Oral Health Status and Treatment Needs of Patients on ART at Levy Mwanawasa University Teaching Hospital in Lusaka, Zambia: A Cross Sectional Study
Gabriel Mpundu
Levy Mwanawasa Medical University
Dr. Given Moonga
University of Zambia
John Soko
University of Zambia
Crecious Phiri
Levy Mwanawasa Medical University
DOI: https://doi.org/10.55320/mjz.52.2.511
Keywords:Periodontitis, Antiretroviral treatment, mucosa, ulceration, necrotizing gingivitis
ABSTRACT
Background: HIV/AIDS remains a global public health challenge, with 39.1 million people living with HIV worldwide and 1.4 million in Zambia. Oral health is a critical but often overlooked aspect of care in people living with HIV/AIDS (PLWH).
Aim: This study assessed the oral mucosal, periodontal, and dentition status of HIV/AIDS patients attending the ART center at Levy Mwanawasa University Teaching Hospital, Lusaka, Zambia.Methods: A cross-sectional study of 361 HIV/AIDS patients was conducted. Oral health status was recorded using a modified WHO Oral Health Assessment form (1997), and data were analyzed using STATA version 16.0. Chi-square, Fisher’s exact test, and ANOVA were applied to identify significant associations.
Results: Among the participants, 52% were women, and 68% were aged 26–55 years. Periodontitis was the most prevalent oral lesion (48.5%), followed by ulcerations (40.99%), acute necrotizing gingivitis (26%), and hypermelanotic pigmentation (15.8%). Nearly all participants required dental treatment, but only 12% had healthy periodontal status. Significant findings included lower odds of treatment needs in urban residents (OR=0.75, 95% CI: 0.44–0.99, p<0.001) and higher odds among older adults aged 66–75 years (OR=5.38, 95% CI: 1.62–17.80, p=0.006). Excellent self-reported oral health reduced treatment needs (OR=0.07, 95% CI: 0.02–0.21, p<0.001), while poor oral health increased them (OR=2.74, 95% CI: 1.94–8.00, p=0.045). Cleaning teeth twice daily reduced treatment needs (OR=0.16, 95% CI: 0.04–0.62, p=0.008), while patients with over four years of HIV illness had elevated treatment needs (OR=3.30, 95% CI: 1.42–7.67, p=0.006).
Conclusion: The high prevalence of periodontitis and substantial treatment needs highlight the need to integrate oral health into HIV care. Urban-rural disparities, age, duration of HIV illness, and oral hygiene practices were significant determinants of dental treatment needs, underscoring the importance of accessible and preventive oral healthcare services for PLWH.
INTRODUCTION
Acquired Immunodeficiency Syndrome (AIDS) is a life-threatening condition caused by the Human Immunodeficiency Virus (HIV), which progressively weakens the immune system, making the body vulnerable to opportunistic infections, neurological disorders, and unusual malignancies.[1][2] The first recognized case of AIDS was reported by the Centers for Disease Control and Prevention (CDC) in 1981 among homosexual men in the United States.[3]
Globally, the predominant mode of HIV transmission is through unprotected heterosexual intercourse, though other significant routes include unprotected sex between men, injecting drug use, and unsafe blood transfusions or injections.[4] As of 2022, approximately 38.4 million people were living with HIV worldwide, and 1.5 million individuals were newly infected with the virus in 2021.[5] Notably, there has been a global decline in the number of new HIV infections and AIDS-related deaths due to the widespread availability and uptake of antiretroviral therapy (ART). By 2021, nearly 28.7 million people were receiving ART, up from 15.0 million in March 2015.[6]
In Zambia, the first HIV case was detected in 1984. As of 2020, an estimated 1.5 million people were living with HIV in Zambia, with an adult prevalence rate of approximately 11.1% among those aged 15-49.[7] The country has made significant progress in reducing AIDS-related mortality, with 19,000 deaths reported in 2019, down from 24,000 in 2010.[4] Zambia ranks as the seventh country in Africa with the highest HIV prevalence.[4]
Under Zambia's National AIDS Control Programme, the provision of free ART for people living with HIV/AIDS began on April 1, 2004, in selected government hospitals. By October 2016, there were eight ART centers operating across the country.[7] Public health access to ART emphasizes the need for standardized, user-friendly, and minimally toxic treatment regimens.
Oral manifestations are key diagnostic and prognostic indicators in individuals infected with HIV.[8][21] While numerous studies have examined the oral manifestations of HIV infection, there is limited data specific to the Zambian population. The oral presentation of HIV may vary across different populations, underscoring the importance of region-specific research. Therefore, this study aims to investigate the prevalence of oral conditions among HIV/AIDS patients attending the ART centre at Levy Mwanawasa University Teaching Hospital in Lusaka, Zambia.
MATERIALS AND METHODS
This study was a cross-sectional design aimed at assessing the oral health status and treatment needs of 361 HIV/AIDS patients attending the Antiretroviral Therapy (ART) centre at Levy Mwanawasa University Teaching Hospital (LMUTH). A pilot study was conducted with 50 patients, and based on the findings, the study instruments were refined. The final study used a modified version of the World Health Organization (WHO) Oral Health Assessment form from 1997 to record oral mucosal lesions/conditions, periodontal status, and dentition status among participants.
Study Design
This cross-sectional study involved a single observation of each participant to assess their oral health status. The data collection was performed over a defined period, ensuring that each participant was only assessed once.
Sampling Technique
A systematic random sampling method was employed to select participants from the patient population attending the ART centre. All eligible participants who met the inclusion criteria during the study period were approached, and those who provided informed consent were included in the study.
Ethical Considerations
The study received ethical clearance from the University of Zambia Biomedical Research Ethics Committee (UNZABREC) and the National Health Research Authority (NHRA). The ethical approval reference numbers are UNZABREC/2021/09 and NHRA/2021/04. All participants provided verbal informed consent before inclusion in the study. Confidentiality was maintained by anonymizing participant data.
Calibration of Examiners
To ensure reliability and validity of the oral health assessments, all examiners underwent a rigorous standardization and calibration process before data collection commenced. This process included training sessions and inter-examiner reliability testing to minimize variability in the assessment of oral health conditions. Calibration was conducted with a subset of patients, and examiners were required to achieve a kappa statistic of at least 0.80 for inter-examiner agreement before the study began.
Data Collection
Oral examinations were conducted using disposable tweezers, disposable mouth mirrors, Community Periodontal Index (CPI) probes, and straight probes to assess the presence of dental caries and oral lesions. The data collected were systematically recorded and later entered into a spreadsheet program (Microsoft Excel 2007).
Data Analysis
The data were analysed using STATA version 16.0. Descriptive statistics were used to summarize the oral health status of the participants. Inferential statistics, including the Chi-square test, Fisher's exact test, and one-way analysis of variance (ANOVA), were employed to identify associations between variables. The level of statistical significance was set at p < 0.05.
Inclusion Criteria
- All HIV/AIDS patients present at the ART centre during the study period.
- Patients who provided verbal informed consent to participate.
Exclusion Criteria
- Patients who declined to participate in the study.
RESULTS
This study was conducted to assess the prevalence of oral mucosal lesion/conditions, periodontal, and dentition status of HIV/AIDS patients attending ART center Levy Mwanawasa University Teaching Hospital. The study population consisted of 361 individuals, of which 175 (48%) were men and 186 (52%) were women.
Table 1. Demographic Distribution of participants
| Demographics (N=361) | Frequency | Percentage |
|---|---|---|
| Gender | ||
| Female | 186 | 52% |
| Male | 175 | 48% |
| Age category (N=361) | ||
| 18-25 Years | 73 | 20.22% |
| 26-35 Years | 77 | 21.3% |
| 36-45 Years | 81 | 22.4% |
| 46-55 Years | 83 | 23.0% |
| 56-65 Years | 24 | 6.7% |
| 66-75 Years | 19 | 5.3% |
| 76-85 Years | 3 | 0.8% |
| 86-100 Years | 1 | 0.3% |
| Residence (N=361) | ||
| Peri-Urban | 60 | 16.6% |
| Rural | 89 | 24.7% |
| Urban | 212 | 58.7% |
| Education Level (N=361) | ||
| No Formal Education | 18 | 5.0% |
| Primary School | 61 | 16.9% |
| Secondary School | 112 | 31.0% |
| Tertiary Education | 145 | 40.2% |
| Post Graduate | 25 | 6.9% |
| Occupation | ||
| Administration and Office work | 26 | 10.28% |
| Education | 43 | 17.00% |
| General Labour | 72 | 28.46% |
| Health care and Medical | 71 | 28.06% |
| Student | 28 | 11.07% |
| Transportation and driving | 5 | 1.98% |
| Other | 8 | 3.16% |
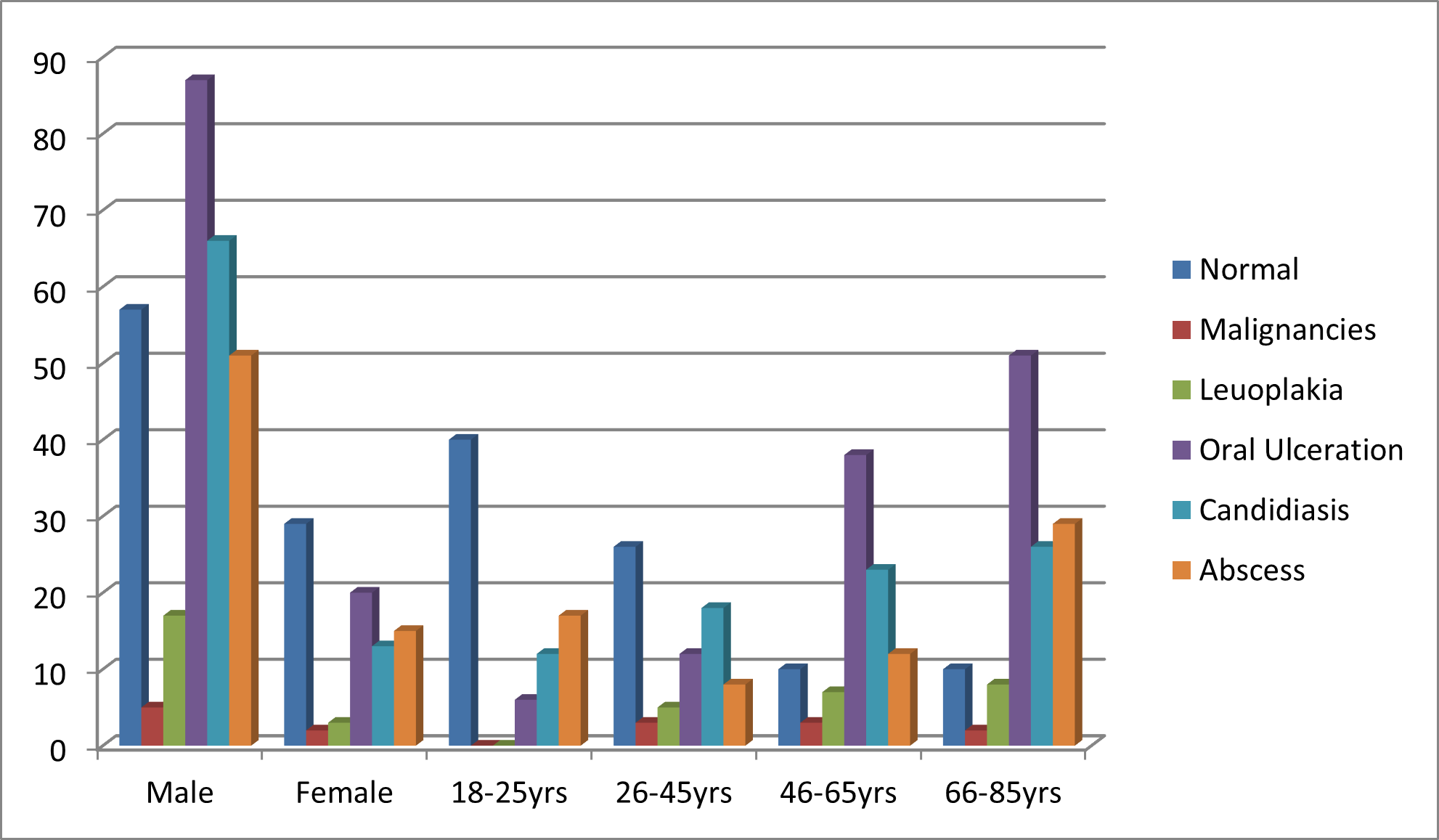
The study subjects were divided into different age groups of 18-25 years (20.2%), 26-35 years (21.3%), 36-45 years (22.4%), 46-55 years (23.0%), and 56-65 years (6.7%), 66-75 years (5.3%), 76-85 years (0.8%) and 86-100 years (0.3%). Table 2 shows the association of extraoral findings with gender. Among the study subjects 43.76% had normal extraoral appearance. Graph 1 shows the association of oral mucosal lesions/conditions with gender. Periodontitis was the most prevalent oral condition found among 32.5% of the study subjects. Buccal mucosa was the most common site of presence of oral mucosal conditions among 39.8% male and 30.6% female study subjects. Approximately 2% of the subjects had a healthy periodontal status.
Table 2: Association of extraoral examination findings with gender
| Lesion | Male (N =175) n (%) | Female (N =186) n (%) | Total (n=361) n (%) |
|---|---|---|---|
| Normal Findings | 96(54.85%) | 62(33.33%) | 158(43.76%) |
| Lip Ulceration | 88(50.28%) | 60(32.25%) | 148(40.99%) |
| Norse/Nasal Ulceration | 15(8.5%) | 11(5.91%) | 26 (7.2%) |
| Head/ Neck Lesions | 29(16.57%) | 14(7.52%) | 43 (11.91%) |
The presence of calculus was the most prevalent finding among 48.9% male and 53.9% female subjects. The loss of attachment of 0-3 mm was seen among 49.1% subjects. The prevalence of loss of attachment of 4-5 mm among the male and female study subjects was 28.2% and 30.6%, respectively. (Graph 1: Oral Lesions by Age Groups)
Graph 2 shows the number of study subjects with different dental treatment needs. One surface filling treatment was required by 86.7% male and 72% female study subjects, which is statistically significant. Prosthetic treatment was required by 69.1% male and 73.2% female subjects.
Graph 2: Treatment Needs
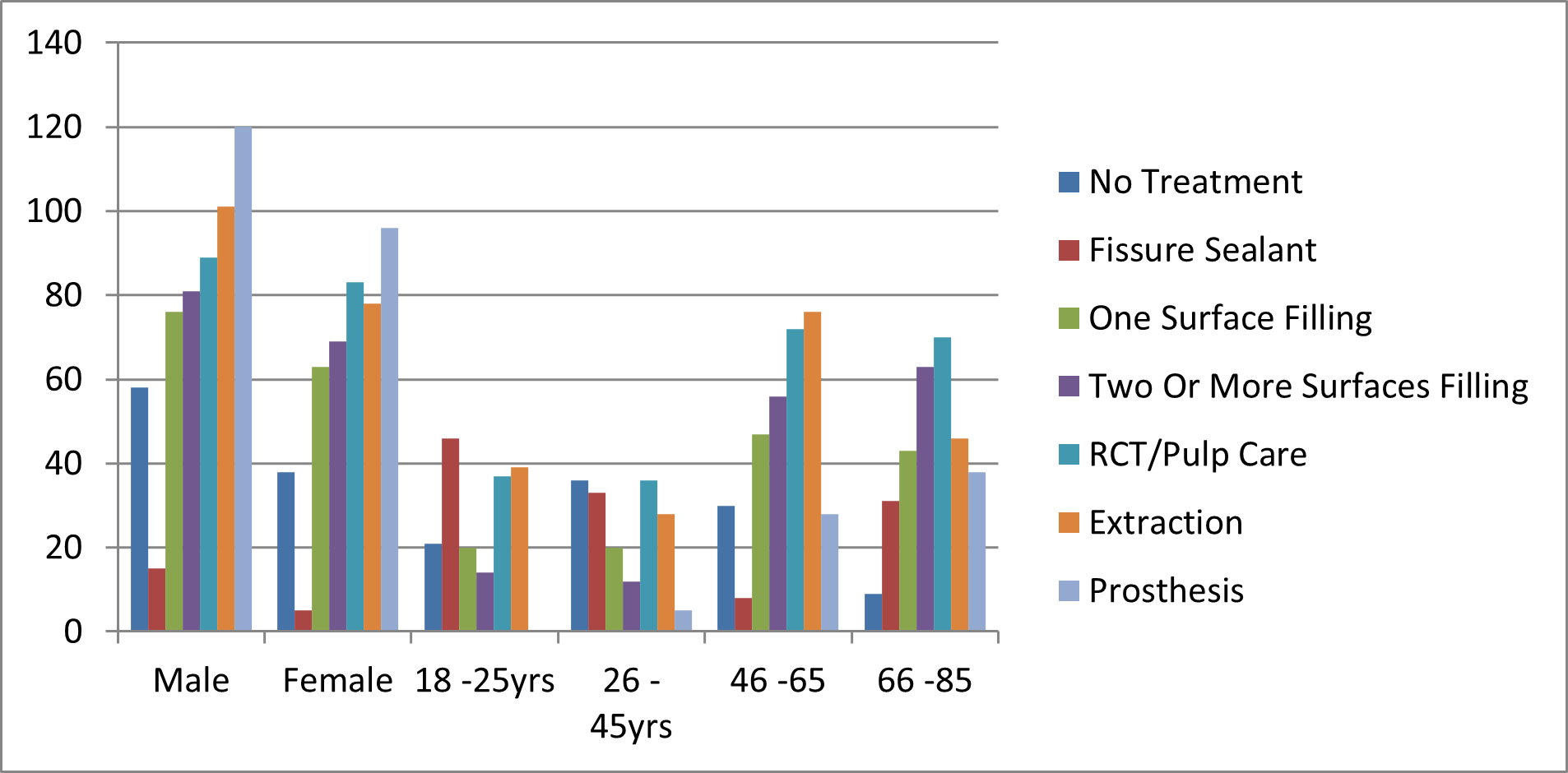
Table 3. Frequency of individuals experiencing symptoms
| Experience | Very Often | Fairly often | Sometimes | No |
|---|---|---|---|---|
| Difficulty Biting | 39 | 56 | 102 | 155 |
| Difficulty chewing | 36 | 23 | 46 | 238 |
| Difficulty in speech | 26 | 27 | 78 | 211 |
| Dry mouth | 36 | 27 | 63 | 219 |
| embarrassment due to appearance of teeth | 27 | 34 | 80 | 207 |
| Tense | 29 | 36 | 71 | 212 |
| Avoid smiling | 21 | 33 | 84 | 204 |
| Interrupted sleep | 17 | 38 | 75 | 215 |
| Days of work | 12 | 29 | 60 | 242 |
| Difficulty usual activities | 15 | 24 | 54 | 238 |
Table shows the frequency of individuals experiencing different levels of difficulty in various aspects related to oral health and well-being.
This data suggests that a significant portion of the sample population experiences some level of difficulty biting, with a higher number reporting it as "sometimes" or "fairly often."
The majority of respondents in this category report no difficulty with chewing. However, a notable number experience some level of difficulty, with "sometimes" being the most common response. Speech difficulties are less prevalent compared to chewing or biting issues, but a significant portion of respondents still report experiencing them, with "sometimes" being the most common response. Dry mouth appears to be a common issue among the sample population, with a substantial number of individuals reporting it as "sometimes."
Many individuals in the sample population report feeling embarrassed due to the appearance of their teeth, with "sometimes" and "fairly often" being the more common responses. A significant portion of respondents reports feeling tense in various situations, with "sometimes" being the most frequent response.
Avoiding smiling due to oral health concerns is relatively common among the sample population, with "sometimes" being the most prevalent response.
Sleep interruptions are reported by a notable number of individuals, with "fairly often" and "sometimes" being the more common responses.
This indicates that a substantial portion of the sample population occasionally misses work due to oral health-related issues.
This suggests that a significant number of individuals experience difficulty in their usual activities, with "sometimes" being the most common response.
Description of Multi-Variant Adjusted Results
Table shows the regression analysis that examines factors influencing the dental treatment needs of people living with HIV (PLWH) based on adjusted odds ratios (OR) and confidence intervals (CI). Key findings are summarized below:
Males showed increased odds of needing dental treatment compared to females (OR=1.5, 95% CI: 0.99-2.27, p=0.047). However, this significance was lost in the adjusted model (OR=1.28, 95% CI: 0.74-2.22, p=0.372).
Urban residents had significantly lower odds of requiring dental treatment compared to rural residents (OR=0.42, 95% CI: 0.23-0.75, p=0.003). After adjustment, urban residents still had reduced odds, maintaining significance (OR=0.75, 95% CI: 0.44-0.99, p<0.001).
Age was a significant determinant, with the 66-75 years age group exhibiting the highest odds of needing dental treatment compared to 18-25 years (OR=5.38, 95% CI: 1.62-17.80, p=0.006). Other age groups did not show significant results.
Patients with removable teeth were more likely to need dental treatment (OR=2.07, 95% CI: 1.29-3.33, p=0.003). However, this association was not significant in the adjusted model (OR=0.83, 95% CI: 0.43-1.58, p=0.567).
Oral health status was a significant factor. Patients reporting "excellent" oral health had reduced odds of needing dental treatment (OR=0.06, 95% CI: 0.02-0.16, p<0.001), a trend that persisted in the adjusted model (OR=0.07, 95% CI: 0.02-0.21, p<0.001). Those with "very good" oral health also showed a significant reduction (OR=0.04, 95% CI: 0.02-0.09, p<0.001).
Cleaning teeth twice or more a day significantly reduced the odds of needing dental treatment compared to cleaning once a month (OR=0.16, 95% CI: 0.04-0.62, p=0.008).
Patients who had not received dental care had lower odds of treatment needs compared to those visiting every six months (OR=0.36, 95% CI: 0.18-0.75, p=0.006). Visiting the dentist more than a year but less than two years ago was associated with higher odds (OR=2.76, 95% CI: 1.13-6.74, p=0.026).
Routine check-ups or treatment were associated with significantly higher odds of needing dental treatment (OR=2.71, 95% CI: 1.19-6.17, p=0.017). This persisted in the adjusted model (OR=2.50, 95% CI: 1.03-6.04, p=0.042).
A duration of 1-3 years significantly reduced the odds of requiring dental treatment compared to a duration of 0-6 months (OR=0.56, 95% CI: 0.39-0.79, p=0.001). Conversely, having HIV for 4 years or more increased treatment needs (OR=3.23, 95% CI: 1.23-8.33, p=0.017), with significance retained in the adjusted model (OR=3.30, 95% CI: 1.42-7.67, p=0.006).
DISCUSSION
This cross-sectional study evaluated the oral health status and treatment needs of 361 patients receiving antiretroviral therapy (ART) at Levy Mwanawasa University Teaching Hospital, Lusaka, Zambia. The oral cavity, often an overlooked diagnostic tool, plays a significant role in identifying early signs of HIV progression.[9]
In the current study, 52% of participants were female, similar to Singh[10], who noted higher female attendance in oral health studies. Women are more likely to seek care due to aesthetic concerns, discomfort, or embarrassment associated with oral health conditions. However, this contrasts with findings from studies conducted in India[11] and Nigeria[12] where males were predominant among HIV-positive patients. Differences in healthcare-seeking behavior and cultural norms may explain this contrast, as women in sub-Saharan Africa often report greater engagement with healthcare services due to maternal health interventions.
The most common age group was 26-55 years, aligning with findings by Mathur[12] and Sandeep[36] who also identified the sexually active population as the most affected age group. However, studies conducted in high-income countries like the United States report older age groups (55+) were being more represented in HIV-positive populations due to better survival rates and aging with ART.[21] This highlights the demographic shift in HIV prevalence based on the healthcare context.
The prevalence of periodontal disease was 48.5%, which aligns with findings by Sandeep[36] and Ranganathan[13], who observed that periodontal issues are among the earliest clinical signs of HIV infection due to immunosuppression. However, studies from high-income settings[40] report lower periodontal disease prevalence due to better oral hygiene practices and access to dental care. These contrasting findings emphasize the impact of socioeconomic factors, ART adherence, and access to healthcare on oral health outcomes.
Oral mucosal lesions were observed in 80.53% of participants, which is consistent with a study in South Africa[14], who reported a 51.1% prevalence. The higher rate in this study could reflect differences in ART coverage and disease stage. In contrast, studies in developed settings[9] report mucosal lesion prevalence below 30%, attributed to early diagnosis and effective ART regimens.
Smokers and alcohol users in this study were more likely to have poor oral health, aligning with Gary et al[15], who highlighted the negative impact of these habits on oral hygiene and periodontal health. Similarly, Patton[21] identified smoking as a risk factor for severe periodontal disease in HIV patients. However, contrasting findings in Australia reported no significant association between smoking and oral health in patients with well-controlled HIV, likely due to robust oral health education programs.[21]
This study reported lower oral health-related quality-of-life impacts compared to Malaysia[16][17], where a prevalence of 33.9% was observed, in low-income populations, which reported 62.6%. The lower prevalence in this study could be attributed to the predominance of middle- and upper-socioeconomic status (SES) participants, which is associated with better oral health outcomes. Conversely, psychological discomfort as the most affected domain, whereas physical pain was predominant in this study, similar to findings by Santo.[17]
Nearly all participants required some form of dental treatment, with 82% needing fillings and 73% requiring extractions. This is consistent with studies in India[18] and in Zimbabwe[19], which reported similar high treatment needs among HIV-positive patients. However, findings from high-income countries like Canada[30] showed significantly lower treatment needs due to proactive dental interventions integrated into HIV care.
This study highlighted the beneficial impact of fluoride toothpaste on oral health status, aligning with findings by Shetty[20] who reported improved periodontal outcomes with fluoride use among HIV patients. However, these findings differ from Gathecha[25], who found that fluoride alone was insufficient to mitigate oral health challenges without comprehensive oral health education.
A weak positive correlation between age and oral health was observed, implying that older individuals may have slightly worse oral health. This aligns with another study[15], who noted age-related oral health decline in HIV patients, primarily due to cumulative effects of chronic illness and long-term ART.
This study's findings align with regional and global research, highlighting significant oral health issues among HIV-positive individuals, particularly periodontal disease and mucosal lesions. However, notable contrasts exist with studies from high-income countries, emphasizing disparities in healthcare access, ART coverage, and socioeconomic factors. Integrating oral health services into HIV care remains essential to address the treatment needs and improve the quality of life for people living with HIV/AIDS.
Multi-Variable Regression Results
Urban residents were significantly less likely to need dental treatment compared to their rural counterparts (OR=0.75, 95% CI: 0.44-0.99, p<0.001). This finding is consistent with global and regional studies, which highlight rural-urban disparities in access to healthcare. In sub-Saharan Africa, rural areas often face a lack of dental healthcare infrastructure and professionals, leading to unmet dental treatment needs.[26] In Zambia, similar trends have been observed, where urban centers are better equipped with dental clinics and specialists.[27]
Public health strategies should prioritize mobile dental clinics, community outreach programs, and training of rural healthcare workers to bridge this gap.
Older adults, particularly those aged 66-75 years, had significantly higher odds of needing dental treatment (OR=5.38, 95% CI: 1.62-17.80, p=0.006). This aligns with global patterns showing that oral health deteriorates with age due to cumulative exposure to risk factors and the aging process (Petersen & Ogawa, 2012). In sub-Saharan Africa, the limited focus on geriatric dental care exacerbates this issue.[25]
Targeted public health interventions are needed to integrate oral health into geriatric healthcare services, with a focus on preventive care for older adults in Zambia.
Patients with self-reported "excellent" oral health were less likely to need dental treatment (OR=0.07, 95% CI: 0.02-0.21, p<0.001), while those with "very good" oral health also had reduced odds (OR=0.05, 95% CI: 0.02-0.13, p<0.001). Conversely, patients reporting "poor" oral health were significantly more likely to require treatment (OR=2.74, 95% CI: 1.94-8.00, p=0.045). These results demonstrate the reliability of self-perceived oral health as a proxy for clinical needs, aligning with studies from other regions.[26]
Health literacy campaigns should be enhanced to improve individuals' awareness of their oral health, encouraging timely visits to dental clinics for preventive care.
Cleaning teeth twice or more daily was significantly associated with reduced odds of needing dental treatment (OR=0.16, 95% CI: 0.04-0.62, p=0.008). This supports evidence from the World Health Organization that regular tooth brushing with fluoride toothpaste can prevent dental caries and periodontal disease.[29] In sub-Saharan Africa, barriers such as limited access to affordable fluoride toothpaste hinder adherence to recommended practices.[30][31]
Public health efforts should promote the availability and affordability of fluoride toothpaste, along with education on proper tooth brushing techniques.
Patients living with HIV for more than four years were significantly more likely to need dental treatment (OR=3.30, 95% CI: 1.42-7.67, p=0.006). This reflects the long-term impact of HIV on oral health, including increased susceptibility to conditions such as oral candidiasis and periodontitis due to prolonged immunosuppression.[29] Studies in sub-Saharan Africa report similar findings, emphasizing the need for integrated oral healthcare services for PLWH.[28]
Incorporating dental care into HIV treatment programs is crucial to improve the quality of life for long-term HIV survivors in Zambia.
Patients who visited a dentist for routine check-ups or treatment were more likely to require dental treatment (OR=2.50, 95% CI: 1.03-6.04, p=0.042). This suggests a reactive approach to dental care, where patients seek help primarily when problems arise, rather than for preventive purposes. Globally, a similar trend is observed in resource-limited settings where prevention is often overlooked.[32] Public health initiatives should focus on promoting preventive dental care to reduce the burden of curative treatment.
CONCLUSION
The study concludes that periodontitis (48.5%) was the most prevalent oral mucosal lesion, followed by acute necrotizing ulcerative gingivitis. Approximately 2% of the participants had healthy periodontium, indicating a significant burden of oral health challenges among HIV-positive individuals. The mean Decayed, Missing, and Filled Teeth (DMFT) score was 4.03±1.54, reflecting considerable treatment needs. Oral manifestations remain critical diagnostic and prognostic indicators of HIV infection, with their presence often signalling early disease progression. Therefore, careful evaluation of individuals with HIV for these manifestations is essential for early detection and improved management of HIV infection.
Recommendations
- Oral Health Education and Integration
Emphasizing the importance of good oral health is crucial. A dentist should be placed at all ART centres to provide oral health education and address oral infections among immunosuppressed patients effectively.
- Provincial Studies
Further studies across various provinces of Zambia are needed, especially in the ART era, to monitor the changing prevalence of oral diseases, oral health status, and treatment needs among people living with HIV/AIDS (PLHIV).
- Collaboration Between Health Professionals
Strengthened coordination between medical and dental healthcare providers is essential. Regular screening for oral lesions should be integrated into routine HIV care, with clear referral systems and early management protocols to improve patient outcomes.
- Targeted Interventions
The study highlights the need for interventions addressing factors like tobacco and alcohol use, which contribute to poor oral health among PLHIV. Awareness campaigns targeting these behaviours could significantly improve overall outcomes.
- Resource Allocation
Government and stakeholders should allocate resources to ensure access to fluoride toothpaste and regular dental checkups, particularly for high-risk groups, to improve oral hygiene and reduce the prevalence of periodontal diseases.
Financial support and sponsorship: Nil
Conflicts of interest: There are no conflicts of interest.
REFERENCES
- Smith CJ, Ryom L, Weber R, et al. Trends in underlying causes of death in people with HIV from 1999 to 2011. Lancet HIV. 2020.
- World Health Organization. Global progress report on HIV, viral hepatitis, and sexually transmitted infections, 2021. Geneva: WHO; 2021.
- Centers for Disease Control and Prevention. Pneumocystis pneumonia — Los Angeles. MMWR Morb Mortal Wkly Rep. 1981;30(21):250–2.
- Joint United Nations Programme on HIV/AIDS (UNAIDS). Global HIV & AIDS statistics — 2020 fact sheet [Internet]. 2020 [cited 2023 Sep 3]. Available from: https://www.unaids.org/en/resources/fact-sheet
- Joint United Nations Programme on HIV/AIDS (UNAIDS). UNAIDS Data 2022. Geneva: UNAIDS; 2022.
- World Health Organization. Consolidated guidelines on HIV prevention, testing, treatment, service delivery, and monitoring: recommendations for a public health approach. Geneva: WHO; 2022.
- Ministry of Health Zambia. Zambia National Oral Health Policy 2020–2030. Lusaka: Ministry of Health; 2021.
- Johnson NW, Glick M, Mbuguye TL. Oral health and HIV/AIDS: A global perspective. J Dent Res. 2019;98(4):389–98.
- Greenspan D, Greenspan JS. HIV-related oral manifestations. Oral Surg Oral Med Oral Pathol. 1992.
- Singh A, Patel R, Sharma N, Gupta M. Gender differences in oral health among PLWH. J Oral Health Res. 2020.
- Denny CE, Patel V, Jones M, Rao K. Gender prevalence of HIV/AIDS. J AIDS Res. 2019.
- Sandeep A, Kumar V, Jain P, Reddy A. Periodontal health in HIV-positive individuals. J Clin Periodontol. 2018.
- Ranganathan K, Umadevi K, Saraswathi TR, Kumarasamy N, Solomon S. Oral manifestations of HIV infection. Indian J Dent Res. 2010.
- Duggal P, Naidoo S, Chikte UM. Oral lesions in South African HIV patients. S Afr Dent J. 2015.
- Gary S, Patel M, Johnson R, Smith D. Smoking and alcohol effects on oral health. J Public Health Dent. 2020.
- Ahmad F, Rahman ZA, Noor MM, Aris A. Oral health-related quality of life in Malaysian PLWH. J Health Psychol. 2018.
- Santo C, Ribeiro A, Pizarro M, Martins L. Oral health impacts in low-income populations. Eur J Oral Sci. 2015.
- Chaudhary R, Sharma P, Kumar A, Gupta S. Dental treatment needs in HIV patients in India. Int Dent J. 2020.
- Chidzonga MM, Mafeni MJ, Chokunonga E. Oral health needs in Zimbabwean HIV patients. J Oral Pathol Med. 2003.
- Shetty K, Rao N, Krishnan S, Patel R. Fluoride use in HIV-positive populations. J Dent Med. 2019.
- Patton LL, Santos GM, McKaig R, Strauss R. Oral health integration in HIV care. Am J Public Health. 2018.
- World Health Organization. Global progress report on HIV, viral hepatitis, and sexually transmitted infections, 2021. Geneva: WHO; 2021.
- World Health Organization. Consolidated guidelines on HIV prevention, testing, treatment, service delivery, and monitoring: recommendations for a public health approach. Geneva: WHO; 2022.
- Zambia Ministry of Health. Zambia Population-Based HIV Impact Assessment (ZAMPHIA) 2021. Lusaka: Ministry of Health; 2021.
- Gathecha G, Maina J, Kiboi J, Muasya M. Oral health disparities in sub-Saharan Africa: A review. Afr Health Sci. 2021;21(1):120–30.
- Locker D, Clarke M, Payne B. Self-perceived oral health and clinical outcomes in older adults. Community Dent Oral Epidemiol. 2002;30(1):3–9.
- Ministry of Health Zambia. Zambia National Oral Health Policy 2020–2030. Lusaka: Ministry of Health; 2021.
- Mwakatobe A, Mumghamba E. Oral health care barriers among HIV patients in resource-limited settings. Tanz Dent J. 2015;18(2):45–50.
- Patton LL, McKaig R, Strauss R, Eron JJ Jr. Oral health in HIV/AIDS: A global perspective. Oral Dis. 2008;14(Suppl 1):25–30.
- Petersen PE. The World Health Organization global policy for improvement of oral health. Community Dent Oral Epidemiol. 2003;31(Suppl 1):3–24.
- Varenne B, Petersen PE, Ouattara S. Barriers to oral health in rural sub-Saharan Africa. Community Dent Oral Epidemiol. 2015;43(2):99–107.
- Chaudhary P, Manral K, Gupta R, Bengani AK, Chauhan BI, Arora D. Oral health status and treatment needs among HIV/AIDS patients attending Anti-Retroviral Treatment Centre in Western India: A cross-sectional study. J Family Med Prim Care [Internet]. 2020 [cited 2020 Sep 3];9(7):3722–8. Available from: http://www.jfmpc.com/text.asp?2020/9/7/3722/290809
- Juma O, Saleh A, Eshraq ZE, Abdulwahab MA, Aesa AJ. Oral health status and treatment needs for children with special needs: a cross-sectional study. Pediatr Dent J [Internet]. 2019 [cited 2020 Sep 3];19(1):127. Available from: http://doi.org/10.4034/PB)CI.2019.191.127
- Vishnu V, Saxena V, Verma H, Jain M, Sharva V, Sathpathy M. Oral health status & treatment needs of patients attending anti-retroviral therapy among HIV patients in Government Medical College, Bhopal – A cross-sectional study. Dent Oral Maxillofac Res. 2019;5(1). DOI: 10.15761/DOMR.1000310
- Shirin S, Tahereh NZ, Hamideh K, Sarvir M. Dental health status of HIV-positive patients and related variables in Southeast Iran. Int J High Risk Behav Addict. 2016 Jun;5(2):e20149. DOI: 10.5812/ijhrba.29149
- Sandeep K, Prashant M, Shilpa W, Bhuvnesh A, Deepika J, Shaijal G. Oral health status and oromucosal lesions in patients living with HIV/AIDS in India: A comparative study. Hindawi
Medical Journal of Zambia, Vol 52, 2
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.