Acceptability Factors of Tetanus Toxoid Vaccination among Women in Fiwale, Masaiti District, Zambia
Chimponda Mary
Department of Public Health, Michael Chilufya Sata School of Medicine, Copperbelt University, Ndola, Zambia).
Mubbunu Lumamba
Department of Basic Sciences, Michael Chilufya Sata School of Medicine, Copperbelt University, Ndola, Zambia.
Siziya Seter
Department of Public Health, Michael Chilufya Sata School of Medicine, Copperbelt University, Ndola, Zambia).
DOI: https://doi.org/10.55320/mjz.51.4.451
Keywords:Vaccination, Tetanus toxoid, Prevalence, Correlates, Rural district, and Tetanus
ABSTRACT
Background: Tetanus toxoid vaccines are effective against maternal and neonatal tetanus. Despite its effectiveness and availability, its utilization is generally low in some populations. The level of its use and the factors associated with its acceptability in Masaiti a rural district of Zambia, are unknown.
Aim of the study: The objective of this study was to establish the prevalence and factors associated with acceptability for Tetanus toxoid vaccination.
Methods: A cross-sectional study was conducted using a questionnaire with a sample size of 305. Pearson’s Chi-square test and multiple logistic regression analysis were performed to identify factors associated with immunization status at the level of significance of 5%. Women aged 15 to 49 years were included in the study at Fiwale, Masaiti district of Zambia. Adjusted odds ratios (95% CI) were reported.
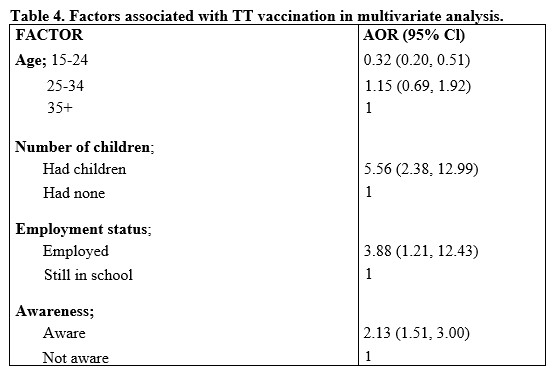
Results:A total of 293 (96.1% response rate) women participated in the survey of which 135 (46.1%) were vaccinated. Respondents who were in the age group of 15-24 years were 68% less likely to be vaccinated than those aged 35 years or older. Participants who had children were 5.56 times more likely to be vaccinated than those who did not have children; Furthermore, participants who were employed were 3.88 times more likely to be vaccinated compared to those who were not employed. Respondents who knew about TT vaccination were 2.13 times more likely to be vaccinated than those who were not aware.
Conclusion:This study revealed a lower than recommended uptake of tetanus toxoid (TT) vaccination among women in Fiwale, Zambia. Demographic factors such as age, education level, marital status, number of children, and employment status were significantly associated with vaccination status. Younger, less educated, unemployed, unmarried, and childless women were more likely to be unvaccinated. To increase TT vaccination rates, targeted interventions should focus on these vulnerable groups. Awareness campaigns, community outreach programs, and mobile vaccination clinics can be effective strategies to disseminate accurate information and facilitate convenient access to vaccination services.
INTRODUCTION
The Zambian government under the Ministry of Health is working to eliminate maternal and newborn tetanus as one of the objectives of the World Health Organization (WHO) by 2030. However, the vaccination rate among women of childbearing age for the tetanus toxoid vaccine remains below the 2020 goal of 80% coverage for healthy people.[1]
The burden of maternal and neonatal tetanus is a pressing health equity issue that predominantly impacts vulnerable populations, such as the impoverished and those residing in areas with inadequate healthcare infrastructure. Fiwale district, a rural area characterized by widespread poverty and limited access to essential health services, exemplifies this disparity. Maternal and neonatal tetanus has been called a silent killer[2] , as victims often die without being officially recorded. Tetanus is estimated to cause 213,000 to 293,000 deaths worldwide each year and is responsible for 5 -7% of all newborn deaths and 5% of maternal deaths.[3] Zambian records show that mothers who are protected against neonatal tetanus based on ages less than 20 years were 65.3%, 20-34 years were 81.5%, and 35-49 were 82.6% more likely to be vaccinated.[1] Maternal and neonatal tetanus is an important cause of maternal and neonatal mortality, claiming about 180,000 lives worldwide every year, almost exclusively in developing countries.[4] Although easily prevented by maternal immunization with the toxoid tetanus vaccine and aseptic obstetric and postnatal umbilical cord care practices, maternal and neonatal tetanus persists as a public health problem in many countries, mainly in Asia and Africa.[5] The provision of tetanus toxoid immunization to women of childbearing age helps to achieve the goal of worldwide elimination of maternal and neonatal tetanus.[6] Continued elimination will require improvements to the currently inadequate immunization and health service infrastructures and universal access to these services.
Most tetanus cases occur in sub-Saharan Africa, where progress has been slower and countries are still developing, but with the help of vaccine, the number of tetanus cases decreased by 75% between 1990 and 2016 in sub-Saharan Africa.[1] New tetanus infections have decreased worldwide since 1990 with the number of maternal and newborn tetanus elimination cases (MNTE) decreasing by 89% in period.[5]
Factors such as sociodemographic characteristics and utilization of antenatal care services have been found to be associated with vaccination status. For example, a high number of ANC visits is associated with the use of TT immunization.[5] Studies have also shown that mothers who use the follow-up of the ANC service[7] , older[8] , educated[9] and living closer to health facilities are more likely to be immunized. Furthermore, Shafiq et al[9] . reported that the lack of information on the TT vaccine service was more likely to be associated with not receiving the TT vaccine. In a study by Fournet et al.[6] , several common beliefs were found to be associated with a nonvaccinating state. Similarly, a study by Akmatov et al[10] reported that participants with negative attitudes toward vaccinations were more likely to be unvaccinated.
Zambia is one of the countries that has benefitted from the positive impact of the vaccine in terms of reducing cases of tetanus. The number of cases and deaths caused by tetanus has steadily declined in recent decades. Despite the positive impact, some parts of the country have received the vaccine with a negative attitude, and this has resulted in the abandonment of the vaccine target. If shunning continues, maternal and neonatal deaths due to tetanus shall continue to occur when full protection of women against tetanus is not achieved.
This study aimed to determine coverage, and identifying key socio-demographic factors influencing tetanus toxoid vaccination acceptability among women in Fiwale district.
METHODS AND MATERIALS
Research Settings
The study was conducted at the Fiwale Rural Health Centre located approximately 50 km east of the Masaiti District Health Office on the Copperbelt Province. Fiwale Rural Health Centre is a Mission Health Centre run by the Northern Baptist Association of Zambia (NBAZ), which was established in 1938.[11] This Rural Health Centre does not have admitting wards; however, the services offered include maternal and child health (MCH), maternity ward, outpatient department, antiretroviral therapy (ART) services, laboratory, and pharmacy services. The annual outpatient attendance for women aged 15 to 49 years was two thousand and seven in 2019.[11]
Study population
The target population for this study was women between 15 and 49 years of age at Fiwale Rural Health Centre.
Study design
In this study a cross-sectional approach was adopted. It involved the gathering of data that reflect experiences, focusing on perceptions and opinions of women of childbearing age who participated in the research.
Sample size
The sample size for the study was determined using the formula by Cochran (1963) for finite populations. Where n is the desired sample; P is the prevalence 29%; q is I-p; Z is the standard normal deviation (1.96 at 95% CI); e is the degree of precision.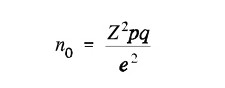
Taking the annual outpatient attendance for women aged 15 to 49 years at Fiwale Rural Health Centre of two thousand and seven (2007) in 2019 [11]; the calculated sample size was 274. Thereafter, considering a 10% nonresponse rate, the sample size was adjusted to 304.
Sampling Procedure
Sample selection
In this study, 293 women between 15 and 49 years of age were systematically randomly sampled without replacement from the target population of 2007 women in Fiwale according to the attendance record for 2019[11] . Systematic random sampling was used to achieve a more uniform spread over the entire population and therefore be more representative of the population.Inclusion Criteria
The sample included women between 15 and 49 years of age who accessed health care services at the Fiwale Rural Health Centre. The study only included those who gave their consent to participate in the study.
Exclusion Criteria
The study excluded women between 15 and 49 years of age who did not give their consent and young women who had not reached the age of 15 years who had no guardians to obtain permission from, as well as women of their childbearing age who accessed health services from other rural health centres. Women who did not fall in the age bracket were also excluded from the study.
Data Collection
The study used a questionnaire to collect data. The questionnaire was developed following the World Health Organization Vaccination Coverage Cluster Surveys reference manual.12 The questionnaire was translated from English to Bemba and Lamba languages. Translation was done so that subjects could easily understand the questionnaire, as these languages are spoken within the Fiwale area. The questionnaire comprised questions on information on tetanus toxoid vaccination, accessibility of services to patients, the attitude of health personnel towards patients, and record keeping in patients. The questionnaire was a written interview conducted face-to-face. A preliminary pre-test of a semi-structured questionnaire was conducted on thirty individuals at Fiwale Health Centre, and these same individuals were not included in the main study. This was done to adjust the questionnaire, as well as to estimate the duration the respondent would be expected to take in answering the questionnaire. All questionnaires were serialized using a unique number per respondent to facilitate the validation and accountability process. The complete questionnaires were verified for completeness and then stored by researchers.
Data Management and Analysis
The collected data was coded and entered into a computer database designed using the Microsoft Excel application. Data verification and validation was performed by rechecking all data entries with the original data forms to achieve a clean data set that was then exported into a Statistical Package for Social Sciences (SPSS) version 20 for analysis. Pearson’s Chi-square was used to evaluate for the association between dependent and independent variables at a significance level of 5%. An odds ratio with a 95% confidence interval was reported. Further logistic regression was used to identify independent predictors of maternal vaccination status at a 5% significant level.
Ethical clearance
The study did not collect names or any information that could be used to identify study participants. Questionnaires were identified by prewritten serial numbers. The information collected during the study was used only for the purposes indicated in the study objectives. Ethical clearance was granted by the Ethics Committee of the Tropical Diseases Research Centre (TDRC) IRB00002911 FWA number: 00003729. The approval number for the study is TRC/C4/06/2020.
RESULTS
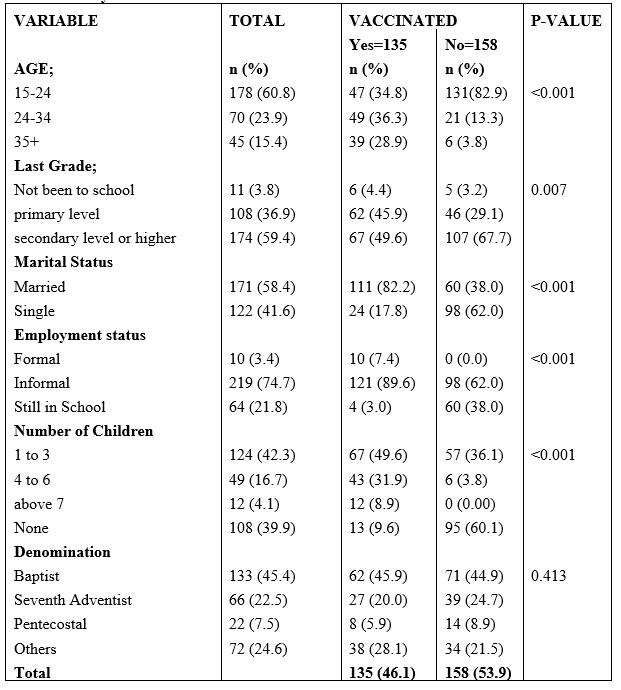
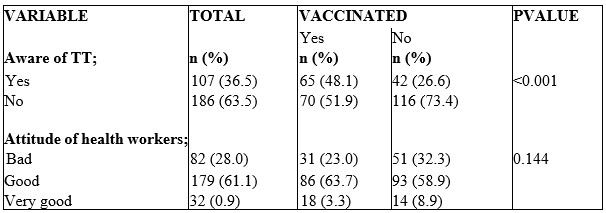
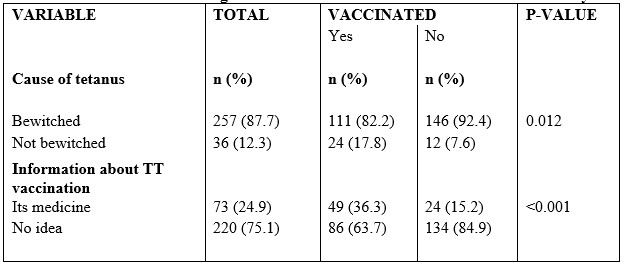
Social-demographic characteristics of the sample A total of 293 respondents participated in the survey, of which 135 (46.1%) respondents were vaccinated. Table 1 represents the sociodemographic characteristics of the respondents. Age, the last grade achieved, marital status, number of children, and employment status were significantly associated with vaccination. Individuals who were not vaccinated tended to be younger, of little educational status and unmarried.
DISCUSSION
In general, 46.1% of the participants in the current study were vaccinated and the factors associated with TT vaccination were age, number of children, employment status, and awareness of TT vaccination. This finding shows that the percentage of Fiwale TT vaccination is low compared to the Zambian ministry of health 2020 goal of 80% coverage for healthy people.[1] Furthermore, other studies in sub-Saharan Africa have shown similar findings; for example, Anatea et al.[13] reported a percentage of 41.1% TT vaccination among women of reproductive age in Dukem city, eastern Ethiopia, which is similar to the findings of this study. Furthermore, the finding of the current study is also like that reported by Abuwa et al.[14] who reported complete vaccination of 41.2%, and Dubale & Kalbiso[8] who reported 49% utilization of TT according to the Ethiopian Demographic Health Survey of 2016. Shafiq et al.[9] reported that 43% of women in Karachi had received the TT vaccine. Other related findings are those of those of Maral et al.[15] who reported that 46.7% of pregnant women were vaccinated against tetanus. Hassan et al.[16] in Cairo Governorate, Egypt, reported that only 42.6% of the mothers studied were fully protected against maternal and neonatal tetanus in their last birth.
Although this study reports a low coverage of TT vaccination, other studies reported a much lower utilization status. Kalaca et al.[17] reported that only 25.7% of women had received tetanus vaccinations, while Gebremedhin et al.[18] reported that 14.8% of women had received all five doses of TT. In another study by Perry et al.[19] conducted in zone 3 of Dhaka city in urban Bangladesh, 11% reported having obtained the complete series of five TT immunizations. Balafama and Boma[20] reported a very poor coverage of 2% (TT) in a study among undergraduate students at a Nigerian university. Mehanna, Ali and Kharboush[21] reported that only 17% had received 5 complete doses of the vaccine, and Gebremedhin et al.[18] reported a low coverage of 14.8%, which is well below the World Health Organization 100% vaccination rate.
The finding of 46.1% in the current coverage study was less than the TT vaccination reported by other studies as well; for example, Afridi et al.[22] and Naeem et al.[23] , which were 65% and 55.6%, respectively.
The present study found that age was associated with the vaccination status of TT, it was found that women between 15-24 years of age were 68% less likely to be vaccinated than those 35 years or older. The findings of this study are similar to the results of Shafiq et al. [9] who reported that age less than 25 years was associated with non-vaccination compared to women 25 years or older. Furthermore, this finding is also similar to the finding of Dubale et al.[8] which revealed that women aged 30 and older were more likely to be vaccinated than those under 21 years of age. It is hypothesized that many women older than 25 years have a high vaccination rate because at this age many would already have been pregnant and attended antenatal services where tetanus vaccination is mandatory. Respondents who had children were more likely to be vaccinated than those who did not have children. The finding corresponds to the findings reported by Dubale and Kelbiso.[8] The observed finding could be due to the opportunity to get the TT vaccine and the knowledge about its importance that antenatal care visits (ANC) provide during visits. The result of this study is consistent with that of Esen et al.[24] who reported that women who had children had greater odds of being vaccinated with TT than those without children.
Contrary to the finding of the present study, the result reported by Ahmed and El-Barrawy 25 revealed that greater parity was significantly associated with a lower number of doses of the TT vaccine. The lowest percentage of fully vaccinated women was observed among women who had experienced more than one pregnancy. Similarly to the findings of this study on the number of children and the status of vaccination, the studies by Gebremedhin et al.[18] and Yaya et al.[26] reported that multiparity was significantly associated with the uptake of tetanus toxoid vaccination. The reason could be attributed to the mandatory administration of TT vaccination to women when they register for ANC. The other explanation may be related to the fact that those with a history of pregnancy could have been exposed to health education and counselling about TT vaccination by health care providers during ANC visits.
The study also found that employment status considerably predicted acceptance of TT vaccination. The employed participants in the study were more likely to be vaccinated compared to those still in school. This result is consistent with the study reported by Asundep et al.[27] , and Anatea, Mekonnen and Dachew [13] . Compared to the findings of this study, the studies by Naeem et al.[13] and Belihu et al.[28] are comparable, as they found that occupation status is significantly associated with TT immunization. Similarly to the finding of this study that employment is associated with TT vaccination, women's employment was reported to contribute to having been sufficiently immunized against tetanus by Haile, Chertok and Teweldeberhan[29] in a Kenyan study. The possible reason might be due to the accessibility of transport to health facilities that employed tend to have transportation compared to unemployed, as well as having relatively more advanced education.
The current study finding found that those who knew about the tetanus vaccine were more likely to be vaccinated than those who did not. This observation is similar to a previous study by Roosihermiatie et al.[30] who reported that those who were aware of TT vaccination were more likely to have been vaccinated than those who were not aware. Similarly, Shafiq et al.[9] in a study of knowledge, attitudes, and practices related to tetanus toxoid vaccination in women of childbearing age found that those with knowledge were more likely to be vaccinated. A cross-sectional study in Karachi peri-urban settlements found that ignorance of tetanus vaccination was a non-vaccination predictor. Similarly, in the study by Balafama and Boma[20] , the odds of being vaccinated with the tetanus vaccine were higher in participants who were aware than in those who were not aware of the vaccine. Consistent with this finding is that of Naeem et al.[23] and Siddiqui et al.[31] who reported that lack of awareness of vaccination had higher odds of not being vaccinated; it is hypothesized that awareness increases mother's health-seeking behaviour and opens an opportunity for TT vaccination during childbearing age. Ahmed and EL-Barrawy[25] in the study in the Dakahlia governorate, Egypt, reported that the lack of awareness of the importance of the vaccine was attributed to the unvaccinated status, as those who were not aware were more likely to be unvaccinated than women who were aware. For this reason, raising awareness campaigns to strengthen women's knowledge of the importance of vaccination with TT and receiving the said vaccine will greatly help ensure that women are vaccinated with TT. In line with the finding of the present study, the result of Hasnain, Sheikh[32] also revealed that those who were aware of the TT vaccination and its importance were more likely to be vaccinated than those who were not aware.
CONCLUSION
This study revealed a lower than recommended uptake of tetanus toxoid (TT) vaccination among women in Fiwale, Zambia. Demographic factors such as age, education level, marital status, number of children, and employment status were significantly associated with vaccination status. Younger, less educated, unemployed, unmarried, and childless women were more likely to be unvaccinated. To increase TT vaccination rates, targeted interventions should focus on these vulnerable groups. Awareness campaigns, community outreach programs, and mobile vaccination clinics can be effective strategies to disseminate accurate information and facilitate convenient access to vaccination services.
Study limitations
The target population was limited to women of childbearing age between 15-49 years of age who visited the Fiwale Rural Health Centre; therefore, interpretation of the findings may not be used to other women of childbearing age beyond the Fiwale region. Furthermore, the study was susceptible to recall bias as data on vaccination status were based on the self-reporting of the respondents.Acknowledgement
In memory of Mary Chimponda who passed away after completing her MPH program and graduated posthumously, at Copperbelt University, Michael Chilufya Sata School of Medicine (CM).Competing interests
The authors declare no competing interest.
Authors’ contributions
Conceptualization, CM, SS; methodology, CM, SS; data collection, CM; analysis, CM, SS, ML; drafting of manuscript, ML, SS; review and editing, ML, SS; supervision, SS; manuscript submission, ML and SS have read and agreed to the published version of the manuscript.
Funding
This study did not receive any specific funding.
REFERENCES
- 1. Zambia demographic and health survey. Zambia statistics agency 2018. Lusaka: Ministry of Health [Zambia]; 2020
- Fry M, Edwards G, Taylor A. Tetanus--the silent killer: how safe are you? Aust Crit Care. 1998;11(3):82-85.
- European Centre for Disease Prevention and Control (2019). Disease Factsheet about Tetanus, An agency of the European Union https://www.ecdc.europa.eu/en/tetanus/facts
- Rooper MH, Vandelaer JH, Gasse FL. Maternal and neonatal tetanus. Lancet. 2007;370 (9603): 1947-59.
- Nigussie J, Girma B, Molla A, Mareg M. Tetanus Toxoid Vaccination Coverage and Associated Factors among Childbearing Women in Ethiopia: A Systematic Review and Meta-Analysis. Biomed Res Int. 2021; 2021:5529315.
- Fournet N, Moliema L, Ruijs WL, Harmsen IA, Keck F, Durand JY, et al. Under-vaccinated groups in Europe and their beliefs, attitudes and reasons for non-vaccination; two systematic reviews. BMC Public Health. 2018;18(1): 196
- Baltazar JC, Sarol JN Jr. Prenatal tetanus immunization and other practices associated with neonatal tetanus. Southeast Asian J Trop Med Public Health. 1994;25(1):132-8
- Dubale MM, Kelbiso HL. Tetanus toxoid immunization status and associated factors among mothers in Damboya woreda, Kembata tembaro zone, SNNP, Ethiopia. J Nutr Metab. 2018; 2018:2839579
- Shafiq Y, Khowaja AR, Yousafzai MT, Ali SA, Zaidi A, Saleem AF. Knowledge, attitudes and practices related to tetanus toxoid vaccination in women of childbearing age: A cross-sectional study in peri-urban settlements of Karachi, Pakistan. J Infect Prev. 2017;18(5):232-41
- Akmatov MK, Rübsamen N, Deyneko IV, Karch A, Mikolajczyk RT. Poor knowledge of vaccination recommendations and negative attitudes towards vaccinations are independently associated with poor vaccination uptake among adults - Findings of a population-based panel study in Lower Saxony, Germany. Vaccine. 2018;36(18):2417-26
- Fiwale Rural health Centre. Fiwale Action plan 2020- 2022. Ndola: Ministry of Health [Zambia]; 2019
- Vaccination Coverage Cluster Surveys: Reference Manual. Geneva: World Health Organization; 2018 (WHO/IVB/18.09). License: CC BY-NC-SA 3.0 IGO.
- Anatea MD, Mekonnen TH, Dachew BA. Determinants and perceptions of the utilization of tetanus toxoid immunization among reproductive-age women in Dukem town, eastern Ethiopia: a community-based cross-sectional study. BMC Int Health Hum Rights. 2018;18(1):27
- Abuwa PN, Alikor EA, Gbaraba PV, Mung KS, Oruamabo RS. Determinants of tetanus toxoid immunization of parturient women: a community-based study in Rivers State of Nigeria. West Afr J Med. 1997;16(3):174-8
- Maral I, Baykan Z, Aksakal FN, Kayikcioglu F, Bumin MA. Tetanus immunization in pregnant women: evaluation of maternal tetanus vaccination status and factors affecting rate of vaccination coverage. Public Health. 2001;115(5):359-64
- Hassan AM, Shoman AE, Abo-Elezz NF, Amer MM. Tetanus vaccination status and its associated factors among women attending a primary healthcare centre in Cairo governorate, Egypt. J Egypt Public Health Assoc. 2016;91(3):127-34
- Kalaqa S, Yalgin M, Simsek YS. Missed opportunities for tetanus vaccination in pregnant women and factors associated with seropositivity. Public Health. 2004;118(5):377-82
- Gebremedhin TS, Welay FT, Mengesha MB, Assefa NE, Werid WM. Tetanus Toxoid Vaccination Uptake and Associated Factors among mothers who gave birth in the Last 12 Months in Errer District, Somali Regional State, Eastern Ethiopia. Biomed Res Int.2020; 2020:4023031
- Perry H, Weierbach R, Hossain I, Islam R. Tetanus toxoid immunization coverage among women in zone 3 of Dhaka city: the challenge of reaching all women of reproductive age in urban Bangladesh. Bull World Health Organization. 1998;76(5):449-57
- Balafama AH, Boma O. Awareness and status of tetanus toxoid vaccination among female undergraduate students in a Nigerian University. Int J Trop Dis Health. 2015;7(1):6-15
- Mehanna A, Ali MH, Kharboush I. Knowledge and health beliefs of reproductive-age women in Alexandria about tetanus toroid immunization. J Egypt Public Health Assoc. 2020;95(1):22
- Afridi NK, Hatcher J, Mahmud S, Nanan D. Coverage and factors associated with tetanus toxoid vaccination status among females of reproductive age in Peshawar. J Coll Physicians Surg Pak. 2005;15(7):391-5
- Naeem M, Khan VIZ, Abbas SH, Adil M, Khan A, Naz SM, et al. Coverage and factors associated with tetanus toxoid vaccination among married women of reproductive age: a cross-sectional study in Peshawar. J Ayub Med Coll Abbottabad. 2010;22(3):136-40
- Esen B, Kurtoglu D, Coplu N, Gozalan A, Miyamura K, Ishida S, et al. Tetanus immunization status among women of childbearing age in Turkey. Jpn J Infect Dis. 2007;60(2-3):92-6.
- Ahmed Al, EL-Barrawy AM. Factors Affecting Maternal Tetanus Vaccination in Dakahlia Governorate, Egypt. Journal of High Institute of Public Health (JHIPH). 2019;49(1):30-5
- Yaya S, Kota K, Buh A, Bishwajit G. Antenatal visits are positively associated with uptake of tetanus toxoid and intermittent preventive treatment in pregnancy in Ivory Coast. BMC Public Health. 2019;19(1):1467
- Asundep NN, Jolly PE, Carson A, Turpin CA, Zhang K, Tameru B. Antenatal care attendance, a surrogate for pregnancy outcome? The case of Kumasi, Ghana. Matern Child Health J. 2014;18(5):1085-94
- Belihu KD, Tesso FY, Woldetsadik TD. Dropout rate of tetanus toroid immunization and associated factors among reproductive age group of women in Debrebirhan town, Amhara Region, Northern Ethiopia. Journal of women's health care. 2017; 6:390.
- Haile ZT, Chertok IRA, Teweldeberhan AK. Determinants of utilization of sufficient tetanus toxoid immunization during pregnancy: Evidence from the Kenya demographic and health survey, 2008-2009. J Community Health. 2013; 38:492-9
- Roosihermiatie B, Nishiyama M, Nakae K. Factors associated with TT (tetanus toxoid) immunization among pregnant women, in Saparua, Maluku, Indonesia. Southeast Asian J Trop Med Public Health. 2000;31(1):91-5
- Siddiqui AA, Khan M, Khan JA, Haseeb SS, Mohib A, Kadri MM. Awareness, knowledge, and coverage of vaccination against tetanus, diphtheria, and pertussis among medical students of Karachi: a cross-sectional analysis. Cureus. 2019;11(4): e4472
- Hasnain S, Sheikh NH. Cause of low tetanus toxoid vaccination coverage in pregnant women in Lahore district, Pakistan. East Mediterr Health J. 2007;13(5):1142-52
Medical Journal of Zambia, Vol 51, 4
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.