Is It Possible to Miss a Metallic Airway Foreign Body on a Chest Radiograph? Imaging Case Report from Zambia
Osward Bwanga
Midlands University Hospital Tullamore, Radiology Department, Co. Offaly, Ireland
Mulewa Mulenga
Arthur Davison Children's Hospital and Copperbelt University, Ndola, Zambia
Ethel C. Jere
Arthur Davison Children's Hospital, Radiology Department, Ndola, Zambia
James M. Sichone
University of Zambia, School of Health Sciences, Radiography Section, Lusaka, Zambia
DOI: https://doi.org/10.55320/mjz.49.1.1111
Keywords: Aspirated foreign body, Children, Medical imaging, Radiographer, ZambiaABSTRACT
Infants and young children are commonly referred for medical imaging for suspected aspirated or inhaled foreign bodies (Fbs). FB aspirations are potentially life-threatening and immediate diagnosis and treatment are vital to avert fatalities. Chest radiography is the first-line imaging method indicated to evaluate suspected aspirated FB. This can be supplemented withothermedical imaging modalities, such as fluoroscopy, computed tomography (CT), and magnetic resonance imaging (MRI). However, the lack of specialised medical imaging modalities in developing countries impends timely diagnosis of aspirated FB. We report a case of a 7-year-old girl with airway metallic FB not visible on the initial chest radiograph. This case report highlights the challenges low-income health institutions are facing in the diagnosing of airway FBs and other complicated conditions which require advanced imaging. In the absence of specialised medical imaging modalities, radiographers and clinicians should have high indexes of suspicion to avert deaths. In addition, specialised training of radiographers in the absence of radio lo gists might contribute to improved patient outcomes.
INTRODUCTION
Aspiratedor inhaled foreign bodies (Fbs) are a common emergency referral for medical imaging in children. Infants and young children habitually place objects into their mouths, are mostly playful and active when eating and do not have developed dentition to chew food properly. 1, 2 The objects that children place in their mouths sometimes can lodge in the airway resulting in serious complications or even leading to death.2, 3 Complications of delayed FB removal include recurrent pneumonia, pneumothorax, lung collapse, bronchomalacia, empyema thoracis, and mediastinitis.3, 4 Medical imaging plays an important role in diagnosing and managing aspirated FBs. However, in life-threatening situations, medical imaging should not delay intervention, bronchoscopy should be performed immediately as is the management of choice in removing an airway FB.2, 5
Chest radiography is the first-line and most important imaging examination in the diagnosis of an aspirated FB.2, 6, 7 The recommended projections are posterior-anterior (PA) and lateral views of the chest.27 A lateral projection gives a further view of the chest and more details on the anatomical location of the FB: anterior, midline, or posterior. The collimated beam on the frontal chest radiograph should include a neck (patient's head turned to one side) to ensure the FB is not located in the nasopharynx or oropharynx. 7 However, literature reports that 30% to 40% of the patients with airway Fbs have a normal chest radiograph.2, 4, 5, 8 In this regard, other specialised imaging modalities, such as fluoroscopy, computed tomography (CT), and magnetic resonance imaging (MRI) can be performed to confirm the diagnosis.1, 2, 8, 9 Therefore, clinicians should be well-informed about the range of medical imaging modalities that can be used to evaluate different types of aspirated Fbs.
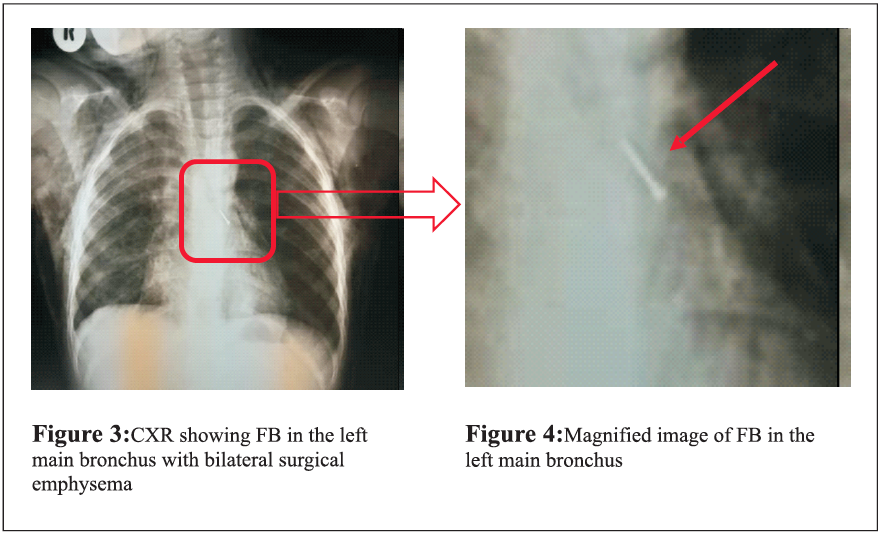
FBs are commonly aspirated into the right tracheobronchial tree in older children and adults because of the wider and steeper structure of the right main bronchus.5, 7, 8, 9 However, the tracheal bifurcation in infants is more central, and FBs may be seen equally in the left and right main bronchi.1, 5 There is a scarcity of case reports on this subject from a medical imaging perspective. The common cases reported on this subject are from and empyema thoracis was made by the attending clinicians. Bilateral underwater seal intercostal drainages (ICDs) (Figure 2) were inserted, and the patient was put on treatment. When the patient was presented to the primary hospital, no report of FB aspiration was made,and neither did the initial chest radiograph (Figure 1) demonstrate any FB in the airway. The patient's condition did not improve despite the ICDs and treatment. Therefore, the patient was referred to ADCH for further management.
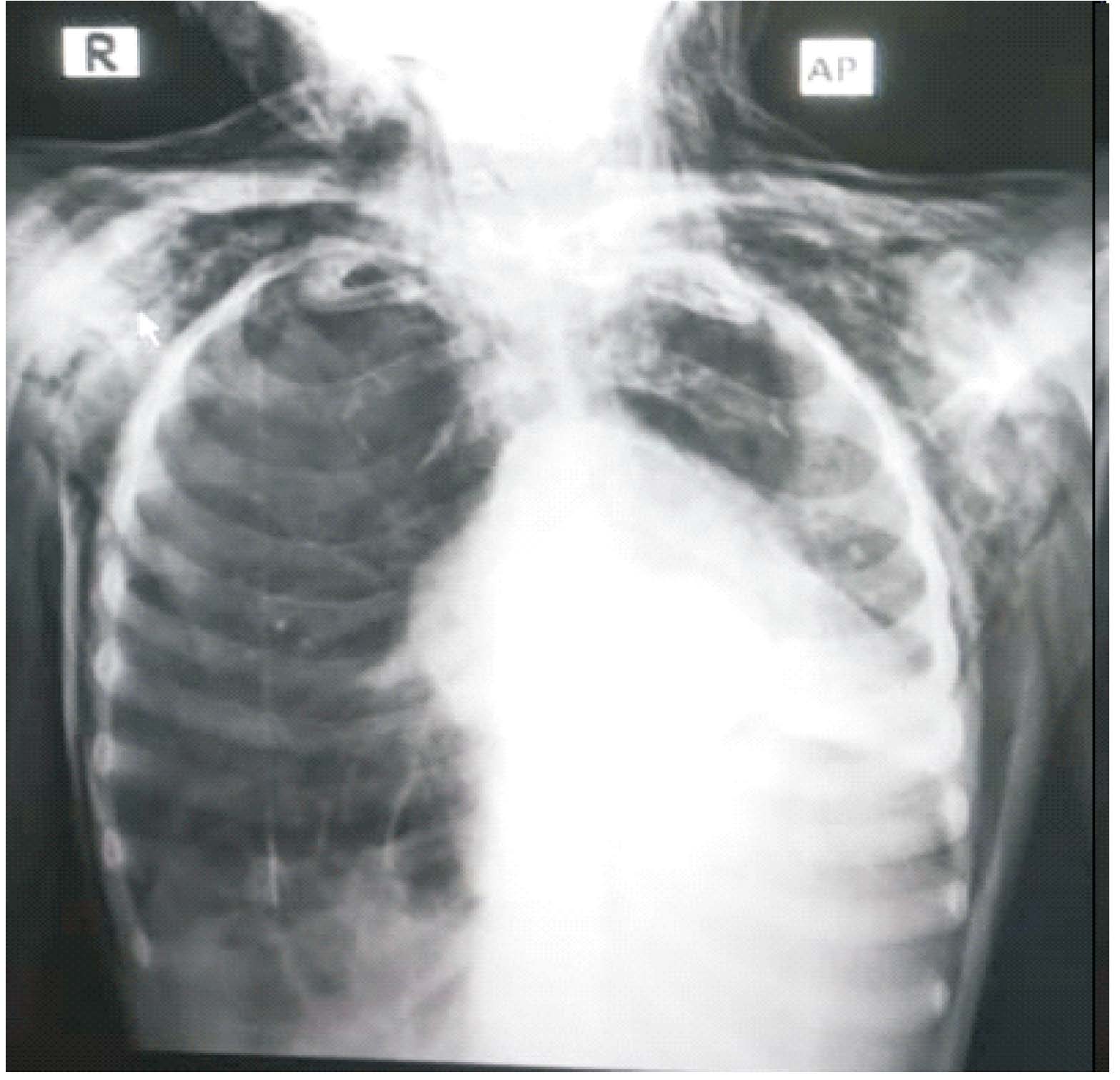

Following admission and clinical assessment, the consultant surgeon suspected the FB in the airway as the main cause of the child's illness. A repeat chest X-ray was requested a day after admission to exclude FB. The patient came to the radiology departmentaccompanied by her mother and thenurse. Clinical details on the radiology request form (RRF)read, "secondary pneumonia and surgical emphysema with suspected foreign body" for chest X-ray. The imaging room was prepared, and the procedurewas explained to the patient and the mother. This included the rehearsal of the breathing techniques. The patient came in the hospital gown, and before imaging, the radiographer ensured that no confusing opacities were present on clothing, on the skin, or erect bucky of the X-ray equipment. An AP projection of the chest, with the patient seated on the specialised imaging stool,was performed using a conventional X-ray machine and cassette. The X-ray film was processed, and the radiograph (Figure 3) was assessed for quality and given to the nurse.

DISCUSSION
In this case report, chest radiography was used to diagnose an aspirated metallic FB in the left main bronchus of a child referred to ADCH for further management. This agrees with the literature that reports that chest radiography should be the first imaging examination in diagnosing aspirated FBs.2, 4, 6, 7, 9 The exammatlon is painless, fast, and non-invasive.2 In addition, it is cheaper and commonly available in most medical facilities when compared with cross-sectional modalities, such as CT and MRI. However, chest radiography can at times be non-revealing in the evaluation of airway FB.49 Our case revealed similar findings were inflammatory changes in the lung parenchyma, the airway, and complications that arose masked the FB. Hence, the FB was missed on the initial chest radiograph (Figure 2). Other factors that can contribute to missed FB on plain X-rays include insufficient information on the radiology request form (RRF), poor patient positioning during imaging, inadequate image penetration, inappropriate techniques, and a lack of trained 'Eyes' to evaluate images. 2, 6, 12
The medical imaging method chosen to demonstrate the presence and position of a FB depends on the opacification of the material.2 Radiopaque (inorganic) materials, such as teeth, coins, and pins or nails are easily demonstrated, whilst radiolucent (organic )materials, such as nuts, and seeds are not easily demonstrated on the radiograph. Therefore, the diagnosis of FB aspiration by imaging is challenging because between 70% and 80% of aspirated FBs, such as seeds, and nuts are radio lucent. 59For this reason, radiologists, reporting radiographers, and referring clinicians rely on secondary signs, such as the 'ball valve effect' to make the diagnosis.1, 4 FB lodged within the main bronchus results in persistent hyperinflation of the affected lung or lobe because of the 'ball valve effect' where the air is allowed to enter the lung on inspiration but is obstructed and unable to leave the lung on expiration. 1, 6, 12 Although most aspirated FBs are radiolucent, chest radiography should be performed to aid in the identification of any possible associated collapse or consolidation of the lung.6
In our case report, film-screen radiography (FSR) was used for image capture which is currently available at ADCH. The main disadvantage ofFSR is the lack of post-processing capabilities, such as image magnification, edge enhancement, and windowing tools that can make the presence of a FB more easily visualised. 2, 6 These post-processing features are only available in Digital Radiography (DR) systems: Computed Radiography (CR) and Direct Digital Radiography (DDR). DR offers more benefits than FSR. In the absence of a digital imaging system, there is a need for radiographers to pay close attention and in some instances vary their technique by increasing the penetration and undertaking additional views. 2, 6, 13
Fluoroscopy is another medical imaging modality that can be used in suspected FB aspiration.2, 4, 9 Patel5 states that in case there is a high suspicion of FB aspiration by an infant or toddler, and the chest radiograph is normal, fluoroscopy can be performed. Fluoroscopy has the advantage of providing real-time images of the internal structures of the patient and allows appreciation of the FB from various aspects, while conventional radiographyis limited to two (2) orthogonal plains. 14 The fluoroscopy equipment is also cheaper than other cross-sectional modalities, such as CT and MRI. The non-availability of the fluoroscopy imaging services at the primary hospital and ADCHlimited the diagnosis of airway FB and delayed the treatment of the patient.
Literature also reports that cross-sectional imaging modalities, such as CT and MRI can supplement general radiography and fluoroscopy.2, 4, 7 CT and MRI may be used when it is necessary to demonstrate the FB relative to the internal organs, and any damage to the surrounding structures may have occurred on account of the FB.2, 4, 8, 9 However, MRI should only be used for non-metallic FBs because of the magnetic nature of the imaging modality of attracting metallic objects which can cause internal body injury.2 Unfortunately, CT and MRI are not available at ADCH. These advanced imaging modalities are crucial in the delivery of quality imaging services.
The services of a radiologist are crucial in the timely diagnosis of aspirated FBs using imaging. However, ADCH has no radiologist to report on radiographic images and perform other radiology duties.
Currently, radiographic images are interpreted by referring clinicians. A lack of radiologists affects most of the hospitals in Zambia, with only nine (9) employed in the public health sector.15 The establishment of reporting radiographers to report on general (plain films) radiographic images can help to overcome this challenge. This initiative of having reporting radiographers has worked well in countries, such as the United Kingdom (UK), Denmark, the United States of America (USA), and Uganda.16-19. The few radiologists available in the country can concentrate on reporting on specialised imaging examinations, such as CT, MRI, radionuclide imaging (RNI), mammography, and performing interventional radiology (IR).
CONCLUSION
Aspirated FB is a relatively common paediatric event that presents in children and can have serious or sometimes fatal consequences. In our setting, access to medical imaging is limited due to a lack of different imaging modalities, and radiologists. This significantlyhindersthe delivery of quality imaging services. Yes, it is possible to miss an airway FB on a plain radiograph. However,the presence of radiologists and other imaging optionssuch as fluoroscopy, CT and MRI canincreasethe chance of yielding the right diagnosis and avoiding delayed complications. In the absence of these medical imaging modalities, clinicians and radiographers must have a high index of suspicion to avert deaths.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the children's parents for publication of this case report and accompanying radiographic images. Permission was also obtained from the Senior Medical Superintendent of our hospital to use radiographic images.
ACKNOWLEDEMENTS
Dr. Chizoma Greiner, Paediatric Surgeon of the University Teaching Hospitals - D Block, and all radiographers who imaged this patient.
REFERENCES
- Srivastava G. Airway Foreign Bodies in Children. Clin PediatrEmerg Me d. 2010;11(02):67-72.
- Whitley AS, Jefferson G, Sloane KHC, Anderson G, Hoadley G. Clark's positioning in radiography. 13th ed. London: CRC Press Ltd; 2015.
- Al Maary J, Alahmari AS. Distal airway aspirated metallic foreign body, a case report of spontaneous expectoration. Am J Case Rep. 2020;21 :e917608. Published 2020 Jan 7. doi: 10.12659/AJCR.917608
- Pugmire BS, Lim R, Avery LL. Review of ingested and aspirated foreign bodies in children and their clinical significance for radiologists. Radiographies. 2015; 35(5): 1528-38.
- Patel MS. Airway foreign bodies in children; 2021. From (Accessed 07 October 2021 ).
- Dimond DJ, Palarm T. Paediatric imaging in general radiography. In: Clarver E, Carver B, (Ed). Medical imaging techniques, reflection and evaluation. 2nd Ed. London: Churchill Livingstone Elsevier; 2012: Pp 303-322.
- Aslan N, Y1ld1zda D, 6zden 6, Yontem A, Horoz 66, Klliy S. Evaluation of foreign body aspiration cases in our pediatric intensive care unit: Single-center experience. Turk Pediatri Ars. 2019;54(1):44-48. doi: 10.14744
- Niknejad MT. Foreign body; 2021. From https ://radiopaedia.org/articles/foreign-body-1 (Accessed 07 October 2021).
- Tseng HJ, Hanna TN, Shuaib W, Aized M, Khosa F, Linnau KF. Imaging foreign bodies: ingested, aspirated and inserted. Ann Emerg Med. 2015;66(6):570-582.
- Eren S, Balci AE, Dikici B, Doblan M, Eren MN. Foreign body aspiration in children: experience of 1160 cases. Ann Trap Paediatr. 2003;23(1 ):31-37.
- Saitabau Z, Mrisho BE, Swai H, Ntunaguzi D, Massa we ER. An unusual long standing tracheal foreign body in a paediatric patient removed via tracheostome: A case report. Indian Journal of Case Reports. 2019:268-70.
- Clarke C, Dux A. Chest x-rays for medical students. Oxford: Blackwell Publishing Ltd. 2011. 13. Johnston JN, and Fauber TL. Essentials of radiographic physics and imaging.3rdEd. St Louis Missouri: Elsevier; 2020.
- Chanda E, Bwanga 0, Mutambo S, ChishaM, MulengaM, MusukuJ. Diagnostic imaging of non-accidental injury and percutaneous foreign bodies: a case report from Zambia. Medical JournalofZambia. 2021; 48(2):141 -147.
- Bwanga 0, Chanda E, Kafwimbi S, Sichone J. Opinions of Zambian radiographers on extending their role in the interpretation and reporting on general radiographic images: a cross-sectional survey. Medical Journal of Zambia. 2021; 48(3): 212 -220.
- College of Radiographers. The role of the radiography workforce in image interpretation, film reading and clinical image reporting. London: The College ofRadiographers; 2018.
- Bwanga 0, Mulenga J, Chanda E. Need for image reporting by radiographers in Zambia. Medical Journal of Zambia. 2019; 46(3): 215-220.
- Mubuuke AG, Businge F, Kiguli-Malwadde E. Diagnostic accuracy of chest radiograph interpretation by graduate radiographers in Uganda. African Journal of Health Professions Education. 2019; 11(4):129-132.
- Bwanga 0, Sichone J, Sichone P, Kazuma Y. Image interpretation and reporting by radiographers in Africa: Findings from the literature review and their application to Zambia. Medical Journal of Zambia. 2021;48(2):125 -135.
Medical Journal of Zambia, 49, 1