A Sigmoid Vaginoplasty in a Patient with Vaginal Agenesis in a low resource country: A Case Report from Zambia
Edah Monjeza
University Teaching Hospitals- Women & Newborn Hospital, Nationalist Road, Lusaka, Zambia
Goshon Kasanda
University Teaching Hospitals- Women & Newborn Hospital, Nationalist Road, Lusaka, Zambia
Mwansa Ketty Lubeya
University Teaching Hospitals- Women & Newborn Hospital, Nationalist Road, Lusaka, Zambia
DOI: https://doi.org/10.55320/mjz.52.1.536
Keywords:Vaginoplasty, Vaginal Agenesis, Intestinal neovagina, FSFI, Psycho-social Status
ABSTRACT
Vaginal agenesis is a rare condition affecting several females that present with amenorrhoea and unexplained abdominal pain. While it can be a cosmetic issue, it does affect the lives of individuals. We explored the surgical outcomes of a sigmoid vaginoplasty in a 22-year-old female who presented with primary amenorrhoea and lower abdominal pain. We discussed the case, procedural steps, postoperative management, and patient outcomes. The management of vaginal agenesis using a sigmoid vaginoplasty was dependent on the patient’s presentation, their sexual activity and social needs. A female sexual function index (FSFI) was used to assess the functionality of the neovagina which corresponded to the success of the operation. The purpose of this case report is to highlight the postoperative sexual functionality following the sigmoid vaginoplasty. Furthermore, vaginoplasties should be considered as an appropriate route for management of vaginal agenesis in Zambia.
INTRODUCTION
Vaginoplasty is a rising procedure in the field of medicine[1] being used to create, repair, or correct vaginal agenesis, imperforate hymen, atresia of the lower one-third of the vagina, and gender affirmation.[2] Some of the types of vaginoplasty procedures include the McIndoe technique, which involves the usage of a skin graft, a peritoneal vaginoplasty, which uses a portion of the peritoneum, a buccal mucosa vaginoplasty involving the use of the lining of the oral cavity and the intestinal vaginoplasty that uses a portion of the sigmoid colon to create a neovagina and this can be done laparoscopically or exploratively.[3], [4], [5], [6] The most well-known procedure is the McIndoe vaginoplasty.[7] However, no agreement has been reached concerning the best strategy for making a functional neovagina. For now, the intestinal vaginoplasty appears to be encouraging and more information is required for it to acquire general acknowledgment. The sigmoid vaginoplasty has a wide range of advantages over the other methods; it is near the perineum, it can easily be mobilized on its vascular pedicle, it requires minimal dilation and has a low risk of stenosis. It is self-lubricating and produces less mucus compared to the small intestines. This results in a cosmetically acceptable neovagina with a good length.[8]
Vaginal agenesis, which is a defect in the female reproductive system, involves the congenital malformation of the mullerian ducts.[9] It occurs in 1 per 4,500 - 5,000 females.[10] A female sexual function index (FSFI)[11] was used to assess the functionality of the neovagina because of its clear wording and particular detail to psychometric properties, which can be used to correspond to the success of the operation. We present the case of a young adult female with Mullerian agenesis who was managed at a level one hospital in Lusaka Zambia.
CASE PRESENTATION
A 22-year-old female presented with primary amenorrhoea and abdominal pain. The patient reported she was unable to have penetrative sexual intercourse, she also gave a history of having two previous sexual partners and this affected her relationships. On examination, the patient had a short stature, normally developed breasts, and a blind-ending vagina approximately 3-4cm on digital vaginal examination. Ultrasound scans were done that revealed the presence of ovaries but an absent uterus.
She was scheduled for a sigmoid vaginoplasty and the procedure lasted two hours and thirty minutes. During the post-operative period, she reported using vaginal dilators for four weeks and she reported having successful penetrative vaginal sexual intercourse. The patient was carefully counselled about the operation, fertility aspects were discussed and that the purpose of the procedure was purely coital. Possible In-Vitro Fertilization (IVF) with a surrogate mother was suggested as option, as was adoption.
Pre-operative preparations
Besides other preoperative preparations, the bowel was completely emptied before surgery. The patient was catheterized, and intravenous metronidazole and Ceftriaxone were given for prophylaxis against bacterial infection.
Surgical procedure
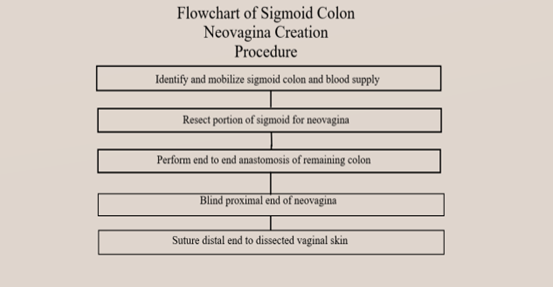
The procedure was done under general anaesthesia with the patient in stirrups to enable access to both the vagina and abdomen and dissection vaginally into the recto-vesical space for the neovagina was carried out.

On the abdominal aspect, the length of the sigmoid colon was identified, mobilized, and isolated with its major blood supply. Resection of the portion of the sigmoid that needed to be used as a neovagina was done both proximal and distal while maintaining blood supply to the cut segment.
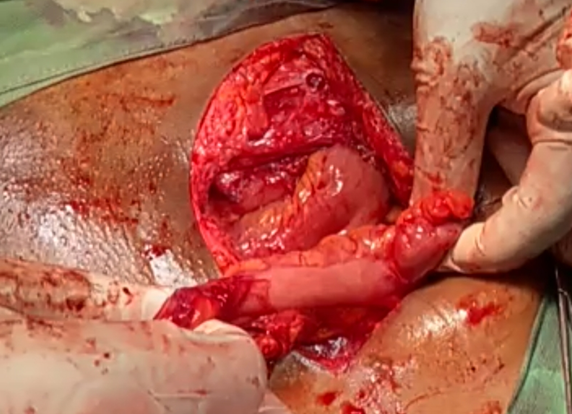
End-to-end anastomosis of the remaining sigmoid was done while leaving it lateral to the neovaginal segment of the colon that was rotated 180 degrees to reduce tension on the neovaginal portion. The proximal end of the neovagina was blinded and suspended on the inferior longitudinal spinal ligament at the level of the promontory. The distal end of the segment was passed to the perineum through the already created perineo-peritoneal space and sutured to the dissected vaginal skin. Abdominal lavage was done before closing the abdomen.
Post Operation
The neovagina was found to have a good cosmetic appearance. The patient did not experience any immediate or long-term complications like stenosis, altered intestinal habits, bowel prolapse or infection.
DISCUSSION
The management of Mullerian agenesis using sigmoid vaginoplasty is highly dependent on the patient's presentation, putting into consideration whether they are sexually active as well as their social needs.[12] Historically, the length of the neovagina was commonly used as a measure of vaginoplasty outcomes[13] but deemed to be inconclusive on the general sexual satisfaction status of the women. Comparing the length on presentation (3-4cm) to the most ideal length anatomically at ≥ 8cm-9cm[14], a sigmoid vaginoplasty demonstrates a significant improvement. However, it is important to consider other aspects that can better assess the outcomes of the procedure.
The quality of life can be a suitable aspect to consider when assessing the success rate of this procedure. Looking at the fertility needs of the women undergoing this treatment option, informed consent is cardinal to the management, outlining the fertility choices that women of childbearing age have after undergoing the procedure, especially in this patient's case, with a presentation of an absent uterus on abdominal ultrasound places our patient in the spectrum of individuals with vaginal agenesis that have fertility issues. Adequate counselling was done listing out the options the patient had for having children such as surrogacy and adoption which have proven to be of great success.
A FSFI score questionnaire was used on this patient. It is a 19-part questionnaire that was created as a multi-layered, concise and self-report instrument for surveying the critical components of sexual functionality in females. It was used in this case because it is psycho-metrically sound, simple to administer and is easily understood by a wide range of populations. Six domains were assessed in this scoring system: desire, arousal, orgasm, lubrication, satisfaction, and pain. Each domain had a maximum score of 6.0, the scoring tool had a full-scale score of 36.0, and an ideal cutoff score of 26.55 to tell apart women with sexual dysfunction from women without sexual dysfunction.[15] Our patient had a final scale score of 26.7 out of 36.0. She scored highest in the satisfaction domain at 6.0, obtaining 4.8 in the arousal domain, 4.5 in lubrication, 4.2 in the desire domain, and lowest in the orgasm and pain domains both at 3.6. The results portrayed by our patient explain the status of the sexual functionality of the neovagina. It showed overall satisfaction with moderate levels of arousal, desire, and a significant amount of lubrication. However, it recorded significant levels of dyspareunia and lower chances of achieving orgasm. The final scale score signifies sexual function in correspondence with the ideal cutoff score. The FSFI scores of this patient helps us understand the postoperative functionality of the neovagina and we can conclude that there were good operative outcomes.
Involving the women's sexual partners in the assessment of the outcomes can give insight into the success rate. The patient reported having overall satisfaction in her sexual relationships. She also reported increased levels of confidence after having the surgery.
According to the American College of Obstetricians and Gynaecologists (ACOG), to diagnose mullerian agenesis, the following can be done; karyotype, magnetic resonance imaging (MRI) which can confirm endometrial activity, testosterone level, ultrasonography and follicle stimulating hormone (FSH) level.[16] The inability to fully diagnose in this case was a consequence of lack of resources. Low resource income countries face difficulties with fully diagnosing this condition hence resorting to using only the resources that are present.
It is important to consider counselling, the availability of support groups for patients as well as access to a medical summary explaining their condition and any other factors related to it. The ability and skill of the surgeon is also an important factor to consider when dealing with this condition. Referring patients to good facilities with skilled personnel can foster excellent results and a quick recovery with few follow ups.
CONCLUSION
This case is one out of the many presentations of vaginal agenesis, the management and overall outcomes of the procedure demonstrated positive results in the general sexual functionality of the neovagina. Mullerian agenesis is a rare condition. Patients in resource limited settings can benefit from patient education with an emphasis on sexual health and prioritizing personnel training. The assessment of the procedure and observation for any complications related to the surgical operation allowed for this procedure to be considered as a satisfactory technique in the management of vaginal agenesis.
Limitations
We only reported one of the many cases of mullerian agenesis managed by a sigmoid vaginoplasty hence, not having an appropriate comparison group.
Consent
Written informed consent was obtained prior to this case report being authored.
REFERENCES
- Li, J. S., Crane, C. N., & Santucci, R. A. (2021). Vaginoplasty tips and tricks. International Braz J Urol, 47(2), 263–273. https://doi.org/10.1590/S1677-5538.IBJU.2020.0338
- Ruggeri, G., Gargano, T., Antonellini, C., Carlini, V., Randi, B., Destro, F., & Lima, M. (2012). Vaginal malformations: a proposed classification based on embryological, anatomical and clinical criteria and their surgical management (an analysis of 167 cases). Pediatric Surgery International, 28(8), 797–803. https://doi.org/10.1007/s00383-012-3121-7
- Bhaskar, V., Sinha, R. J., Mehrotra, S., Mehrotra, C. N., & Singh, V. (2018). Long-term outcomes of sigmoid vaginoplasty in patients with disorder of sexual development - our experience. Urology Annals, 10(2), 185–190. https://doi.org/10.4103/UA.UA_88_17
- Castanon, C. D. G., Matic, S., Bizic, M., Stojanovic, B., Bencic, M., Grubor, N., Pusica, S., Korac, G., & Djordjevic, M. L. (2022). Laparoscopy Assisted Peritoneal Pull-Through Vaginoplasty in Transgender Women. Urology, 166, 301–302. https://doi.org/10.1016/j.urology.2022.05.001
- Chan, J. L., Levin, P. J., Ford, B. P., Stanton, D. C., & Pfeifer, S. M. (2017). Vaginoplasty with an Autologous Buccal Mucosa Fenestrated Graft in Two Patients with Vaginal Agenesis: A Multidisciplinary Approach and Literature Review. Journal of Minimally Invasive Gynaecology, 24(4), 670–676. https://doi.org/10.1016/j.jmig.2016.12.030
- Karateke, A., Haliloglu, B., Parlak, O., Cam, C., & Coksuer, H. (2010). Intestinal vaginoplasty: seven years' experience of a tertiary centre. Fertility and Sterility, 94(6), 2312–2315. https://doi.org/10.1016/j.fertnstert.2010.01.004
- Keser, A., Bozkurt, N., Taner, O. F., & Sensöz, O. (2005). Treatment of vaginal agenesis with modified Abbé-McIndoe technique: long-term follow-up in 22 patients. European Journal of Obstetrics, Gynaecology and Reproductive Biology, 121(1), 110–116. https://doi.org/10.1016/j.ejogrb.2004.11.027
- Rajimwale, A., Furness, P. D., 3rd, Brant, W. O., & Koyle, M. A. (2004). Vaginal construction using sigmoid colon in children and young adults. BJU international, 94(1), 115–119. https://doi.org/10.1111/j.1464-4096.2004.04911.x
- ACOG Committee on Adolescent Health Care (2006). ACOG Committee Opinion No. 355: Vaginal agenesis: diagnosis, management, and routine care. Obstetrics and Gynaecology, 108(6), 1605–1609. https://doi.org/10.1097/00006250-200612000-00059
- Evans, T. N., Poland, M. L., & Boving, R. L. (1981). Vaginal malformations. American Journal of Obstetrics and Gynaecology, 141(8), 910–920. https://doi.org/10.1016/s0002-9378(16)32683-7
- Opperman, E. A., Benson, L. E., & Milhausen, R. R. (2013). Confirmatory factor analysis of the female sexual function index. Journal of Sex Research, 50(1), 29–36. https://doi.org/10.1080/00224499.2011.628423
- Delshad, S., Delshad, B., & Mogheimi, P. (2022). Postoperative outcomes of sigmoid colon vaginoplasty for vaginal agenesis: A randomized controlled trial. Annals of Medicine and Surgery (2012), 78, 103833. https://doi.org/10.1016/j.amsu.2022.103833
- McQuillan, Sarah & Grover, Sonia. (2014). Systematic review of sexual function and satisfaction following the management of vaginal agenesis. International Urogynaecology. 25. 10.1007/s00192-013-2316-3
- Kölle A, Taran FA, Rall K, Schöller D, Wallwiener D, Brucker SY. Neovagina creation methods and their potential impact on subsequent uterus transplantation: a review. BJOG. 2019 Oct;126(11):1328-1335. doi: 10.1111/1471-0528.15888. Epub 2019 Aug 13. PMID: 31338951.
- Wiegel, M., Meston, C., & Rosen, R. (2005). The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. Journal of Sex & Marital Therapy, 31(1), 1–20. https://doi.org/10.1080/00926230590475206
- ACOG Committee Opinion No. 728 Summary: Müllerian Agenesis: Diagnosis, Management, And Treatment. (2018). Obstetrics And Gynaecology, 131(1), 196–197. https://doi.org/10.1097/AOG.0000000000002452
Medical Journal of Zambia, Vol 52, 1
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.