Rare type of cancer of the cervix in a seventeen-year-old virgin: A case report
Tapuwa Gracious Motsi
Oncocare Cancer Centre, 1 Walmer Drive Newlands, Harare, Zimbabwe
Eucaria Mushosho
School of Allied Health Sciences, Harare Institute of Technology
Bornface Chinene
School of Allied Health Sciences, Harare Institute of Technology
DOI: https://doi.org/10.55320/mjz.51.3.551
Keywords:cervical cancer, virgins, Human Papilloma Virus, HPV-negative cervical cancer
ABSTRACT
Cervical cancer among virgins is very rare. This is due to the main causative factor of the cancer being the sexually transmitted Human Papilloma Virus (HPV), which accounts for 99% of all cervical cancer cases. Presented here is a case of a seventeen-year-old patient with no history of any sexual intercourse, who presented with pelvic bleeding and upon undergoing an ultrasound scan, a cervical mass was noted. The biopsy showed an adenocarcinoma of the uterine cervix with no trace of HPV DNA. Radical modified hysterectomy was performed which was followed by adjuvant radiation treatment given concomitantly with six cycles of chemotherapy. She also received brachytherapy. Unfortunately, the patient deceased, almost two years after initial the diagnosis due to kidney failure caused by radiation nephropathy. This case report sheds light on the possibility of HPV-negative cervical cancer in virgins which can be attributed to factors other than HPV infection. It underscores the potential risk of overlooking cervical cancer in virgins, which may lead to late-stage diagnosis. This case report also adds to the literature on HPV-negative cervical cancer where there are a few recorded cases.
INTRODUCTION
Cervical cancer is a malignant tumour of the lower-most part of the uterus: the cervix. It is the third most common cancer among women worldwide[1]. In Zimbabwe, it ranks as the first leading cause of female cancer with about 3,186 new cervical cancer cases being diagnosed annually[1]. An estimation of 2270 women are diagnosed with cervical cancer in Zimbabwe annually and a mortality rate of 64% has been recorded[2].
Cervical cancer is mainly caused by Human Papilloma Virus (HPV), a sexually transmitted infection. HPV accounts for the cause of 99% of all cervical cancer cases[3]. The infection has over 100 types, with approximately thirteen capable of causing cancer, particularly types 16 and 18, which are responsible for 70% of cervical cancer cases[3]. Squamous carcinomas account for 85-95% of invasive cervical cancer cases, while the rest are adenocarcinomas or adenosquamous tumours.
Besides HPV, smoking and exposure to other sexually transmitted infections like Human Immune Virus are also risk factors for cervical cancer[4]. Invasive cervical cancer rarely affects women under 21, with only 0.1% of cases occurring before this age[5]. The occurrence of cervical cancer in 15 to 24-year-olds is low. This is due to the natural history of the HPV type of disease and most virgins are found within this age range[5].
Despite the advancement of very sensitive tests for detecting HPV at the molecular level, and regardless of the method employed for HPV detection, a small number of cervical cancer cases may test negative for HPV[6]. These cancers are termed HPV-negative cervical cancers. Approximately 3-8% of cervical cancer cases represent HPV-negative cervical cancer[7]. There is a consistent reporting of cervical cancer cases that are not influenced by HPV in clinical practice. Cervical cancer patients who test negative for HPV display a notably poorer prognosis, primarily because of advanced International Federation of Gynecology and Obstetrics (FIGO) stage and lymphatic invasion at the time of diagnosis, as well as increased metastatic spread, compared to their HPV-positive counterparts[7]. Due to the rarity of HPV-negative cervical cancer, there is lack of research and minimum information on diagnosing and treating this type of cervical cancer.
CASE PRESENTATION
A seventeen-year-old female patient presented with a six-week history of vaginal bleeding in January 2014. She had been previously treated with oral contraceptives, but her symptoms continued to persist. Her familial, medical history was unremarkable. Upon physical examination, a moderately pale, well-hydrated teenager without jaundice, fever, pedal edema, or palpable peripheral lymph nodes was observed. The physical examination also revealed an intact hymen since the patient claimed to have no history of any sexual encounter. Due to the bleeding, a transabdominal ultrasound scan was performed which revealed a heterogenous hyperechoic cervical mass measuring 4.5 x 2.0 cm. The presence of the mass was also confirmed through a digital rectal examination. Additionally, partial parametrial involvement was also identified during the rectal examination.
Decision was made to carry out a biopsy since the findings from the ultrasound were highly suggestive of malignant neoplasm. Biopsy of the cervical mass revealed an undifferentiated malignant tumour of the cervix with lymphovascular invasion. A cervical cytology HPV testing was carried out which was negative. Other tests for sexually transmitted infections such as HIV, syphilis, hepatitis B and C were carried out which came back negative. Oncological markers such as CA 125 and CEA were within normal ranges. An abdominopelvic Computed Tomography scan was carried out which revealed a cervical mass as well as the absence of the left kidney. The mass was confined to the cervix with suggestion of lymphovascular involvement or pelvic extension.
A multi-disciplinary team involving surgeons, radiation oncologist, radiation therapists was involved in the management of the case. There was a notion to try and preserve fertility due to the young age of the patient. However, fertility preservation would be difficult due to the stage of the disease as well as parametrial involvement of the disease. Therefore, fertility preserving surgeries such as extrafascial hysterectomy or radical trachelectomy were not considered, and modified radical hysterectomy proved to be the best option. There was also a concern of a higher risk of complication if two or more radical therapies were combined, that is surgery, radiation treatment as well as chemotherapy. The team then noted that adjuvant radiotherapy had been recommended in literature after radical hysterectomy if there were parametrial involvement, positive surgical margins, or pelvic lymph node metastases, and it should be considered if there is a combination of lymphovascular space invasion, tumor size greater than 2 cm, and deep invasion[8]. Therefore, adjuvant radiotherapy was elected as the next mode of treatment following the hysterectomy since the patient’s disease included parametrial involvement, lymphovascular invasion, and her tumor was around 4.5 cm in size. Concomitant chemotherapy was also considered due to the metastatic nature of the disease stage.
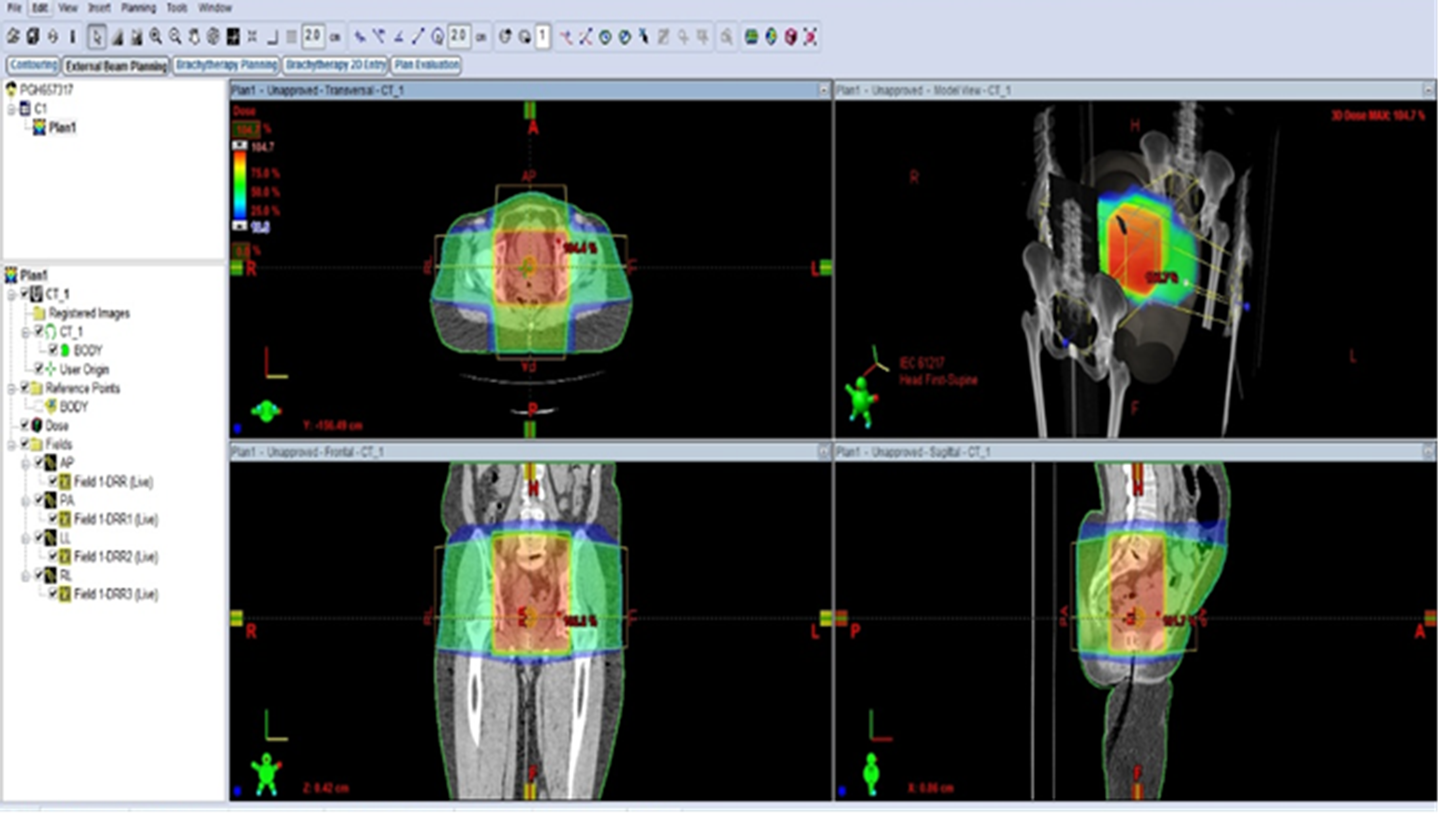
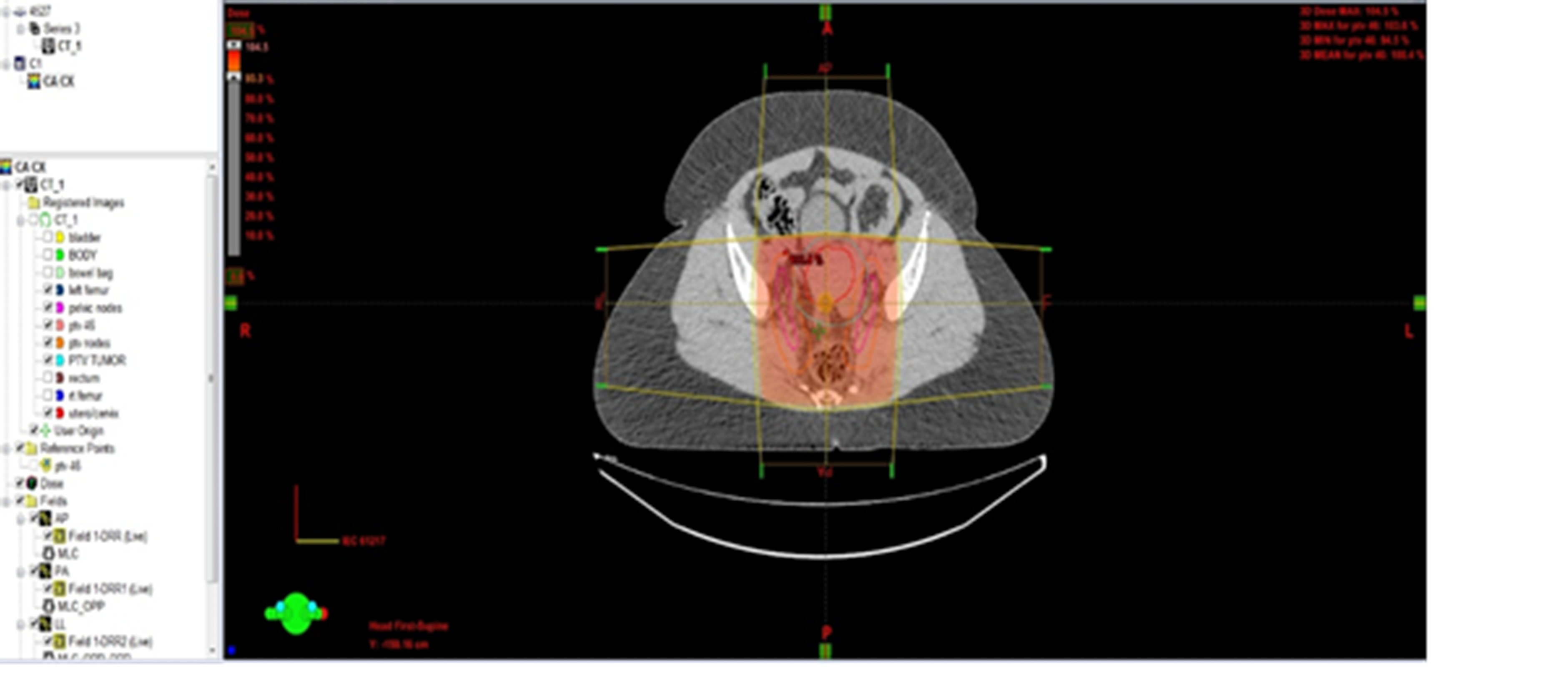
The patient proceeded to undergo radical abdominal hysterectomy, ovarian transposition as well as pelvic lymph node dissection. The final histological analysis of the tumour revealed a high-grade cervical adenocarcinoma, with lymphovascular involvement of the parametria. The dissected pelvic lymph nodes were free of disease. The malignancy was classified as FIGO stage IIB due to the parametrial involvement. The patient was then referred to Parirenyatwa Radiotherapy Centre for adjuvant oncological treatment, where adjuvant chemoradiotherapy was prescribed to the patient. An external beam radiation therapy dose of 50.4 Gy in 28 fractions at 1.8 Gy per fraction over seven weeks, as well as 21 Gy in 3 fractions at 7 Gy per fraction for intracavitary brachytherapy for three weeks was prescribed to the patient. The patient underwent EBRT from 29 May 2014 to 11 July 2014. The brachytherapy treatments were administered on 30 June, 4 July and 8 July of that same year. She received radio-sensitising chemotherapy in the form of cisplatin and paclitaxel weekly for six weeks concomitantly. Excellent response to the treatment was noted by the presiding oncologists.
The patient was followed up after six weeks, monthly for two months, and then every three months. She then presented with kidney failure due to radiation nephropathy in early 2016. Her health rapidly deteriorated and she deceased that same year, almost two years after diagnosis.
DISCUSSION
This case of cervical cancer developing in a virgin is a very interesting case in terms of its extreme rarity and atypical clinical course. The patient presented here is also one of the youngest reported patients in Zimbabwe to be treated at this radiotherapy centre.
Invasive cervical cancer is very rare in women younger than 21 years. Only 0.1% of cervical cancer occurs before age 21 years[5]. The incidence of cervical cancer in 15 to 24-year-olds is low[9]. This situation can be explained by the natural history of the HPV type of the disease.
The case contradicts our understanding that almost all cervical cancer is due to sexually transmitted HPV. The occurrence of cervical cancer in individuals who have not had sexual intercourse or within eight years of first intercourse could suggest the presence of an uncommon form of cervical cancer not linked to HPV. It is probable that we were addressing an HPV-negative type of cervical cancer. Several potential mechanisms for carcinogenesis could be proposed to account for this exceptional case:
Initially, there are potential ways in which cervical cancer could develop, involving temporary participation of HPV, known as a "hit-and-run" mechanism. Nevertheless, the "hit-and-run" mechanism seems improbable, as the expression of E6 and E7 oncoproteins of high-risk HPV is necessary to sustain the transformation of cervical epithelial cells[10]. There is only a single case that seems to be associated with this mechanism.
The link between being exposed to diethylstilböstrol (DES) and the development of adenocarcinoma of the vagina or cervix is well-documented in the literature. A similar case report[11] noted that young women who have not had sexual intercourse can develop cervical cancer as a result of being exposed to diethylstilboestrol in the womb. The report[11] mentioned that DES, a synthetic version of estrogen, was given to expectant mothers from 1940 to 1971 to avoid miscarriage, early childbirth, and labour-related issues until it was banned. It was prohibited due to its adverse side effects, which included the development of cancer. Based on the patient's provided information, her mother was pregnant between 1996 and 1997. Therefore, DES could not have caused the patient's cervical cancer.
The development of cervical carcinoma may occur through pathways that are not dependent on HPV, as suggested by epidemiological evidence showing that patients with HPV-negative cervical intraepithelial neoplasia (CIN) exhibit different risk factors compared to those with HPV-positive CIN. The p53 molecule is implicated in the HPV-independent carcinogenesis of the uterine cervix. While most p53 dysfunctions in cervical cancer are associated with the E6 oncoprotein of high-risk (HR)-HPV, other mechanisms such as point mutation or genetic polymorphism could lead to malignant transformation through an HPV-independent process. According to a report on HPV-negative cervical cancer, it was discovered that p53 mutation was more prevalent in HPV-negative cervical cancers compared to HPV-positive ones. It was found that 71% of HPV-negative cervical cancer cases exhibited an abnormal p53 immunostaining pattern with p16 overexpression[7]. Another study by Petitijean, et.al[12] demonstrated a strong association between p53 mutation and a poor prognosis, which may explain why HPV-negative cervical cancer tends to have more aggressive characteristics, such as advanced FIGO stage, a higher rate of metastasis, and a poorer prognosis compared to HPV-positive cervical cancer[12]. Therefore, it is speculated that HPV-negative cervical cancer may emerge from the de novo mutation of p53, without the presence of HR-HPV DNA.
The diagnosis of cervical cancer in virgins presents with adverse psychological effects especially in virgins. Surgical interventions to combat cervical cancer may involve the complete removal of the uterus, fallopian tubes, ovaries, the upper portion of the vagina, and the lymph nodes. These organs are all involved in pregnancy, childbirth, and sexual activity[13]. Other treatments for cervical cancer, like radiation therapy and pelvic exenteration, also impact the reproductive system. The patient presented in our case underwent surgery as well as radiation therapy hence there was need for strong psychological support and counselling.
Unfortunately, the patient passed away in 2016, approximately eighteen months after the initial diagnosis. Sources indicate that she was mostly in good health during the period between completing treatment and her passing, and then suddenly fell ill and passed away. Although there are few cases documented in the literature, the reported instances have tended to be fatal. A similar case report from Portugal[14] documented an eighteen-year-old patient who succumbed to the disease fourteen months after diagnosis despite oncological evaluation and treatment. Another West African case report[5] documented a seventeen-year-old patient whose diagnosis was Stage IIB squamous cell carcinoma of the cervix who received radiotherapy and chemotherapy but defaulted further treatment. She presented four months later to the clinic with disease progression and deceased six months after initial presentation. The fatality of these HPV-negative cervical cancers remains unclear whether this is due to delayed diagnosis or the more aggressive nature of these tumours[15]. This rare tumour probably evades all current screening methods, whether based on Pap smear or HPV testing.
CONCLUSION
In conclusion, this case report sheds light on the possibility of cervical cancer in virgins being attributed to factors other than HPV infection. It underscores the potential risk of overlooking cervical cancer in virgins, which may lead to late-stage diagnosis. The rarity of cervical cancer in virgins, coupled with the challenge of suspicion and lack of established guidelines for diagnosis in this demographic, highlights the importance of vigilant clinical judgment.
Screening methods involving invasive procedures like PAP smears pose a dilemma for virgin patients, emphasizing the need for clinicians to navigate such situations carefully and remain vigilant for rare occurrences to ensure timely diagnosis and treatment. If this cancer was independent of HPV, then it means HPV vaccination will not be effective in such cases. This becomes a dilemma in coming up with preventive measures for such types of cervical cancer.
Counselling is also essential in cases like these. Patients should receive relevant information in a non-intimidating manner to aid their understanding of their condition. Providing patients and their families with pre-counselling before treatment can help them prepare for what to expect and explore effective coping strategies. Therapeutic approaches like cognitive-behavioural therapy can offer significant support, as they challenge the patient's unique thought patterns to reduce depression and anxiety. Additionally, techniques such as relaxation training and cognitive stress coping can also prove beneficial.
Ethical Considerations
Permission to access patient information was received from the chief radiographer at the radiotherapy centre where the patient received oncological treatment. Ethical clearance was obtained from the School of Allied Health Sciences certificate number 2022/0012. Approval from the Medical Research Council of Zimbabwe was unnecessary because this was done retrospectively without involving patients, but only patient records were used. Patient confidentiality was respected, since the name of the patient or contact details remained anonymous. No consent form was given to the patient since the patient had already deceased by the time the case report was written. The ethical clearance was awarded because the information in the case report does not disclose the patient's identity, and no harm will be caused to the remaining family members. Publication of this case will contribute positively to the future management of the rare type of cervical cancer in virgins.
Conflicts of Interest
Authors declared they have no conflicts of interest.
Author Contributions
T. Motsi was responsible for case identification and initial write-up. E.Y. Mushosho supervised the case and realigned it for publication. B. Chinene did plagiarism checks, editing, and formatting of the paper.
REFERENCES
- Bruni L, Albero G, Serrano B, Mena M, Collado JJ, Gomez D. Human Papillomavirus and Related Diseases in Zimbabwe, s.l.: ICO/IARC HPV Information Centre. 2019. 18-26.
- Kuguyo O, Matimba A, Tsikai N, Mugwali T. Cervical cancer in Zimbabwe: a situation analysis. PanAfrican Medical Journal. 2017. ISSN: 1397-8688.
- Sasagawa T, Takagi H, Makinoda S. Immune response against human papillomavirus (HPV) infection and evasion of host defence in cervical cancer. Journal of Infection and Chemotherapy. 2012. 18:807-815.
- World Health Organization. Cervical cancer common amongst African women. World Health Organization Regional Office for Africa: 2017.
- Roberts O.A, Owohikoko K.M, Abdus-Salam A.A, Ogun O. Advanced cervical carcinoma in a 17-year-old girl. Department of Obstetrics and Gynaecology, College of Medicine. University of Ibadan. 2017. DOI: 10.3109/01443615.2013.813911.
- Arezzo F, Cormio G, Loizzi V, Cazzato G, Cataldo V, Lombardi C, Ingravallo G, Resta L, Cicinelli E. HPV-Negative Cervical Cancer: A Narrative Review. Diagnostics. 2021;11, 952. https://doi.org/10.3390/diagnostics11060952.
- Lee JE, Chung Y, Rhee S, Kim TH. Untold Stories of human cervical cancers: HPV-negative cervical cancer. BMB Reports. 2022.; 55(9):429-438. https://doi.org/10.5483/BMBRep.2022.55.9.042.
- Carter J and Randall LM. Radical Hysterectomy Treatment and Management. Medscapes. Updated 2022. https://emedicine.medscape.com/article/270723-treatment?form=fpf.
- NHS Screening Programs. Guidelines from NHS Cervical Screening Program. 2010.
- Shim A.R, Choi E.K, Yun S.H, Lee M, Lee M.K, Kim S.W. A case of squamous cell carcinoma of the uterine cervix with diffuse hematogenous lung metastasis in a 36-year-old virgin. Korean Journal of Obstetrics and Gynaecology. 2011; 54(10):634-638.
- Lee YL, Chang KH, Kyung MS, Kim HB, Park S. A case of clear cell adenocarcinoma in the uterine cervix of 52-year-old virgin, Seoul: Korean Journal of Obstetrics and Gynaecology. 2012: 55(3): 192-196.
- Petitjean A, Achatz MI, Borresen-Dale AL, Hainaut P, Olivier M. TP53 mutations in human cancers: functional selection and impact on cancer prognosis and outcomes. Oncogene. 2007;26, 2157-2165.
- Monesa, N. A Critical Literature Review of the Psychological effects of cervical cancer. Mini-Dissertation for Master’s in Psychology in the faculty of Arts at Rand Afrikaans University. 2003. 48-49.
- Pestana I, Costa A, Gorgal R, Mota R, Portugal R, Paiva V. Cervical uterine cancer in a virgin young woman- Case Report. Journal of Obstetrics and Gynaecology. 2014. Early Online 1-2.
- Liebrich C, Wegener G, Iftner T, Petry K.U. Primary Cervical Cancer truly negative for high-risk human papillomavirus is a rare but distinct entity that can affect virgins and young adolescents. European Journal of Gynaecological Oncology. 2009. ISSN 0392-2936.
Medical Journal of Zambia, Vol 51, 3
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.