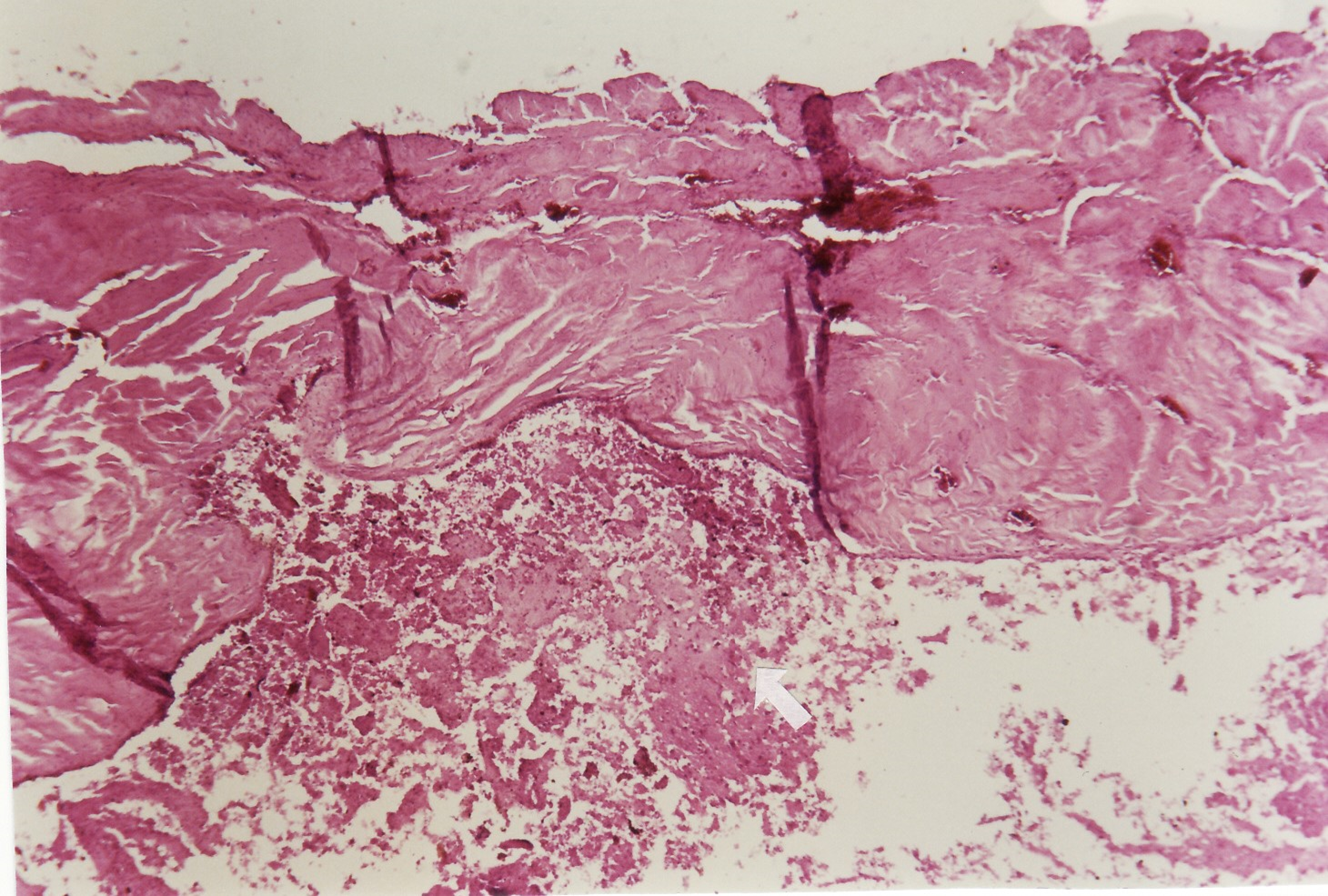
- The formaldehyde-fixed brain confirmed the subacute subdural haematoma (SDH) and showed a minor yellowish cortical contusion on the right occipital lobe and a smaller brownish contusion on the cortex of right occipital lobe and postero-inferiorly over the left cerebellum. Further dissection showed localised supracallosal haematoma associated with several iatrogenic needle track haemorrhages in the parietal lobes and directed towards the lateral ventricles [Figure 4]. There were punctate haemorrhages in the internal capsule of left striatum.

Fig. 4 Formaldehyde-fixed brain hemisections with supracallosal (arrowed) haematoma The hemisection of the eyes fixed in formalin showed left retinal and right subhyaloid haemorrhages which were confirmed by microscopy, and minor left perineural haemorrhage and right retroscleral haemorrhage with intraocular haemorrhages [Figures 5-8].
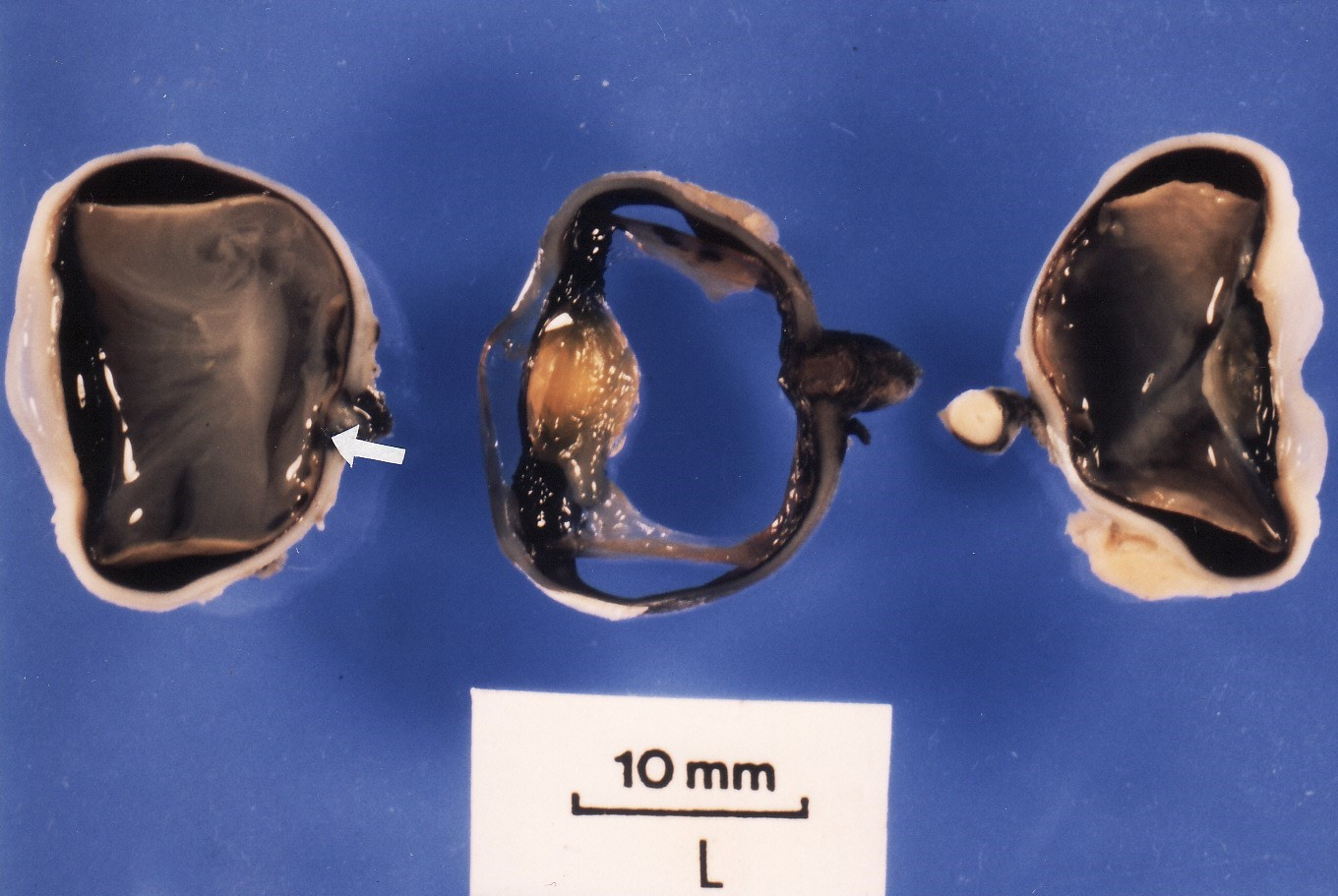
Fig 5. Formaldehyde-fixed eyeball trisection with retinal (arrowed) haemorrhage 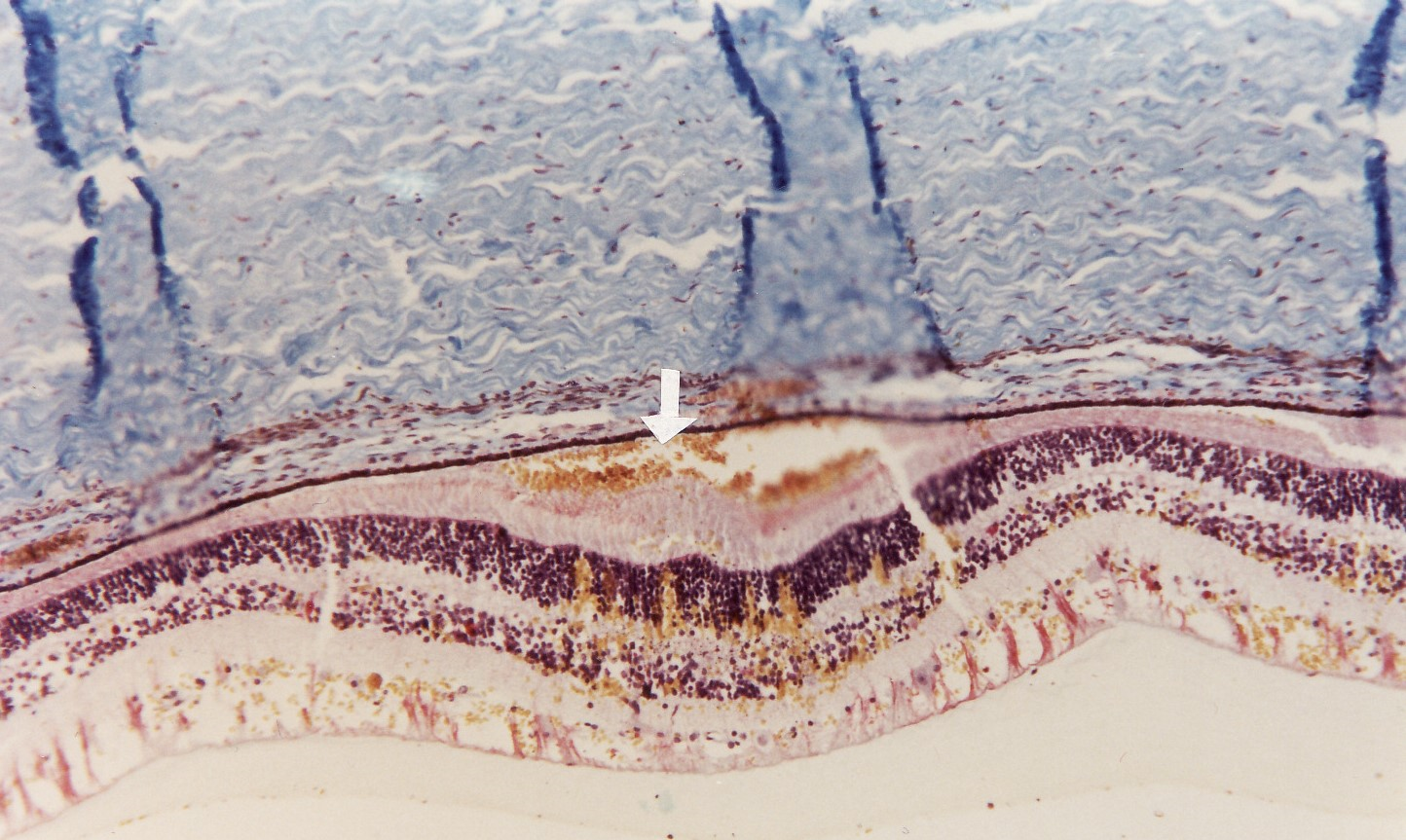
Fig 6. Micrograph of left eye with retinal (arrowed) haemorrhage (Acid Fuchsine x100) 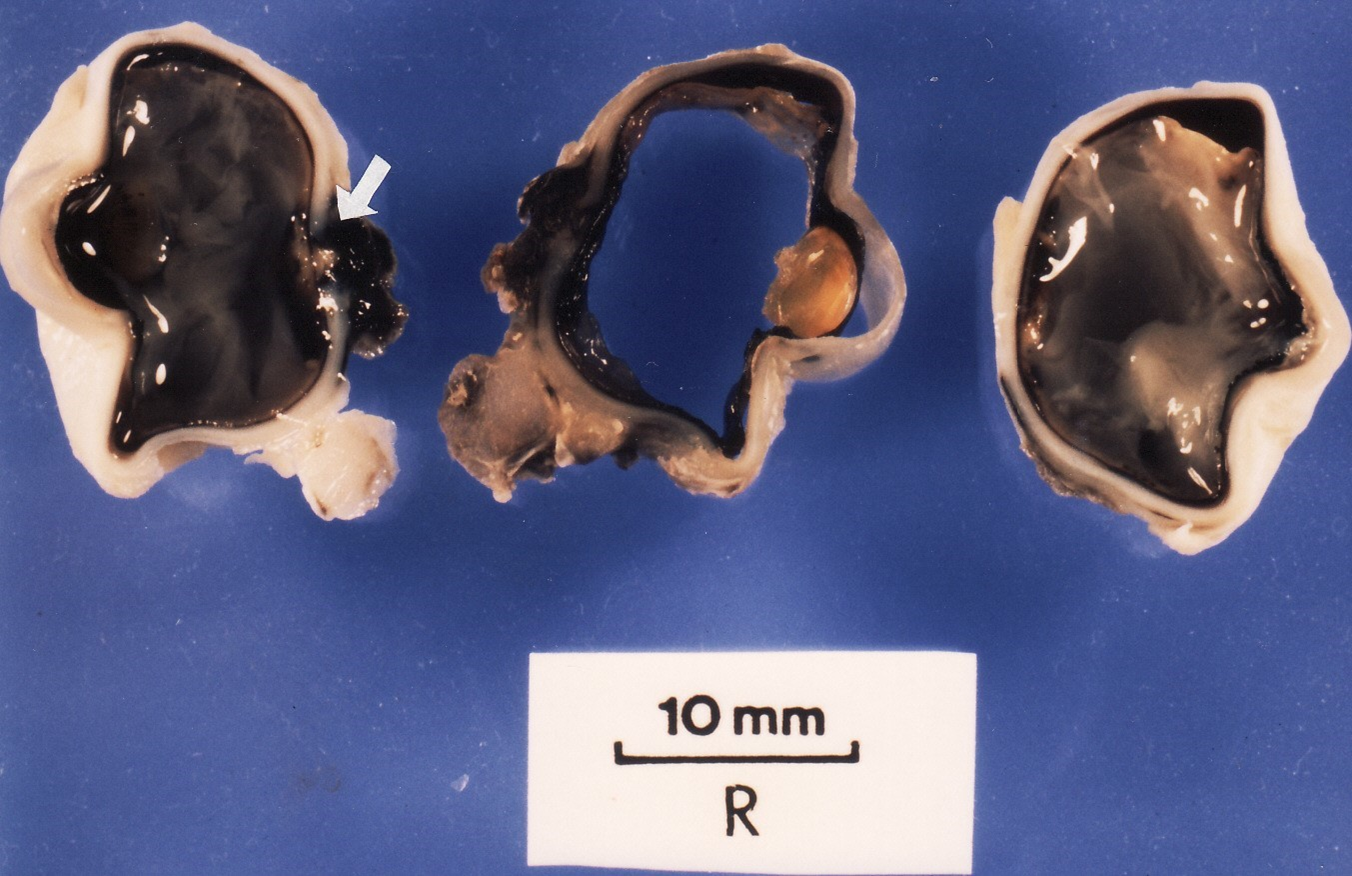
Fig.7 Formaldehyde-fixed eyeball trisection with subhyaloid (arrowed) haemorrhage 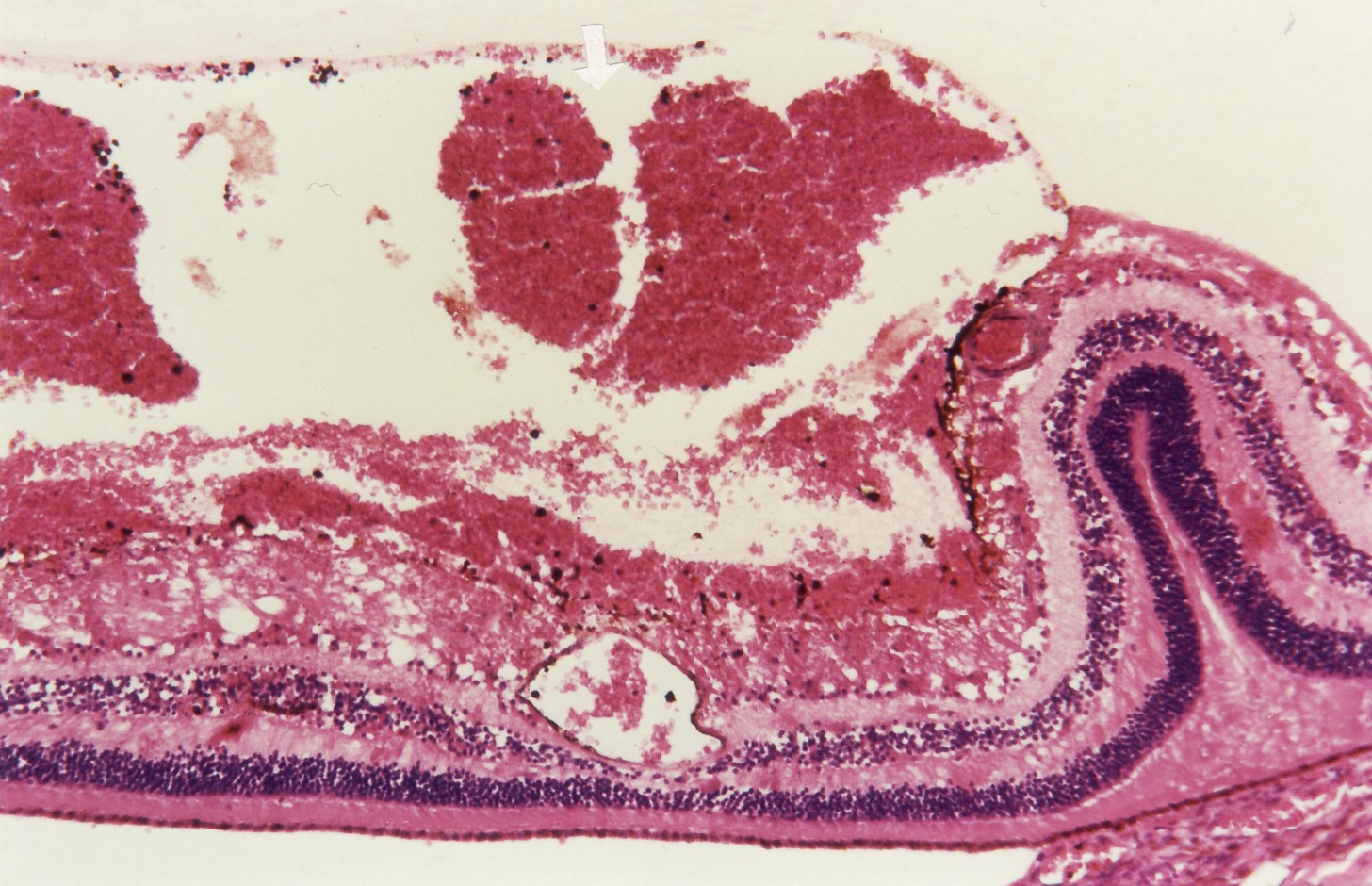
Fig. 8 Micrograph of right eye with subhyaloid (arrowed) haemorrhage (Haematoxylin Eosin x100) The retention of the eyes constitutes other appropriate examination related to the cause of death and therefore permitted by NFA in Part V, OSFP under s.26.
- After a preliminary briefing of the thanatopsy findings with the Police and crime scene manager, , criminal charges were brought against the parents, pending completion of police investigations.
- All significant material evidence were photographed in the original state as proof of evidence and retained. The postmortem report and photographs were disclosed to the defence solicitors representing the accused and given access to the postmortem exhibits. These are lawful requirements of NFA in Part VI, National Forensic Science and Biometric Department under s. 28,
DISCUSSION
The objectives in this reported long case of BBS are to emphasise the considerable diagnostic challenge in child abuse cases and the importance of adhering to the standardized MLDI protocol for the management of infanticides. It is prescribed for by the NFA in Part II, National Forensic Authority, under s. 4. The forensic service providers are duty bound to be consistent with the provision of the law relating to children's welfare in Zambia.
The NFA regulates forensic service providers by setting minimum quality standards, monitoring integrity, enforcing compliance with forensic ethical matters and public accountability in Part II, National Forensic Authority under s. 4. It enables forensic medical examination, collection and retention of exhibits and documentation of the clinico-pathological findings which can withstand the rigour of the legal process and possible judicial review. The guidelines issued by the National Forensic Authority in Part VII, General Provision under s. 33, is obligatory for all licensed forensic service providers. A breach in the legal requirements of the NFA such as non-compliance, submitting a false or misleading report and withholding material factual information is a criminal offence liable to a penalty in Part VII, General Provision under s. 31.
There are no reliable statistical data on incidence and prevalence of syndrome of child abuse and neglect (SCAN) in Zambia. However, it is common knowledge that Zambia is not immune from the global endemic of corporal punishment administered to children at home or school. Maltreatment of children and infliction of non-accidental trauma [NAT] on minors is a major medico-social problem.
It is entrenched in primeval traditions and sociocultural acceptance of poor parental skills which disregard child-friendly methods of teaching a lesson in discipline. It is now recognised that there is deliberate intention on the pretext of punishment rather than just impulsive parental chastisement in a moment of exasperation, often triggered by most trivial reason.[3]
The CCA provides legal means for correcting the outdated socio-cultural attitude on parental responsibility and the care and protection of minors in Zambia, and prosecution of culpable offenders. Corporal punishment of children as well as subjecting a child to torture and cruel treatment are prohibited in Part II, The Rights and Responsibility of Child under s. 22-23 respectively. It also entitles a child to be protected from maltreatment and any other form of exploitation under s. 17.
There are many variations of child abuse such as physical: sexual; psychological; neglect and deprivation. The characteristic features of the syndrome are recurrent NAT; mismatch between the injuries and false medical history; delayed medical attention; multiple attendance at different surgeries or hospitals to avoid suspicion.[3,4]
Generally, the injuries 'speak for themselves' about the mechanism, more so when medical history is inconsistent with the injuries. The clinical findings are variable and there may be several bruises, multiple fractures at different stages of healing, subdural haemorrhage with or without skull fracture, intraocular haemorrhaging, intra-oral trauma, bite marks, scalds and burns or marks of torture.[4] There was a triad of the listed findings in the case illustrated.
There are natural diseases that mimic NAT which must be proactively excluded such as skin disorders e.g. erythema infectiosum (slapped face disease), toxic epidermal necrolysis and chicken pox scars; blood disorders such as leukaemia and coagulation defect; bone disorder such as osteogenesis imperfecta (brittle bone disease); connective tissue disorders such as Ehlers-Danlos syndrome producing enhanced bruises, and retinal haemorrhage.[5] A child may be battered and finding a natural disease does not exclude SCAN.
Children sustain unintentional bruises and other minor injuries during abrasive playtime, and it can lead to conviction of innocent guardians telling the truth if they are misdiagnosed as NAT. It is of utmost importance to differentiate between evidence-based NAT and accidental injury and may be useful in unmitigated rebuttal of a clinical challenge in cases of suspected child abuse.
Ideally, every sudden and unexpected or unnatural deaths or when a medical certificate of the cause of death (MCCD) cannot be issued ought to be referred for thanatopsy, lest the corpse in an occult homicide is disposed of unchecked. The list includes suspicious and violent deaths; deaths due to child abuse and elderly abuse, medical negligence, poisoning, scheduled industrial diseases; custodial unexpected and sudden trauma death (CUSToD) syndrome,[6] and deaths that are of public interest. An infanticide case should be prosecuted by forensic pathologists who has gained postgraduate qualification in medical jurisprudence, and advisably jointly with a paediatric pathologist. The extent of a postmortem examination can be limited according to the circumstances surrounding the death and sociocultural traditions such that histopathological, toxicological and other allied scientific investigation may be omitted when appropriate.
The external injuries in the so-called shaken baby syndrome tend to be fingertip or grip-type bruising and distributed around the elbow and knee, as in this case when arms and legs are used as handles.5 As it is often difficult to age bruising accurately, a colour match photograph should be considered for the jury to see and decide.[5]
The internal injuries in SCAN may be severe such as pulmonary haemorrhages, even without rib fractures in a soft impact trauma; a ruptured hollow viscus from manual compression; mesenteric contusion from a direct blunt force to the abdomen which may not have an external sign; hepatic laceration inferiorly which may also be caused by frantic cardio-pulmonary resuscitation (CPR).[5] SCAN must be excluded when pancreatitis presents in children under the age of five.[5]
When there are no visible signs of non-accidental trauma in a suspected case of SCAN then toxicology must be considered to detect felonious poisoning. Microscopy examination may resolve a diagnostic dilemma, and the evidence can be preserved as histology slides. A search using ultraviolet light (UV) or refracted UV photography can reveal resolving faint bruises or old scars. The NFA in Part VI, National Forensic Service and Biometric Department under s. 27, 29 makes provision for the scientific collaboration. It is also advisable to conduct a 24-hour post-refrigeration re-examination of the body and look for latent bruises. In corpses with darkly pigmented skin, it may be necessary to examine the subcutis for evidence of soft tissue contusions caused by blunt trauma.
It is preferable to have colour photographs with a measure scale included within and shot by a professional photographer. It is noteworthy to be aware of a forensic folly due to colour mismatch and artefacts in forensic medicine. Also, beware of perjuriously doctored photographs when expert opinions are based without comparing them to the evidence in the flesh. The photographs may be put before the jurors in an aesthetic form to help with comprehending esoteric medical expert opinions.
All forensic exhibits must be properly documented and submitted to the SFA as in Part VI, National Forensic Science and Biometric Department under s. 28, and disclosed to properly interested party. The NFA makes it a criminal offence liable to a penalty in Part VII, General Provision under s. 31, to submit a false or misleading report or withholding material information.
The conclusion drawn from the postmortem examination was that her death was due commotio cerebri which was entirely consistent with violent shaking of the head. There was no evidence that natural diseases, congenital abnormalities or hospital treatment or resuscitation could have caused or contributed to her death. The pattern of the bruises on the limbs strongly indicated violent gripping as convenient handles for shaking or tossing the baby. The bruising in association with finger nail marks were contemporaneous with the SDH and consistent with being inflicted less than several days prior to her death, based on microscopy findings of erythrocyte lysis with fibrin formation [Figure 9].
A commotio cerebri was produced either by an impact of the head or violent shaking of the head as in the so-called shaken baby syndrome but biomechanical studies supports a blunt force although shaking may be a part of it.[7] The mechanism could be operating when the victim is thrown against upholstered furniture as alleged in this case which would not necessarily produce external mark of cranial trauma.[7] However, it does not explain a SDH associated with innocent shaking of the head to resuscitate the baby.[3] A SDH may also be caused by cavernous sinus thrombus which may be infective in meningitis and otitis media, or aseptic due to dehydration.
The age of SDH was of considerable forensic interest in relation to the perimortem events. A precise estimate may not be possible even upon histological examination, particularly in the crucial early period. This was evident at the committal proceedings in this case because of considerable delay between presenting symptoms and detection of a non-accidental trauma to the head.
An ocular injury was a significant sign for suspecting SCAN. A retinal haemorrhage is a reliable indicator but not pathognomonic as it can occur in non-traumatic conditions such as bleeding diathesis, bacterial endocarditis and Purtscher retinopathy due to sudden rise in retinal venous pressure caused by chest compression during CPR.[4] A SDH causing raised intracranial pressure may be accompanied by retinal haemorrhage if the retinal venous drainage is obstructed e.g. Terson syndrome.
The NFA in Part V, OSFP under s. 24, mandates the SFP who provides forensic pathology services to conduct other appropriate examination or investigation relevant to the cause of death. The SFP must properly record forensic findings and results of ancillary examinations or investigation and prepare a postmortem examination report for the coroner and Zambia Police Service under s. 26. Furthermore, the SFP must maintain or dispose histology, toxicology and any other samples for necessary investigation under s. 26.
CONCLUSION
The forensic postmortem report in this case was admitted as documentary evidence at the committal proceedings in a magistrate court. The pathologist for the defence representing the mother was entirely in agreement. The pathologist for the father agreed with the essence of the thanatopsy findings but disputed the estimated date of SDH and age of bruising. It was conceded that dating SDH was at best only an approximation, and colours of bruises can be unreliable due to varied factors.
The case was committed for a trial in the High Court where the defence team for the father had commissioned a consultant neuropathologist to act as an expert witness. This strategy was countered by the prosecution who engaged an eminent professor of neuropathology as a trump card.
It is required of the defence solicitors to reciprocate and disclose all medical and scientific evidence to the prosecution lawyers prior to a trial. The medical report prepared by the defence expert emphasised the differential diagnoses of SCAN. The contention was not so much the dating of SDH and age of bruises but the cause of death itself. The defence neuropathologist gave meningococcal meningitis as the primary cause of death, contrary to the pathologists on the same side. A sequence of events was postulated that infection and dehydration precipitated a sagittal sinus thrombus which in turn caused a unilateral SDH, and thereafter a raised intracranial pressure produced intraocular haemorrhages.
At a pretrial case conference, the prosecuting Counsel was briefed on the exculpatory expert opinions of the defence neuropathologist. Advice was also sought on the confidence in the cause of death and the strength of thanatopsy which excluded any natural disease that could have caused or contributed to death. The expert opinions of the prosecution neuropathologist assisted in rebutting meningitis as a natural cause of death.
The prosecution case of the cause of death due to NAT was strongly challenged by the defence counsel at the trial. The prosecution expert witness categorically rebutted existence of sagittal sinus thrombosis or meningitis. A consultant paediatrician who had attended to the baby gave evidence that meningitis was specifically excluded by laboratory tests. Upon cross-examination the defence expert witness retracted meningitis as a cause of death and shifted the emphasis on the clinically evident dehydration as the underlying cause. The evidence of the forensic pathologist upon re-examination was that a triad of SDH, ocular haemorrhage and grip-type bruises was virtually diagnostic of battered baby syndrome in absence of a natural disease or another cause.
The nuance of clinico-pathological evidence seemed to be difficult for the jurors, and after several hours of deliberation a hung jury was not able to deliver a verdict. A retrial was granted, and the jury was dismissed.
After a pause of several days, the father admitted violently shaking the baby in exasperation under difficult circumstances when she refused her feed, but did not intend to harm the child. The court duly recorded a change of plea to guilty of unlawfully killing the baby and assault causing actual body harm. The accused received a suspended sentence. The mother was found not guilty of causing unnecessary suffering to a child.
A good judicial denouement is recognised when there is incontestable medical evidence of guilt, and it is backed by a self-confession of the accused which is not a false confession extracted under duress. A guilty verdict based on unsafe medical expert opinions can be detrimental to good practice in forensic medicine. To this purpose, it is highly recommended that forensic service providers in Zambia religiously follow the provisions of the statutes, namely the CCA which relates to children's welfare and the NFA which regulates and prescribes a standardized practice of forensic pathology and science in child abuse cases.
REFERENCES
- http://laforensic.org/.../202108/Strenghtening-MLDI-in-Z.
- Davis RJ. Forensic science on the quality track. Journal of Forensic Science Society1991; 31:407.
- Gee D.J. Cruelty to children: the battered baby (non-accidental) injury. In: C.J. Polson, D.J. Gee and B. Knight (editors) The Essentials of Forensic Medicine. -4th Edition. Chapter 16. 1985. Oxford. Pergamon Press.
- 1. 4, Pearn J. Physical abuse of children. In: J.K Mason (editor) Paediatric Forensic Medicine and Pathology. Chapter 16. 1989. London. Chapman and Hall Medical.
- Knight B. The autopsy in non-accidental injury syndrome. In: JK Mason (editor) Paediatric Forensic Medicine and Pathology. Chapter18. London. Chapman and Hall Medical.
- Patel F. Custodial restraint asphyxia. American Journal of Forensic Medicine and Pathology 2000; 21:196-7.
- Duhaime A. et al. The shaken baby syndrome: a clinical, pathological and biochemical study. Journal of Neurosurgery 1987; 66:409-15.
STATUTES
Inquest Act 1939 (Zambia)
National Forensic Act, 2020 Act 2 of 2020 (Zambia)
Children's Code Act, 2022 Act 12 of 2022 (Zambia)
Medical Journal of Zambia, Vol 51, 4
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.