Severe Depressive Symptoms among Postpartum women with HIV in Lusaka, Zambia: Associated Factors and Optimal Cut-off Scores for the Edinburgh Postnatal Depression Scale (EPDS)
Margaret Kasaro
UNC Global Projects Zambia, Lusaka, Zambia
Bryan Blette
Vanderbilt University Medical Center, Department of Biostatistics, Nashville, United States
Bellington Vwalika
University of Zambia, School of Medicine, Department of Obstetrics and Gynaecology, Lusaka, Zambia
Ravi Paul
University of Zambia, School of Medicine, Department of Psychiatry, Lusaka, Zambia
Samantha Meltzer-Brody
University of North Carolina, School of Medicine, Department of Psychiatry, Chapel Hill, United States
Crystal E Schiller
University of North Carolina, School of Medicine, Department of Psychiatry, Chapel Hill, United States
J.M. Ncheka
University of Zambia, School of Medicine, Department of Psychiatry, Lusaka, Zambia
M. Bridget Spelke
University of North Carolina, School of Medicine, Department of Obstetrics and Gynecology, Chapel Hill, United States
Joni Price
University of North Carolina, School of Medicine, Department of Obstetrics and Gynecology, Chapel Hill, United States,
Jeffrey SA Stringer
University of North Carolina, School of Medicine, Department of Obstetrics and Gynecology, Chapel Hill, United States
Elizabeth M Stringer
University of North Carolina, School of Medicine, Department of Obstetrics and Gynecology, Chapel Hill, United States
DOI: https://doi.org/10.55320/mjz.51.4.451
Keywords:Postnatal depression; EPDS; MINI; Zambia
ABSTRACT
Background:
The Edinburgh Postnatal Depression Scale (EPDS) is a widely used tool for assessing postpartum depression, but its cut-off scores have not been examined in Zambia. The present study aimed to identify factors associated with severe depressive symptoms and determine the optimal cutoff scores for the EPDS among postpartum women with HIV in Lusaka, Zambia using the Mini International Neuropsychiatric Interview (MINI) as the gold standard.
Methods:
As part of a depression treatment trial, we screened HIV positive women with the EPDS between 6-10 weeks postpartum. To identify women at the lower symptom threshold, those scoring ≥6 (out of 30) on the EPDS were referred for a diagnostic Mini International Neuropsychiatric Interview (MINI). We investigated risk factors associated with severe depressive symptom scores. Additionally, we estimated the optimal EPDS screening threshold for probable diagnosis of depression with a receiver operating characteristic (ROC) curve. Based on literature, we defined an EPDS of 6-13 as “mild depressive symptoms” and an EPDS ≥14 as “moderate/severe depressive symptoms”.
Results:
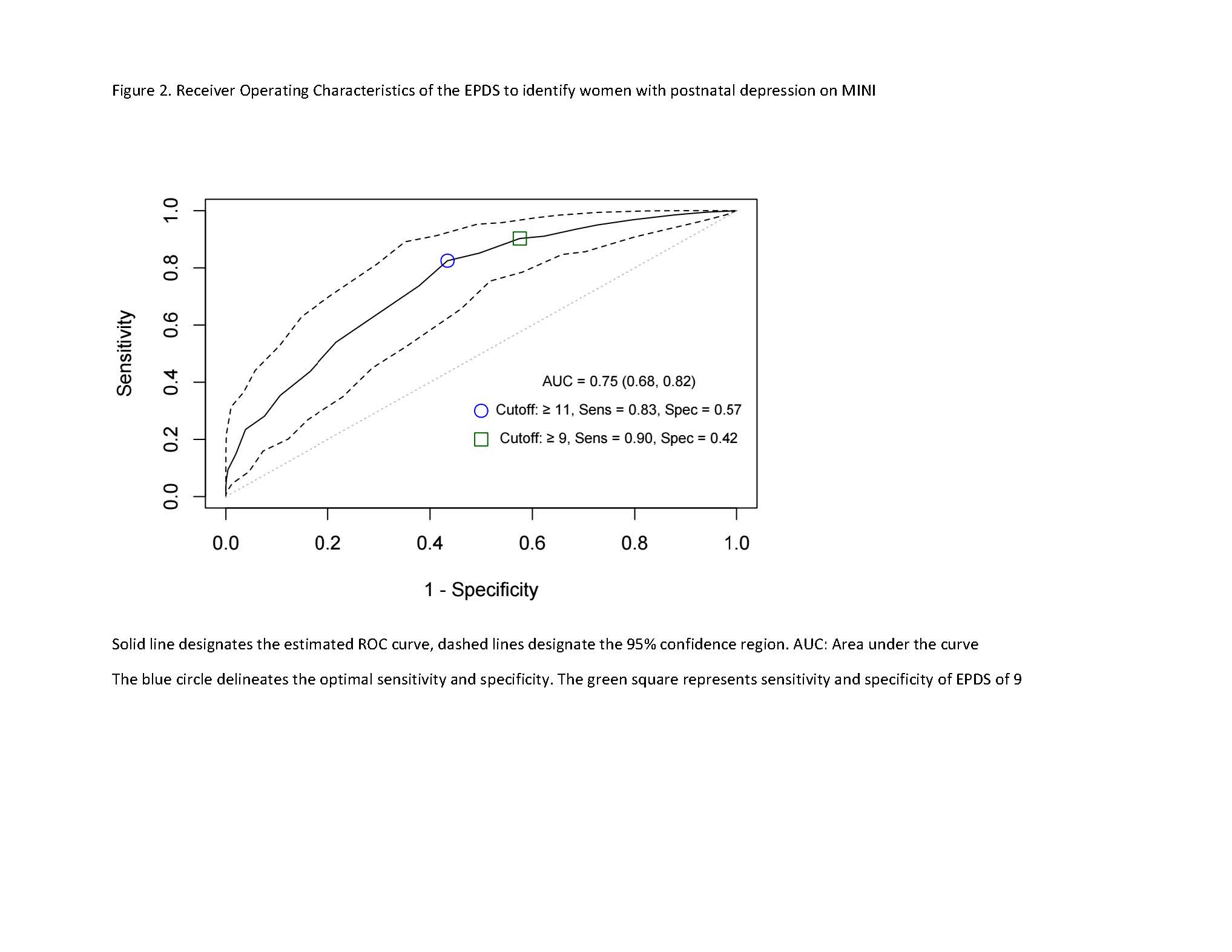
Out of 240 women screened, 192 (80%) scored ≥6 on the EPDS, of whom 120 (63%) agreed to undergo MINI evaluation. Of these, 61/120 (51%) scored between 6 and 13 (inclusive) and 59/120 (49%) scored ≥ 14. In unadjusted analysis, factors associated with severe depressive symptom scores were not being married or living with partner (odds ratio [OR]=3.11; 95% CI 1.03, 9.37; p=0.04) and having more life stressors (mean difference 1.0; 95% CI 0.2, 1.8; p=0.01). Having more life stressors remained significant in an adjusted logistic regression model (aOR 1.23; 95% CI 1.02,1.50; p=0.04), with each additional life stressor increasing odds of moderate/severe depression by 23%. An EPDS score of ≥11 performed best at discriminating MINI-diagnosed depression with a sensitivity of 83% and a specificity of 57%.
Conclusions:
An EPDS score ≥ 11 was the optimal threshold for determining probable depression in HIV positive postpartum women. Women with a greater number of life stressors were more likely to score higher on the EPDS.
INTRODUCTION
The WHO estimates the worldwide prevalence of postnatal depression to be 13% and in sub-Saharan Africa, where screening and treatment are very limited, it approaches 20%.[1] Sub-Saharan Africa also bears the highest burden of HIV among pregnant and breastfeeding women.[1] With widespread access to antiretrovirals, maternal-child transmission of HIV has significantly improved, and the overall prevalence of HIV among pregnant women has also been declining.[2] Despite these recent gains, a diagnosis of HIV still carries tremendous stigma in many settings.[3] Studies have shown that people living with HIV are particularly vulnerable to mental health problems, including depression,[4] and that in the general population, women may present with more severe symptoms of depression than men.[5] Postnatal depression presents a unique public health challenge in the setting of HIV. Many of the hallmark features of depression, such as sadness, fatigue, and withdrawal, work directly against a woman’s ability to care for herself and her baby and may interfere with adherence to her HIV treatment.6
Postnatal depression is commonly screened for using the Edinburgh Postnatal Depression Scale (EPDS), a standardized, 30-point tool comprising 10 questions, each with a maximum of three points.[7] In Zambia, a cross-sectional study at The University Teaching Hospital screened 229 women for postnatal depression using the EPDS and found that 64 women (28%) met the criteria for severe postnatal depression defined as an EPDS score ≥13.[8] A second study conducted at an antenatal clinic in Lusaka, identified 26% women as having symptoms suggestive of antenatal depression based on an EPDS score >11.[9] This study and one other in Zambia, assessed the validity of alternative screening scales used to screen for psychological distress against the EPDS as the reference standard.[10] Although the EPDS was not initially created as a diagnostic tool, it has come to be used as such in both local and international settings because of its simplicity and ease of administration compared to a diagnostic assessment such as the Mini International Neuropsychiatric Interview (MINI).[11,12] The MINI takes between 15 and 30 minutes to complete,[13,14] while the EPDS takes about five minutes. The EPDS has been validated as a diagnostic tool using various threshold scores in Zambia’s neighbouring countries, Zimbabwe and Malawi, as well as a number of other low resource settings.[15] The published range of threshold scores for diagnosing depression has been reported to be from 9 to 13 points,[7,16,17] but it has not been validated against a gold standard in our setting in Zambia. In this study, we leveraged the concomitant administration of the EPDS and the MINI in the parent trial to assess the sensitivity and specificity of the EPDS for diagnosing postnatal depression in women living with HIV in Lusaka, Zambia. We additionally assessed factors associated with EPDS severity in this at-risk population.MATERIALS AND METHODS
The study used data collected during a pilot randomized trial of antidepressant medication versus interpersonal psychotherapy for the treatment of postnatal depression and anxiety among women with HIV (NCT: 04094870).[18] Data were collected between October 29, 2019, and September 8, 2021. Trial recruitment activities included community sensitization and health care provider education at Kamwala Health Centre (KHC), one of 24 public-sector antenatal facilities in Lusaka, Zambia. The recruitment activities at the clinic included the study staff making presentations and participating in the health education sessions at the MCH department to promote messages and education about HIV testing, mental health, what postnatal depression is, and the purpose of the parent trial. Women interested in participation and who met inclusion criteria (≥18 years old, 6-8 weeks postpartum, confirmed HIV infection receiving antiretroviral therapy, and living infant from the most recent delivery) were eligible to be pre-screened with the EPDS.
As previously described, research nurse midwives received in-person and virtual training in mental health assessment and treatment[18] Nurses administered the EPDS and women scoring ≥6 were given more information about the study. We used an EPDS score ≥6 based on evidence from prior postnatal depression studies in Malawi[19] and to maximize sensitivity of the screening test. Prior to administration of the diagnostic MINI assessment, we obtained written informed consent. Women with EPDS ≥ 6 but who did not want to participate in the study were referred for care at the psychiatric clinic at the University Teaching Hospital (UTH).
No identifiable information about individual women was recorded for study purposes until after informed consent had been provided. After consenting for participation, the EPDS individual question results were documented, and the MINI was performed using the mood modules to diagnose depression and anxiety. If the participant was not depressed based on the MINI, she was exited from the study. Questionnaires were administered to collect data on sociodemographic, reproductive and life stressors, and domestic/gender-based violence. To assess for life stressors, we asked if participants had in the last six months experienced challenges such as marital and relationship difficulties, death or injury of a loved one, financial and work challenges, loss of property, and problems with the law. The HIV history and serostatus was verified from participants’ postnatal cards and HIV clinic charts. Data were collected and stored in the REDCap electronic data capture tool hosted at the University of North Carolina (USA).[20]
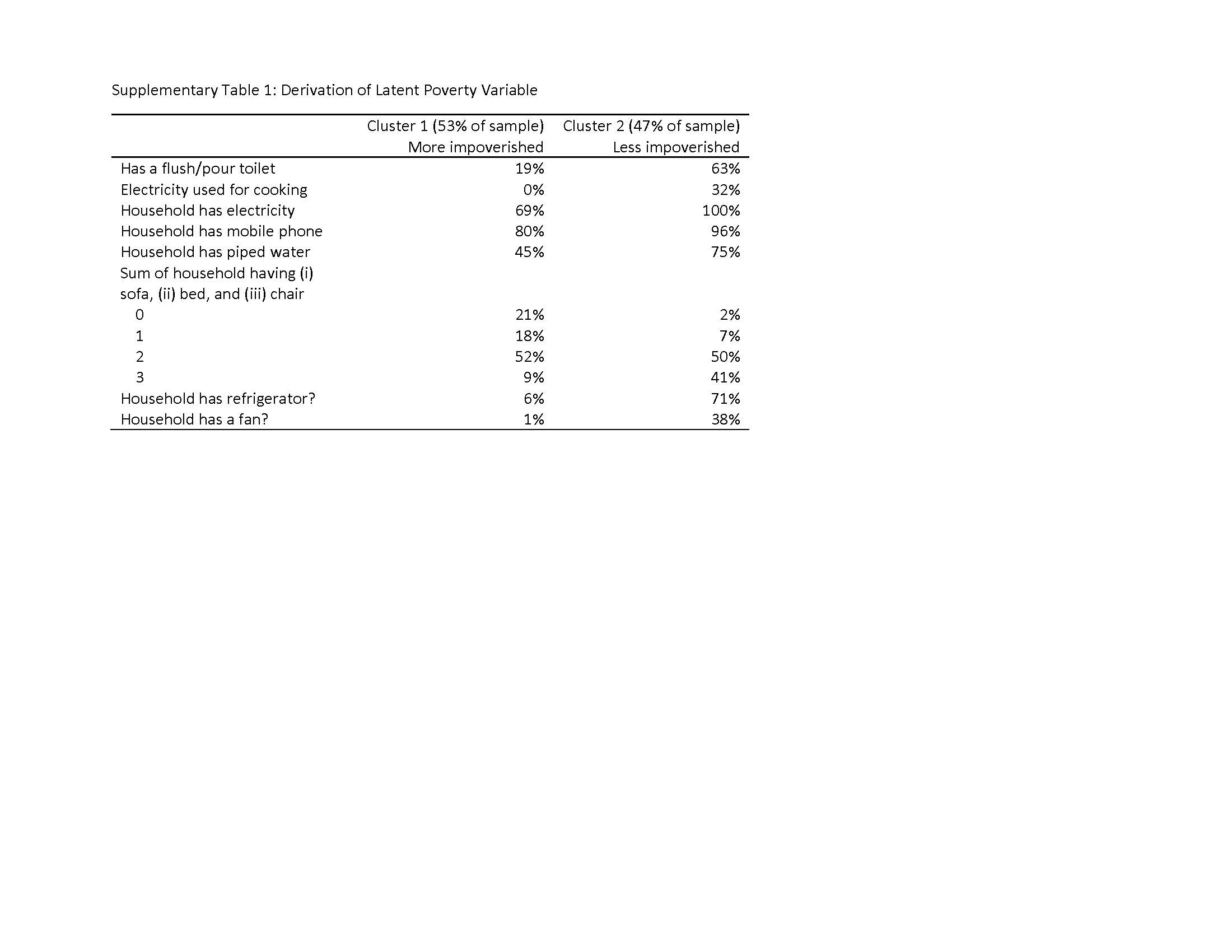
A poverty index variable was derived using latent class analysis. This analysis stipulated wealth as measured by the following variables: type of toilet, electricity for cooking and for the household, piped water possession of mobile phone and household items like a refrigerator. The algorithm clustered individuals into similar groups based on their characteristics. Models were fit using two through five clusters; two clusters emerged as a best fit for the data using AIC and BIC metrics and the model returned as a best fit with 53% of our sample and another cluster with 47% of our sample.[21]
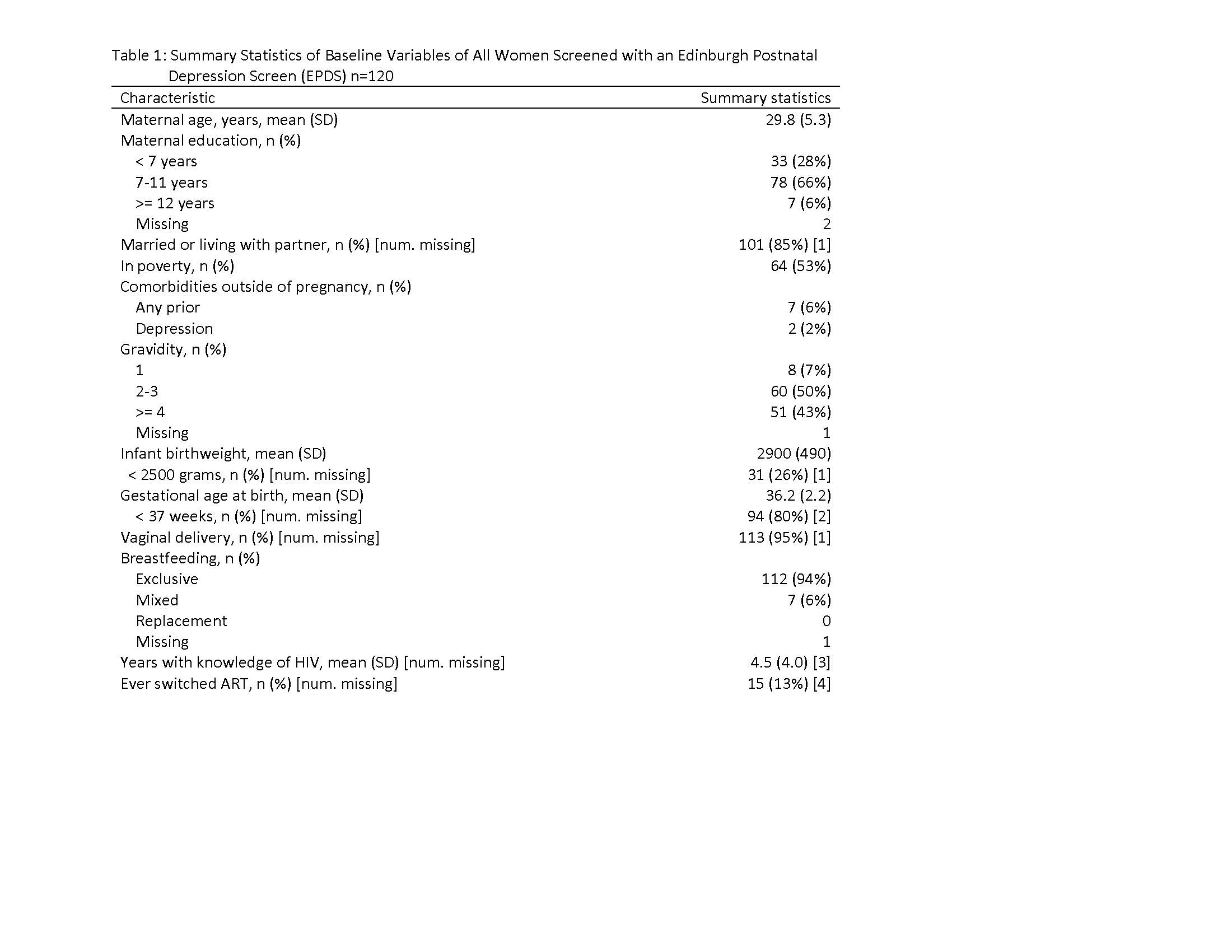
(Table 1; supplementary materials)
Ethical approval for the study was obtained from the University of Zambia Biomedical Research Ethics Committee UNZABREC, reference number: 1404-2020 and the University of North Carolina IRB: 17-2107. Formal permission to conduct the research was also obtained from Zambia’s National Health Research Authority. All participants provided written informed consent.
Statistical Analysis
Baseline variables were summarized with means and standard deviations for continuous variables or counts and percentages for binary and categorical variables. The results of the EPDS were categorized accordingly: “EDPS mild depressive symptoms” if the score was between 6 to 13 and “EPDS Moderate/Severe depressive symptoms” if the score was ≥ 14. T-tests were used to compare continuous variables across depression severity and their corresponding p-values and confidence intervals were reported. Odds ratios and Wald confidence intervals were calculated for each binary and categorical variable cross-classified with depression severity, where one category was chosen as a reference level for each categorical variable. A mid-P exact test was used whenever a table cell had less than 5 participants. Then an adjusted logistic regression model was fit including all variables with p<0.05 in the univariate analysis.
A receiver operating characteristic (ROC) analysis was performed to evaluate the performance of the EPDS in identifying women with probable postnatal depression, treating the MINI as the gold standard diagnostic tool.22 Under the parent trial procedures, only consented individuals with EPDS ≥ 6 were given the MINI assessment and this was accounted for in the analysis to avoid verification bias. Thus, the final ROC curve was estimated using a mean score imputation procedure,23 which assumed a logistic regression model with MINI diagnosis as the outcome and EPDS score as an independent variable. The imputation procedure also included those with EPDS ≥ 6 who declined to receive the MINI assessment.
All statistical analyses were conducted using R version 4.0.2.[24]
RESULTS
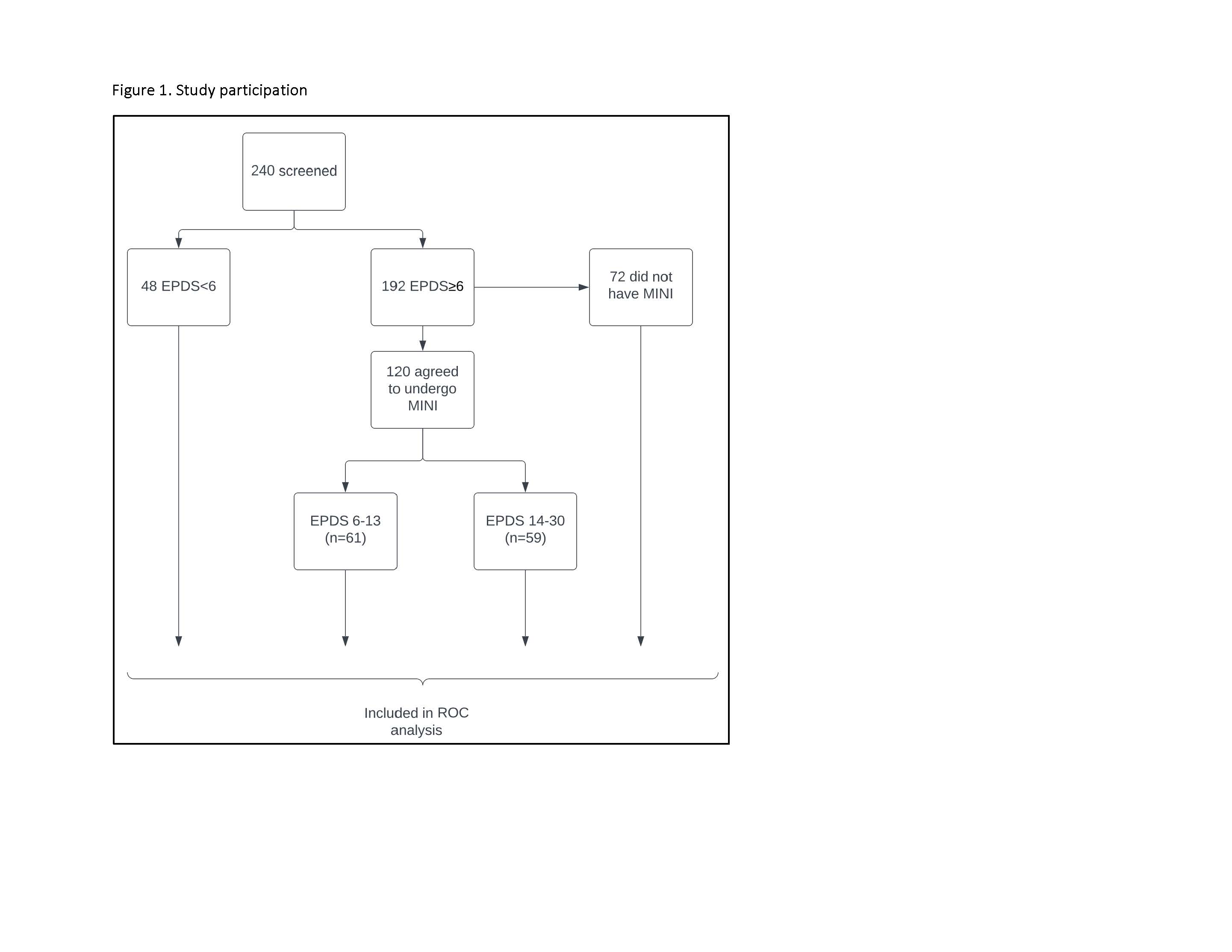
Between October 2019 and April 2020, 240 women were pre-screened with EPDS of whom 192 (80%) scored ≥6. (Figure 1) Some women (n=72) who pre-screened EPDS-positive did not return or were not interested in further testing with the MINI. Of the 120 who went on to complete the diagnostic MINI, 61 (51%) scored between 6 and 13 (inclusive) on EPDS and were thus categorized as “mild depressive symptoms,” while 59 (49%) had scored ≥ 14 and were thus categorized as “moderate/severe depressive symptoms”. 91/120 (75.8%) met criteria for major depressive disorder on the MINI.
Baseline Characteristics of Participants
The mean age of the 120 participants who completed both the EPDS and MINI was 29.8 years (SD 5.3) (Table 1). Two thirds of the participants had between 7 and 11 years of education and most women were married or living with a partner. The proportion of those who were more impoverished based on the poverty index was 53%. Ninety-three percent of participants were multiparous and 95% had had a vaginal delivery in the most recent pregnancy. The mean birthweight was 2900 grams (SD 490 grams). 94% reported exclusively breastfeeding their babies. Very few participants reported known medical comorbidities (6%) or prior depression (2%). Of all participants, the mean number of years of knowledge of HIV status was 4 and a half years (SD 4). All women were taking antiretrovirals and 15 women (13%) reported ever switching their antiretroviral.
Factors associated with higher EPDS scores
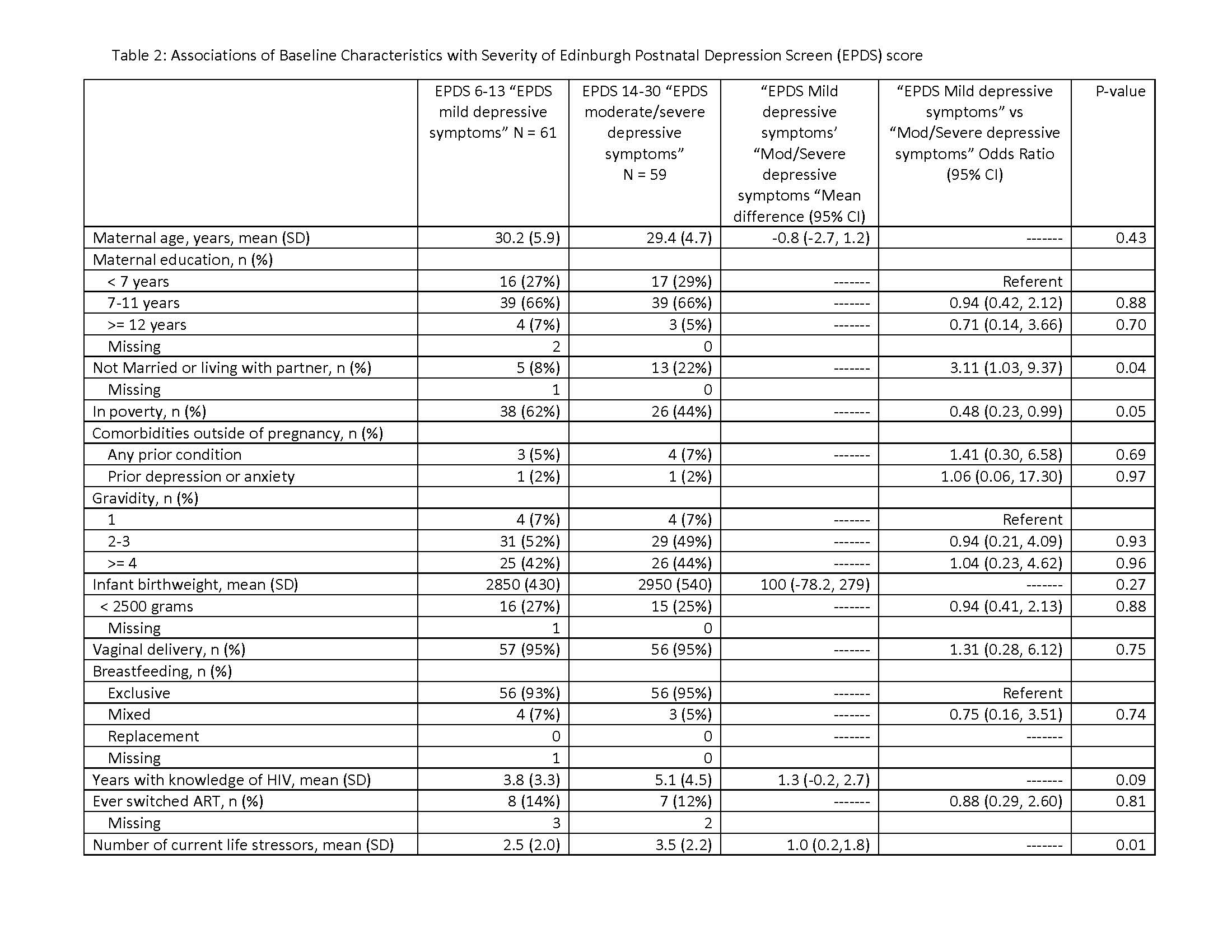
In unadjusted analysis, factors associated with EPDS “moderate/severe depressive symptoms” were not being married or living with partner (odds ratio [OR]=3.11; 95% CI 1.03, 9.37; p=0.04) and having more life stressors (mean difference 1.0; 95% CI 0.2, 1.8; p=0.01). (Table 2) A logistic regression model was fit to estimate adjusted odds ratios. In the adjusted analysis, not being married or living with a partner was no longer statistically significant but retained a large effect size (adjusted odds ratio [aOR] 2.56; 95% CI 0.88, 9.09; p=0.10). Having more life stressors remained significant in the adjusted model (aOR 1.23; 95% CI 1.02,1.50; p=0.04), with each additional life stressor increasing odds of moderate/severe depression symptoms by 23%.
Optimal EPDS threshold defining depression
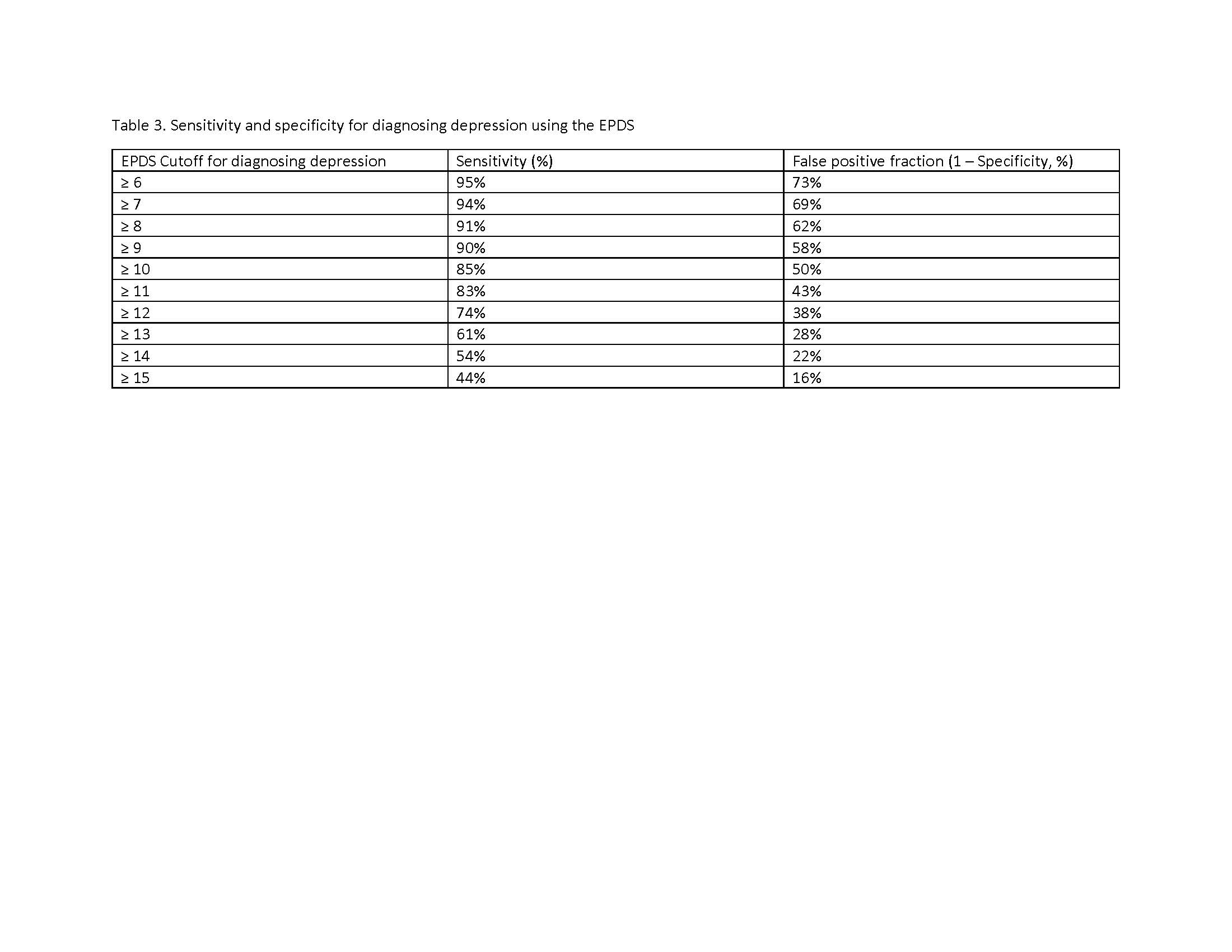
The estimated receiver operating characteristic curve is displayed in Figure 2. Using the MINI as the gold standard, the area under the curve (AUC) was 0.75 (CI 0.68-0.82). An EPDS score of ≥11 performed best at discriminating major depressive disorder with a sensitivity of 83% and specificity of 57%. We also calculated the results using a cutoff score ≥9. In this scenario, the sensitivity increased to 90% but at the expense of specificity which decreased to 42%. Of the women with an EPDS score of 6-10, 23% were determined to have depression on the MINI. Among women with EPDS ≥11, 77% were diagnosed with depression on the MINI (Table 3).
DISCUSSION
In our setting, using an EPDS ≥ 11 seemed to have the best combination of sensitivity and specificity for determining probable major depressive disorder in HIV positive postpartum women in Zambia. Among the 120 postpartum HIV positive women included in this analysis, approximately half had an EPDS score ≥14 which we defined as “moderate to severe depressive symptoms”. Having a greater number of life stressors was associated with a higher EPDS score.
Life stressors can have a significant impact on one’s perception of social support.[25,26,27] Social support refers to emotional, financial, intellectual, and empathetic support.[28] The role of social support in reducing postnatal depression is essential, especially in settings where family and community play such vital and important roles.[26,27,29,30] The onset of depression and anxiety may be triggered by the perception of or actual decreased social support.,27,29,30,31,32]
In our study, not living with a husband or partner was associated with a higher EPDS score and retained a strong effect size even after adjusting for other covariates. Some studies have shown that domestic violence during pregnancy contributes to the incidence of postnatal depression.[29,33] Marital problems, unfaithfulness, and lack of support from the spouse have also been shown to increase the risk of postnatal depression.[25,27]25,27 However, living with a partner or husband may also create stability, especially financial stability, which may improve a woman’s mental health if she has decision-making power at home and has increased support from her partner.[34]
Some studies have shown that being employed has been associated with a reduced risk of postnatal depression.[35] Low education and low income, on the other hand, have been associated with an increased risk of postnatal depression.[29,36,37] In contrast, our study found that women with a higher poverty index (greater wealth) were more likely to have lower EPDS scores. It is possible that since the majority of women in our study met criteria for living in poverty, the poverty index may not be that discriminatory.
An EPDS score of at least 11 performed best at discriminating any depression from no depression. In a recent meta-analysis, Levis et al evaluated the EPDS for screening to detect major depression in pregnant and postpartum women.[38] They also found that among 22788 participants, the combined sensitivity and specificity of the EPDS was maximized at a cut-off value of 11 or higher.
Strengths of our study include the use of the MINI as a diagnostic tool compared to the EPDS and that we engaged trained nurses and midwives to screen for depression and anxiety with the EPDS and diagnose depression with the MINI. A limitation of our study is that we did not complete the MINI assessment for all postnatal women screened with the EPDS. We address this limitation by imputing MINI outcomes for women scoring ≤6 on the EPDS. Additional weaknesses include the small sample size of the study and the inability to control for factors about which we did not ask that may have confounded the relationship between the predictors and the outcome variable. Finally, the EPDS was not self-administered as it is commonly performed in higher resource settings, which may have affected the way in which participants answered the questions.
Apart from the one study that examined the prevalence of postnatal depression among women at the University Teaching Hospital in Lusaka,[8] limited information exists on the burden of postnatal depression among HIV-positive women in Zambia, which poses a real challenge for resource allocation and formulating interventions. Determining the prevalence of postnatal depression, finding the optimal EDPS score for a probable diagnosis of postpartum depression, and characterizing factors associated with symptom severity among HIV positive women will help identify those women at most risk and catalyze tailored services for this group of women. It will also stimulate additional research questions that could produce information towards further improvement in mental health services among HIV positive women. Finally, in most high-income countries, the EPDS is self-administered which may also be possible in Zambia, and therefore exploring this method to scale up screening for depression is an important area of research.
CONCLUSION
We found that among women screened for our study with the EPDS, 49% had severe depressive symptoms (EPDS ≥ 14). Women with moderate to severe depressive symptom scores on the EPDS had a greater number of life stressors and were less likely to be living with a partner. In our setting, an EPDS ≥ 11 is the optimal threshold for determining probable depression in HIV positive postpartum women in Zambia to maximize both sensitivity and specificity. These findings are important in identifying women at most risk and may aid formulation of tailored services for this group of women. In addition, the data will stimulate additional research questions for further improvement in mental health services among HIV positive women.
Acknowledgements
We would like to acknowledge all of the study participants and the study team at Kamwala Health Center in Lusaka, Zambia.
Funding
This study was supported by a grant from NIMH (PI: Stringer, E.; NIMH 1R21MH115806) and NC Translational and Clinical Sciences (NC TraCS) Institute, National Institutes of Health, through Grant Award Number UL1TR002489.
These results were presented at the International AIDS Conference July 18-21 2021 in Berlin, Germany.
TABLES
REFERENCES
- WHO. Maternal and Child Mental Health. 2020.
- Eaton JW, Rehle TM, Jooste S, Nkambule R, Kim AA, Mahy M, et al. Recent HIV prevalence trends among pregnant women and all women in sub-Saharan Africa: implications for HIV estimates. AIDS. 2014;28 Suppl 4:S507-14.
- Bonnington O, Wamoyi J, Ddaaki W, Bukenya D, Ondenge K, Skovdal M, et al. Changing forms of HIV-related stigma along the HIV care and treatment continuum in sub-Saharan Africa: a temporal analysis. Sex Transm Infect. 2017;93(Suppl 3).
- Niu L, Luo D, Liu Y, Silenzio VM, Xiao S. The Mental Health of People Living with HIV in China, 1998-2014: A Systematic Review. PLoS One. 2016;11(4):e0153489.
- Reis RK, Haas VJ, Santos CB, Teles SA, Galvao MT, Gir E. Symptoms of depression and quality of life of people living with HIV/AIDS. Rev Lat Am Enfermagem. 2011;19(4):874-81.
- Association AP. Diagnostic and Statistical Manual of Mental Disorders. Washington DC: American Psychiatric Association; 2013.
- Cox JL HJ, Sagovsky R. . Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782-6.
- Cyimana A, Andrews B, Ahmed Y, Vwalika B. HIV/AIDS and Postnatal Depression at the University Teaching Hospital, Lusaka, Zambia. Med J Zambia. 2010;37(2):78-83.
- Maila B, Paul, R., Mayimbo, S., & Kabwita, K. . Prevalence and correlates of antenatal depression at Chelstone First Level Hospital in Lusaka, Zambia: A cross-sectional study. African Health Sciences. 2022;22(4):334-47.
- Maila B PR, Mayimbo S, Kabwita K. . The Validity of The Patient Health Questionnaire-2 As A Depression Screening Tool in Women Receiving Antenatal Care at Chelstone First Level Hospital, Lusaka, Zambia. JPRM2022. 2022;4(1):27-34.
- Sheehan DV LY, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. . The Mni-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22-33.
- Sheikh WA J, D. M., Msoni, P., Paul, R., & Maila, B. . A Comparative Analysis of Zambia’s Mental Health Legislation and the World Health Organisation’s Resource Book on Mental Health, Human Rights and Legislation. Medical Journal of Zambia. 2021;47(4):327-34.
- van Vliet IM dBEH. The MINI-International Neuropsychiatric Interview. A brief structured diagnostic psychiatric interview for DSM-IV en ICD-10 psychiatric disorders. Tijdschr Psychiatr. 2007;49(6):393-7.
- Pettersson A, Modin S, Wahlstrom R, Af Winklerfelt Hammarberg S, Krakau I. The Mini-International Neuropsychiatric Interview is useful and well accepted as part of the clinical assessment for depression and anxiety in primary care: a mixed-methods study. BMC Fam Pract. 2018;19(1):19.
- Chibanda D, Mangezi W, Tshimanga M, Woelk G, Rusakaniko P, Stranix-Chibanda L, et al. Validation of the Edinburgh Postnatal Depression Scale among women in a high HIV prevalence area in urban Zimbabwe. Arch Womens Ment Health. 2010;13(3):201-6.
- Chibanda D MW, Tshimanga M, et al. . Validation of the Edinburgh Postnatal Depression Scale among women in a high HIV prevalence area in urban Zimbabwe. Arch Womens Ment Health. 2010;13(3):201-6.
- Gibson J M-MK, Shakespeare J, Price J, Gray R. . A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. 2009;119(5):350-64.
- Spelke MB PR, Blette BS, Meltzer-Brody S, Schiller CE, Ncheka JM, Kasaro MP, Price JT, Stringer JSA, Stringer EM. . Interpersonal therapy versus antidepressant medication for treatment of postpartum depression and anxiety among women with HIV in Zambia: a randomized feasibility trial. . J Int AIDS Soc 2022;25(7).
- Harrington BJ, Hosseinipour MC, Maliwichi M, Phulusa J, Jumbe A, Wallie S, et al. Prevalence and incidence of probable perinatal depression among women enrolled in Option B+ antenatal HIV care in Malawi. J Affect Disord. 2018;239:115-22.
- Harris PA T, R., Thielke, R., Payne, J., Gonzalez, N., Conde, J.G. . Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42:377-81.
- Linzer DA LJ. poLCA: An R Package for Polytomous Variable Latent Class Analysis. Journal of Statistical Software,. 2011;42(10):1-29.
- Robin X T, N., Hainard, A., Tiberti, N., Lisacek, F., Sanchez, J.C. and Müller, M. . pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC bioinformatics. 2011;12(1):1-8.
- Alonzo TA. PMS. Assessing accuracy of a continuous screening test in the presence of verification bias. Journal of the Royal Statistical Society: Series C (Applied Statistics). 2005;54(1):173-90.
- Team RC. R: A language and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Austria2021.
- Dadi AF, Akalu TY, Baraki AG, Wolde HF. Epidemiology of postnatal depression and its associated factors in Africa: A systematic review and meta-analysis. PLoS One. 2020;15(4):e0231940.
- Escribà-Agüir V, Artazcoz L. Gender differences in postpartum depression: a longitudinal cohort study. Journal of Epidemiology and Community Health. 2011;65(4):320-6.
- Kakyo TA, Muliira JK, Mbalinda SN, Kizza IB, Muliira RS. Factors associated with depressive symptoms among postpartum mothers in a rural district in Uganda. Midwifery. 2012;28(3):374-9.
- Feng Z, Jones K, Wang WW. An exploratory discrete-time multilevel analysis of the effect of social support on the survival of elderly people in China. Social Science & Medicine. 2015;130:181-9.
- Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry. 2016;3(10):973-82.
- Dibaba Y, Fantahun M, Hindin MJ. The association of unwanted pregnancy and social support with depressive symptoms in pregnancy: evidence from rural Southwestern Ethiopia. BMC Pregnancy Childbirth. 2013;13:135.
- Landman-Peeters KMC, Hartman CA, van der Pompe G, den Boer JA, Minderaa RB, Ormel J. Gender differences in the relation between social support, problems in parent-offspring communication, and depression and anxiety. Social Science & Medicine. 2005;60(11):2549-59.
- Shitu S, Geda B, Dheresa M. Postpartum depression and associated factors among mothers who gave birth in the last twelve months in Ankesha district, Awi zone, North West Ethiopia. BMC Pregnancy Childbirth. 2019;19(1):435.
- Ludermir AB, Lewis G, Valongueiro SA, de Araújo TVB, Araya R. Violence against women by their intimate partner during pregnancy and postnatal depression: a prospective cohort study. The Lancet. 2010;376(9744):903-10.
- Galvão J. Brazil and Access to HIV/AIDS Drugs: A Question of Human Rights and Public Health. American Journal of Public Health. 2005;95(7):1110-6.
- Miyake Y, Tanaka K, Sasaki S, Hirota Y. Employment, income, and education and risk of postpartum depression: The Osaka Maternal and Child Health Study. Journal of Affective Disorders. 2011;130(1):133-7.
- Huang T, Rifas-Shiman SL, Ertel KA, Rich-Edwards J, Kleinman K, Gillman MW, et al. Pregnancy Hyperglycaemia and Risk of Prenatal and Postpartum Depressive Symptoms. Paediatric and Perinatal Epidemiology. 2015;29(4):281-9.
- Chien L-Y, Tai C-J, Yeh M-C. Domestic Decision-Making Power, Social Support, and Postpartum Depression Symptoms Among Immigrant and Native Women in Taiwan. Nursing Research. 2012;61(2):103-10.
- Levis B, Negeri Z, Sun Y, Benedetti A, Thombs BD, Group DESDE. Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for screening to detect major depression among pregnant and postpartum women: systematic review and meta-analysis of individual participant data. BMJ. 2020;371:m4022.
Medical Journal of Zambia, Vol 51, 4
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.