An Appraisal of Anaesthesia for Abdominal Myomectomy in a Tertiary Institution in North-Central Nigeria
Majeed Babajide Adegboye
Department of Anaesthesia, Faculty of Clinical Sciences, University of Ilorin &University of Ilorin Teaching Hospital.
Ebubechi Okuro Ibegbula
Department of Anaesthesia, University of Ilorin Teaching Hospital, Kwara State.
Osasumwen I. Uwadiae
Department of Anaesthesia, University of Ilorin Teaching Hospital, Kwara State.
DOI: https://doi.org/10.55320/mjz.51.2.529
Keywords:Fibroids, Abdominal myomectomy, Anaesthesia techniques, Perioperative outcomes, Postoperative complications.
ABSTRACT
Background: Abdominal myomectomy is a common gynaecological surgical procedure in our institution to remove uterine fibroids. This study examined the anaesthetic technique and the determinants of immediate postoperative complications and outcomes.
Objective: A retrospective study of the various types of anaesthetic techniques used and the immediate post-operative/anaesthetic complications following an open abdominal myomectomy.
Methods: This was a cross-sectional study of all open abdominal myomectomies performed from 1 st January 2016 to 31 st December 2019 at the University of Ilorin Teaching Hospital. Data collected included demographic data, anaesthetic technique, uterine size, estimated blood loss and postoperative outcomes and complications. Data were analysed using Chi-square and Fisher's exact test as appropriate using SPSS (IBM SPSS Statistics version 22.0 Armonk, NYIBM Corp). Ap-value of <0.05 was taken to be significant.
Results: Two hundred open myomectomies were suitable for analysis. The mean age was 36.4±6.0 years and most patients were ASA I 102(51.0%). Most of the surgeries were performed under regional anaesthesia (RA) 130(65.0%) and 56(28.0%) under general anaesthesia (GA) with 14(7.0%) converted from RA to GA. The predominant RA used was epidural anaesthesia 56(28.0%). Most of the patients who had an estimated blood loss of greater than 2000mls 15(71.4) had GAp=0.000. Only one patient 1(0.5%) had an intraoperative cardiac arrest and was resuscitated.
Conclusion: Regional anaesthesia for open myomectomy is high in our institution with a very good outcome, because of the availability of well-trained personnel.
INTRODUCTION
The commonest benign tumour of the uterus in women of childbearing age is uterine fibroid[1] . Fibroidsoccur in 20% to 30% of women over the age of 30 years, it is more common among Black women than in Caucasians. [2,3] The incidence in Nigeria ranges from 17.9-26% as against 5-11% reported in Europe and the United States of America.[4,5] Abdominal myomectomy is the most common method of treating uterine fibroids in our environment and it accounts for 60.4% of gynaecological cases in Ilorin Nigeria.[6,7]
Ndububa[8] in Southeast, Nigeria found out that the sizes of uterine fibroids at presentation ranged from being bulky to 36 weeks gestation with a median of 20 weeks gestation. Most often patients present very late with huge uterine fibroid for surgical management because of poor socioeconomic status and fear about the possible reproductive outcome if the tumour is to be surgically removed. Also, some patients initially choose alternative care which accounts for the possible reason for their late presentation.[7,9] Patients usually present with huge uterine fibroids in Africa which are beyond the scope of laparoscopic myomectomy and will usually require open abdominal myomectomy. [8,10,11]
In patients who present with huge fibroids, the prevalence of increased pre-operative anaemia from menorrhagia remains a risk factor when considering perioperative blood loss.[12,13,14] Various anaesthetic techniques have been described for the surgical removal of uterine fibroids and the size of the fibroid could influence the choice of anaesthesia.[8] Therefore, the choice of anaesthesia that can reduce perioperative blood loss should be considered because of the association between the anaesthetictechnique used and the risk of perioperative blood loss.[15]
Therefore, the study was a retrospective review of anaesthesia foropenabdominal myomectomy.It was designed to analyse the various anaesthetic techniques used and to determine the effects of the various techniques on intraoperative blood loss, the immediate postoperative complications and outcomes in our institution.
MATERIALS AND METHODS
This was a retrospective cross-sectional study of anaesthesia for abdominal myomectomy at the University of Ilorin Teaching Hospital from 1st January 2016 to 31st December 2019.The University of Ilorin Teaching Hospital (UITH) is located in Ilorin in Oke-Ose; Ilorin -East Local government area, which is the capital of Kwara State in the north-central region of Nigeria. The hospital provides primary, secondary, and tertiary health services to the population. It also serves as a major referral centre for all areas in Kwara State and parts of the neighbouring States of Kogi, Ekiti, Osun, Oyo, and Niger. The hospital has an 8-bed ICU.
Operating theatre records and anaesthetic records were reviewed to know the patients who presented with uterine fibroids and were operated on during the study period.Ethical approval was obtained from theinstitution Ethical Review Committee of theUniversity of Ilorin Teaching Hospital with approval number (ERC PAN/2020/08/0043).The study was performed under the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Patient's demographic data, ASA physical status, previous history of myomectomy, indication for myomectomy, uterine size, the anaesthetic technique used, estimated blood loss, the number of units of blood transfused, the cadre of the anaesthetist, conversion of regional technique to general anaesthesia, presence of intraoperative critical incidence and complications were recorded in the proforma.
Inclusion criteria: All patients who underwent abdominal myomectomy during the study period.
Exclusion criteria: Patients with incomplete information in the anaesthetic and operating theatre records.
The sample size was calculated using the formula for post hoc analysis of a retrospective study.[16]
The minimum number of subjects that needed to be enrolled in the study to have a statistical power of 80% was 128. This study used 200 patient records, exceeding the minimum power of 80%.
This was a cross-sectional retrospective study and numerical data were analysed and presented as frequencies, and percentages, while categorical data were analysed using Chi-square and Fisher's exact test as appropriate using the statistical package for social sciences (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY. IBM Corp). A p-value of <0.05 was considered statistically significant.
RESULTS
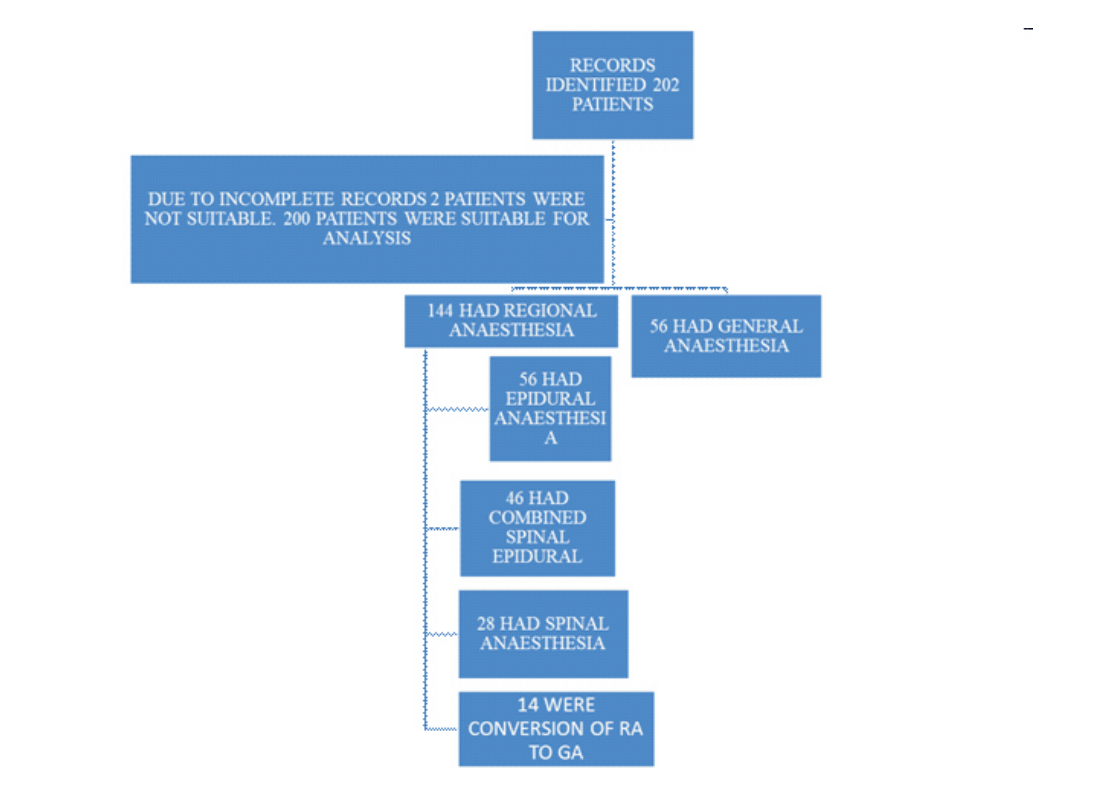
From the retrieved anaesthetic records of 202 patients who had abdominal myomectomy only 200 patients were suitable for analysis for the study, two were not eligible for analysis due to incomplete records. Table 1 shows that most of the patients that had abdominal myomectomy were between the ages of 36 and 40 years (33.0%). The mean age was 36.4±6.0 years, the minimum age was 21 years and the maximum age was 63 years. The majority of the patients were ASA I 102(51.0%). Only 7 (3.5%) had a previous myomectomy Most patients had a uterine size of ≤ 20 weeks 138(69.0%) while 62(31.0%) had a uterine size of ?20 weeks. In this study, the indication for myomectomy for the majority of the patients was menorrhagia 155(77.5%). The mean duration of surgery was 3 hours 38 minutes ±1-hour 35 minutes with a minimum duration of 1 hour and a maximum duration of 7 hours. Most of the abdominal myomectomies were performed under regional anaesthesia 130(65.0%) and only 56 (28.0%) were performed under general anaesthesia. Table 2 shows that the most frequently used regional anaesthetic technique was epidural anaesthesia 56(28.0%) and spinal anaesthesia 28(14.0%) was the least technique used.
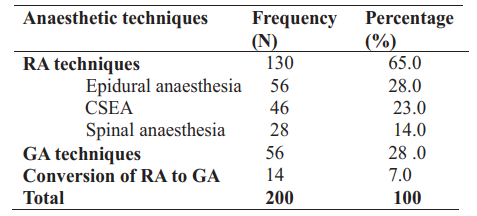
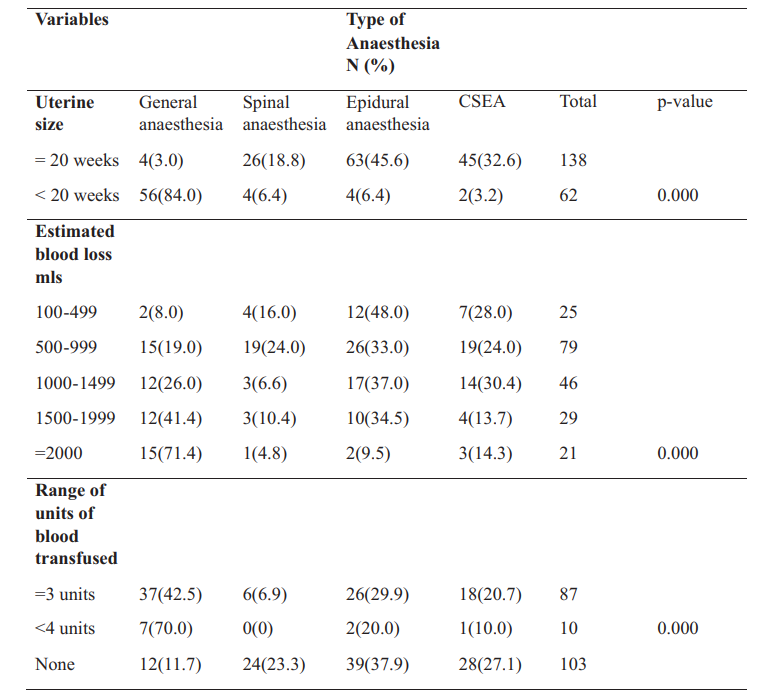
Table 3 shows that most of the patients that had uterine size above 20 weeks had general anaesthesia 56(84%) which was statistically significant p < 0.0001. Also, most of the patients that had estimated blood loss of greater than 2000mls 15(71.4%) had general anaesthesia which was statically significant p < 0.0001. Furthermore, most of the patients that had more than 4 units of blood transfused 7(70.0%) had general anaesthesia and it was also statistically significant p < 0.0001.
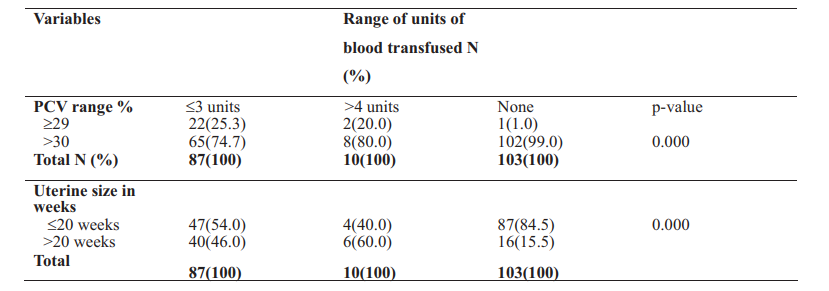
Table 4 shows that out of the 103 patients who were not transfused with blood, 102 (99.0%) of them had a pre-operative packed cell volume (PCV) of greater than 30% and this was statistically significant p< 0.0001. Patients with a uterine size of less than 20 weeks 87(84.5%) also had no blood transfusion and this was statistically significant p < 0.0001.
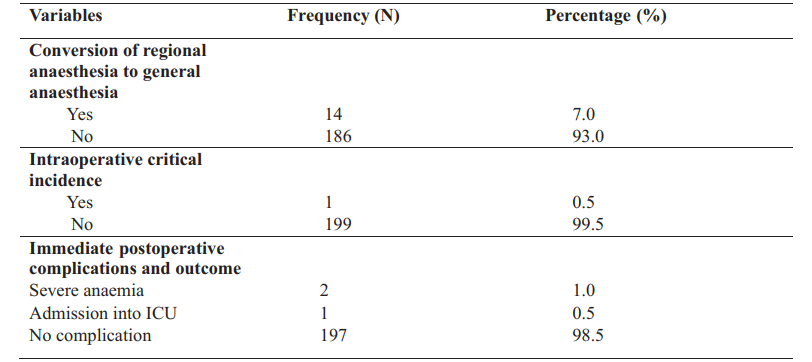
Two patients 2(1.0%) had severe anaemia in the immediate post-operative period and they were transfused with whole blood in the post-anaesthesia care unit and eventually transferred to the ward. Most of the patients 197(98.5%) had no intraoperative or immediate postoperative complications and were transferred to the ward.
The cadre of anaesthetists that conducted the anaesthesia were mostly consultants and senior registrars 167(83.5%), Others were consultants and registrars 31(15.5%), consultant alone 1(0.5%), senior registrar and registrar 1(0.5%).
DISCUSSION
This study showed that General anaesthesia for open-abdominal myomectomy was associated with more estimated blood loss of ≥2000 mls. However, because of the high rate of use of regional anaesthetic techniques, we had very few postoperative complications and good outcomes. The mean age of surgery for open abdominal myomectomy in this study was 36.4± 6.0 years which is comparable with that of the study of Asudo and Abdullahi.[17] who reported 36.5±6.3 yearsin Abuja, Nigeria. The percentage of patients documented with this mean age in this study was also comparable to that in an American study where the incidence of uterine fibroids was 60% at 35 years among African–American women.[18]
In this study, 65% of the abdominal myomectomies were performed under regional anaesthesia. This was higher than that reported by Asudo and Abdullahi.[17] who reported that 54.6% of abdominal myomectomies in their institution were performed using regional anaesthesia. The use of regional anaesthesia was higher in our institution because we predominantly use epidural anaesthesia or CSEA as our technique of choice because it can be used in prolonged surgeries which is a major problem when a single shot spinal anaesthesia is used, it also provides good intraoperative and postoperative analgesia and also for the avoidance of airway related complications associated with general anaesthesia. Nnaji and Chikwe.[19] in Owerri Nigeria reported that the technique of anaesthesia for open abdominal myomectomy was predominantly general anaesthesia (79.0%) because general anaesthesia was their technique of choice in abdominal myomectomies. Globally there is an increasing trend towards regional anaesthetic techniques for procedures amenable to regional anaesthesia including surgeries for fibroid.[19] General anaesthesia has several shortcomings which include the likelihood of high morbidity and mortality during endotracheal intubation, increased prevalence of postoperative nausea and vomiting(PONV), deep venous thrombosis (DVT) and pulmonary embolism.[20,21] Furthermore, evidence has shown that the regional anaesthetic technique has better perioperative outcomes when compared with general anaesthesia in terms of DVT, myocardial events and pulmonary embolism.[22,23] The most frequently used regional anaesthetic in this study was epidural anaesthesia 56(28%) and CSEA 46(23%), which is in line with the best global practices.[19] Most of the anaesthetists in this study preferred to use epidural anaesthesia and CSEA compared to the use of single-shot spinal anaesthesia 30(15%) probably because of the huge size of fibroids and the estimated duration of surgery, as these techniques would enhance the extension of anaesthesia (if required) through the epidural catheter. In this study, the average duration of surgery was about 3 hours therefore, if single-shot spinal were used the surgery would have outlasted the duration of the spinal block. The use of epidural anaesthesia and CSEA also has the advantage that they can be used for postoperative analgesia. The rate of conversion from regional anaesthesia to general anaesthesia in the present study was 7% which is higher than that reported by Asudo and Abduallahi.[17] who reported a conversion rate of 5%. The reason for our higher rate of conversion was that in our study we used more epidural anaesthesia alone, whereas epidural anaesthesia alone was not used in their study, rather they used more CSEA. Epidural anaesthesia alone does provide good and continuous analgesia during surgery; however, the onset of the sensory block may be delayed and sometimes patchy. This negative effect is usually overcome by the use of CSEA and therefore, a lower conversion rate to general anaesthesia.
This study shows that most of the patients with a uterine size of less than 20 weeks had no blood transfusion and this result was statistically significant. It is in agreement with findings by Pundir et al. [24] in an analysis of 200 abdominal myomectomies, who reported that uterine size of 20 weeks or more was a major predictor of perioperative bleeding requiring blood transfusion. West et al.[25] also reported that 77 out of 91 cases of abdominal myomectomy of a uterine size of 20 weeks or more required blood transfusion for perioperative blood loss. Our study also revealed that most of the patients with perioperative PCV of greater than 30% had less blood transfusion which was statistically significant. Kike et al. [26] also reported similar findings that in patients that lost less than 500mls of blood, 80.4% of them had a preoperative PCV of at least 30% (p=0.013). Therefore, adequate PCV may suggest better oxygenation of the myometrial cells and therefore appropriate circulatory and metabolic responses to surgical trauma.
Most patients that had uterine sizes above 20 weeks also had an estimated blood loss of greater than 2000mls in the index study had general anaesthesia. Therefore, when the size of the fibroid is huge the duration of surgery may be prolonged, resulting in the choice of general anaesthetic technique, and there is usually the tendency for increased blood loss when general anaesthesia is used.[11,15] However, a regional anaesthetic technique such as CSEA is a wise choice to be considered as it is associated with hypotensive effects that can significantly help in reducing blood loss at surgery. Haemodynamic differences, with lower arterial blood pressure, lower central venous blood pressure, and most importantly lower peripheral venous blood pressure in the surgical wound seem to explain the lower blood loss intra- and post-operatively in patients given regional anaesthesia. These differences in haemodynamics give rise to less arterial pressure and notably less venous oozing of blood from the surgical area.[27] The study by Otokwala and Ebirim[28] concluded that CSEA technique is safe, with a relatively low rate of perioperative complications when used during open abdominal myomectomy for huge uterine fibroids. The use of RA in this study was high, especially Epidural and CSEA anaesthetic techniques which offered the benefits of good analgesia even in prolonged surgeries and in the postoperative period and the avoidance of airwayrelated complications usually associated with general anaesthesia. General anaesthesia is sometimes associated with morbidities like Difficult airway, awareness under anaesthesia, pain and cardiorespiratory depression.[19]
We recorded only one intraoperative critical incidence which was a case of intraoperative cardiac arrest in a 29-year-old with a uterine size of 20 weeks who had open abdominal myomectomy with epidural anaesthesia. The incident occurred about 90 minutes into the surgery and about 5 minutes after the release of the elastic tourniquet used on the uterus for haemostasis; the patient was noticed to be progressively desaturating, hypotensive and subsequently became unresponsive and then a cardiac arrest which was promptly detected. Cardiopulmonary resuscitation (CPR) was immediately commenced and the patient had return of spontaneous circulation (ROSC) after about 15 minutes. The patient was intubated and surgery was completed with general anaesthesia. The likely cause of cardiac arrest in this patient was reperfusion syndrome caused by prolonged use of the uterine tourniquet leading to sudden hypotension, metabolic acidosis and hyperkalaemia after a few minutes of tourniquet release; the use of the tourniquet caused ischemia to muscle tissues resulting in tissue hypoxia, acidosis, accumulation of lactate, toxic metabolites and oxygen-free radicals.[29] The estimated blood loss was 300mls.The patient was subsequently admitted into the intensive care unit after the procedure for post-resuscitation care and cardiopulmonary monitoring.She regained full consciousness after 48 hours in the ICU and was discharged to the ward. No mortality was recorded throughout the study period.
Limitations
Due to the retrospective nature of the study, we had some incomplete data in the anaesthesia/ theatre records and these incomplete data were not analysed.
CONCLUSION
The rate of regional anaesthesia for open myomectomy is high in our institution with a very good outcome, with epidural anaesthesia and CSEA being the predominant types of anaesthetic techniques used. Our institution operates a consultant lead team which has contributed to improved training of manpower and skill acquisition. Therefore, because of the availability of equipment and skills, we have increased the utilization of regional anaesthesia for open myomectomies in our institution in line with global best practices. This has resulted in reduced postoperative complications and good outcomes. Lastly, a prospective study to assess patient satisfaction with the various anaesthetic techniques for open abdominal myomectomy should be considered.
DECLARATIONS
Acknowledgements
The authors thank all the anaesthetist technicians and records staff at the Institution for helping in the retrieving of patient's folders.
Competing of interest:
The authors declare that they have no competing interest
Funding: Not applicable
Authors` contributions:
·Study design and recruitment of patients: MBA, EOI, OIU ·Statistical analysis, results and draft of the manuscript. MBA, OIU
REFERENCES
- Omole-Ohonsi A, Belga F. Surgical management of uterine fibroids at Aminu Kano Teaching Hospital. Obstet Gynecol Int.2012; 2012:702325. doi:10.1155/2012/702325
- Okogbo FO, Ezechi OC, Loto OM, Ezeobi PM. Uterine leiomyomata in South Western Nigeria: A clinical study of presentations and management outcome. Afr Health Sci. 2011;11(2):271-278.
- Ogunniyi SO, Fasubaa O. Uterine fibromata in Ilesha, Nigeria. Niger Med Pract.1990; 19:9395.
- Ogedengbe OK. Uterine fibroids. In: Okonofua F, Odunsi K, editors. Contemporary obstetrics and gynaecology for developing countries. 1st ed. Ibadan: Women's Health and Action Research Centre; 2003. p. 202-213.
- Laughlin SK, Baird DD, Savitz DA, Herring AH, Hartmann KE. Prevalence of uterine leiomyomas in the first trimester of pregnancy: an ultrasound-screening study. Obstet Gynecol. 2 0 0 9 ; 1 1 3 ( 3 ) : 6 3 0 - 6 3 5 . d o i : 10.1097/AOG.0b013e318197bbaf
- Omokanye LO, Salaudeen GA, Saidu R, Jimoh AAG, Balogun OR. Surgical management of uterine fibroids at the University of Ilorin Teaching Hospital: A 5-year review. Glob Res J Med Sci. 2012;2(2):018-022.
- Uba FA. Uterine fibroids: Which treatment? Niger Med J.2011; 52:149.
- Ndububa VI. Uterine fibroids: Experience with 100 myomectomies in Orlu, South East Nigeria. Port Harcourt Med J. 2016; 10:124-129.
- Adegbesan-Omilabu MA, Okunade KS, Gbadegesin A. Knowledge of, perception of, and attitude towards uterine fibroids among women with fibroids in Lagos, Nigeria. Scientifica (Cairo). 2014; 2014:1-5. doi:10.1155/2014/809536
- Atombosoba AE, Lucky OL, Chukwuemeka AI, Israel J, Isa AI, Ibrahim. Review of the clinical presentation of uterine fibroid and the effect of therapeutic intervention on fertility. Am J Clin Med Res. 2015;3(1):9-13.
- Ezeama CO, Ikechebelu JI, Obiechina NJ, Ezeama NN. Clinical presentation of uterine fibroids in Nnewi, Nigeria: A 5-year review. Ann Med Health Sci Res. 2012; 2:114-118.
- Obuna JA, Umeora OUJ, Ejikeme BN, Egwuatu VE. Uterine fibroids in the tertiary health centre in South-East Nigeria. Niger J Med.2008; 17:447-451.
- Tokarev AA, Butylin AA, Ataullakhanov FI. Platelet adhesion from shear blood flow is controlled by near-wall rebounding collisions with erythrocytes. Biophys J. 2011;100(4):799-808. doi: 10.1016/j.bpj.2010.12.3730
- Tettey M, Aniteye E, Sereboe L, Edwin F, Kotei D, Tamatey M, et al. Predictors of postoperative bleeding and transfusion in cardiac surgery. Ghana Med J. 2009;43(2):71-76.
- Aggo AT, Fyneface-Ogan S, Mato CN. The differential impact of two anaesthetic techniques on cortisol levels in Nigerian surgical patients. Niger J Clin Pract.2012; 15:68-74
- Bolarinwa OA. Sample size estimation for health and social science researchers: The principles and considerations for different study designs. Niger Postgrad Med J. 2020; 27:67-75.
- 1Asudo FD, Abdullahi HI. Anaesthesia for fibroid surgeries: experience from a Nigerian tertiary institution. Int J Contemp Med Res. 2020;7(1)
- Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2 0 0 3 ; 1 8 8 ( 1 ) : 1 0 0 - 1 0 7 .doi:10.1067/mob.2003.99
- Nnaji CT, Chikwe K. Anesthesia for abdominal myomectomy: A five years audit of a Federal Medical Centre in Owerri, Nigeria. J Anest Anesthesiol. 2017;1(1):16-19.
- Ugochukwu O, Adaobi A, Ewah R, Obioma O. Postoperative nausea and vomiting in a gynaecological and obstetrical population in South-Eastern Nigeria. Pan Afr Med J.2010; 7:6. doi:10.4314/pamj. v7i1.69043
- Bon S, Anand TT, Dinesh K. Attenuation of haemodynamic responses to laryngoscopy and endotracheal intubation with intravenous dexmedetomidine: A comparison between two doses. Indian J Anaesth. 2017; 61:48-54. doi: 10.4103/ija.IJA_256_16
- Gupta PK, Hopkins PM. Regional anaesthesia for all? Br J Anaesth. 2012; 109:7-9. doi:10.1093/bja/aes198
- Adegboye MB, Kadir DM, Chikamnario J. Anaesthesia for orthopaedic surgeries in two tertiary institutions in north central Nigeria. J Orthop Trauma Surg Rel Res.2018; 13:13-16.
- Pundir J, Krishnan N, Siozos A, Uwins C, Kopeika J, Khalaf Y, et al. Perioperative morbidity associated with abdominal myomectomy for very large uterine fibroids. Eur J Obstet Gynecol Reprod Biol. 2 0 1 3 ; 1 6 7 ( 2 ) : 2 1 9 - 2 2 4 . d o i : 10.1016/j.ejogrb.2012.12.012
- West S, Ruiz R, Parker WH. Abdominal myomectomy in women with very large uterine size. Fertil Steril. 2006; 85:36-39. doi: 10.1016/j.fertnstert.2005.06.030
- Adesina KT, Owolabi BO, Raji HO, Olarinoye AO. Abdominal myomectomy: A retrospective review of determinants and outcomes of complications at the University of Ilorin Teaching Hospital, Ilorin, Nigeria. Malawi Med J. 2017; 29:37-42. doi:10.4314/mmj. v29i1.8
- Modig J. Regional anaesthesia and blood loss. Acta Anaesthesiol Scand Suppl. 1988; 89:44-48. doi:10.1111/j.1399-6576. 1988.tb02842.x
- Otokwala JG, Ebirim LN. Necessity of Combined Spinal Epidural Technique During Open Abdominal Myomectomy for Huge Uterine Fibroids. Medical Journal of Zambia. 2018; 45: 106 – 111.
- Nnang EJ, Ovono AF, Tsagoulela A, Edjo NG, Assoumou P, Bang NJ, et al. Uterine reperfusion ischemia and use of elastic tourniquet. J Biosci M e d . 2 0 1 9 ; 7 : 9 8 - 1 1 9 .doi:10.4236/jbm.2019.72009
Medical Journal of Zambia, Vol 51, 2
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.