Lipoprotein (a) as a cause of premature coronary artery disease; a case report of a 34-year-old male patient presenting to a specialist heart hospital in Lusaka, Zambia
Edward Kateta
National Heart Hospital, Lusaka, Zambia.
Jane Chanda Kabwe
National Heart Hospital, Lusaka, Zambia.
Agnes Mtaja
National Heart Hospital, Lusaka, Zambia.
Lorrita Kabwe
National Heart Hospital, Lusaka, Zambia.
DOI: https://doi.org/10.55320/mjz.50.3.403
Keywords:Early onset coronary artery disease, lipoprotein (a), chest pain, percutaneous coronary intervention, case report.
ABSTRACT
Background: Premature coronary artery disease (PCAD) is considered when coronary artery disease (CAD) occurs in the younger population, less than 45 years old in males. Modifiable risk factors are present in about 80% of patients with PCAD such as smoking, diabetes, high blood pressure and obesity. High serum lipoprotein (a) level has recently emerged as a risk factor for PCAD. However, it is not routinely investigated in young patients presenting with acute coronary syndromes.
Case Presentation: A 34-year-old African man presented to our hospital with 2 hours of worsening left sided chest pain. He gave a history of long-standing chest pain in the past that was being managed as peptic ulcer disease. He also complained of a slow heart rate. He had no traditional cardiovascular risk factors. The only significant history was a recent recovery from COVID-19 infection two months prior. His physical examination was only significant for a bradycardia, ECG revealed a hyper acute inferior STEMI without right ventricular involvement. Echo showed a normal left ventricle with reduced ejection fraction (EF: 50%), wall motion abnormalities consistent of an inferior MI. He immediately received streptokinase with good clinical and ECG response. His coronary angiogram showed a severe lesion and plaque rupture in the mid-distal segment of a dominant right coronary artery. Percutaneous coronary intervention (PCI) was successfully done, and one drug eluting stent was implanted. He was placed on guideline directed medical therapy for secondary prevention. The only significant possible aetiology found was an elevated Lipoprotein (a) (137mg/dl). Subsequent serum Lipoprotein (a) remained persistently elevated despite therapy with high dose niacin. He was recommended for a PCSK9 receptor blocker, but this medication is not available in the country and the patient could not meet the costs. He remains stable to current medications with no recurrence of chest pain, two years after the index event, the Lipoprotein (a) levels are still high.
Conclusions: Lipoprotein (a) appears to be an important overlooked cardiovascular risk factor for premature coronary artery disease especially in the absence of traditional risk factors. It should always be considered in the screening of premature coronary cardiovascular disease. The acute presentation in this patient was probably triggered by SARS COV-2 infection.
INTRODUCTION
Acute coronary syndrome (ACS) is a rare occurrence in the younger population and literature focussing on myocardial infarction in the young is lacking [1] , but most studies acknowledge the fact that ACS is an increasing health problem in the young adults [2] . Smoking, obesity, diabetes mellitus, intravenous drug use and other risk factors like Protein C or Protein S deficiency, Factor V Leiden, homocysteinemia, autoimmune diseases, familial hypercholesterolemia and hyperhomocysteinemia have been suggested as some of the major promoters of atherosclerosis causing coronary artery disease (CAD) in young adults presenting with premature coronary atherosclerotic myocardial infarction. Recently, a high serum lipoprotein(a) level has emerged as a risk factor for premature coronary artery disease (PCAD) though there is currently no adequate available data on the role of lipoprotein (a) in ST elevation myocardial infarction in young people with normal serum LDL cholesterol. We present a case of a 34-year-old African man that was successfully treated for an ST elevation myocardial infarction (STEMI).
CASE PRESENTATION
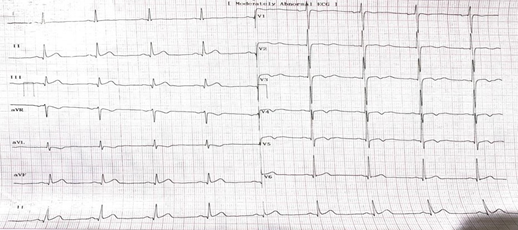
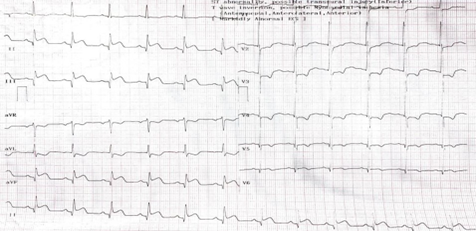
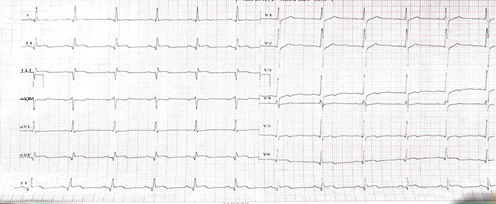
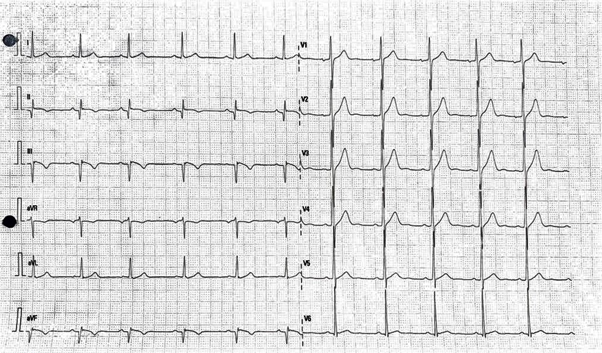
A 34-year-old man presented to our hospital with 2 hours of severe left sided chest pain which is said to have started soon after waking up in the morning. The chest pain was radiating to the left arm with an associated feeling of slowing heart rate. He suffered from COVID-19 pneumonia two months prior to the above presentation and reported an increase in frequency of chest pain after this. He gave a history of experiencing episodes of mild chest pain for ten years and was treated as possible peptic ulcer disease. He had no risk factors for coronary artery disease; in particular, he denied smoking or intravenous drug use, he was not a known diabetic and had normal blood pressure. There was no family history of CAD either. His vital signs were as follows: Blood Pressure 128/90mmHg, Temperature 35.2 ◦C, Pulse 55 breaths per minute and saturations 98% on room air. His body mass index (BMI) was 25.9, the physical examination was only significant for bradycardia. A series of electrocardiograms (ECGs) were performed at 10-minute intervals which showed an evolution of an inferior STEMI (ST elevation in Leads II, III and aVF) with reciprocal changes in the high lateral leads (Figures 1,2 and 3). There was no atrio-ventricular block but only a sinus bradycardia; Lead V4R was also done but was negative for ST elevation to indicate right ventricular involvement. A diagnosis of a hyper acute inferior STEMI in a young adult was made. Immediate point of care echo revealed normal left ventricle size with low normal systolic function (EF 50%), inferior wall hypokinesia, normal valve function and no evidence of dissection in ascending arch and abdominal aorta. The plan was to start immediately with medical treatment whilst awaiting for non-invasive intervention as per guidelines. Successful lysis was achieved after administration of streptokinase 1,500,000 units over 30minutes. There was resolution of chest pain and reduction in the ST elevation by more than 50% (figure 4).
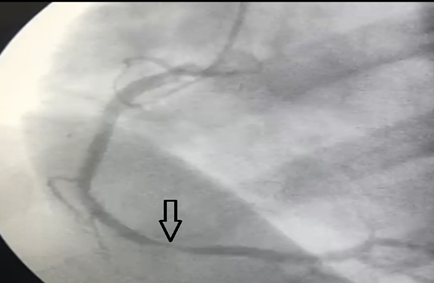
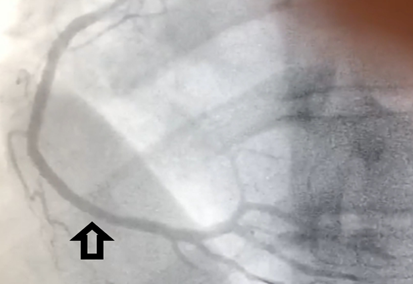
The patient then underwent coronary angiography which showed plaque rupture and a 90% stenosis in the mid-distal segment of a dominant right coronary artery just before the posterior descending artery (PDA) take-off (figure 5). Standard percutaneous coronary intervention (PCI) was done; A 3.0 x 18 mm Ultimaster Tensei drug eluting stent (DES) was deployed at the lesion with good final angiographic result - stent well expanded, TIMI III flow, no edge dissection (Figure 6). Post stent ECG showed resolved ST elevations with pathological Q waves in inferior leads (figure 7). Repeat echocardiography showed right coronary artery (RCA) territory hypokinesia and an EF of 55-60%. He was placed on guideline directed medical therapy which included aspirin, clopidogrel, atorvastatin, enalapril and carvedilol. Blood test results included HIV which was negative, normal full blood counts, kidney and liver function tests and a normal lipid panel. We further did additional tests including C-reactive protein, HBA1C, Protein C and S, anticardiolipin antibodies and anti-prothrombin which were all normal. Since no obvious risk factor was found on the usual investigations, we proceeded to do a lipoprotein(a) test, which result showed elevated levels at 137mg/dl (<50mg/dl). Despite Niacin and statin therapy, the levels have remained elevated with no indication of a downward trend (153mg/dl February 2023). He is not able to afford a PCSK9 inhibitor and which is not available in the country.

DISCUSSION
Compared to older people, myocardial infarction is uncommon in young adults with or without traditional cardiovascular risk factors; in the Framingham heart study conducted four decades ago [3] , the incidence of myocardial infarction over a 10 year follow up was 12.9/1000 in men aged 30 to 34years and 5.2/1000 in women aged 35 to 44 years. However, in recent times data has shown that the incidence of myocardial infarction among young adults is believed to be on the rise [4] . Acute STEMI is a medical emergency that requires urgent reperfusion strategy by using thrombolytic drugs or PCI. Our patient presented with an acute coronary syndrome that rapidly progressed to STEMI. Several studies have concluded that STEMI is the most common presentation of acute coronary syndrome in young adults [5] compared to old people in whom unstable angina and NSTEMI are the commonest presentations. In a prospective study conducted in Senegal on acute coronary syndrome in young Africans, Sarr et al found STEMI in 85.7% of cases and NSTEMI was only recorded in 14.3% of candidates [6] . There is enough evidence to support the fact that majority of young adults with myocardial infarction have single vessel disease and the left anterior descendant artery is the most affected [7] ; though our patient’s coronary angiography revealed a single vessel disease with 90% stenosis of the dominant right coronary artery.
Impaired lipid metabolism is one of the major factors that significantly contribute to premature cardiovascular disease. However, lipid control with statins has not been adequate in reducing the risk of cardiovascular diseases [8] . Several studies have identified an elevated lipoprotein (a) as an independent cardiovascular disease risk factor for coronary artery disease in the absence of traditional risk factors [9-10] .
Lipoprotein (a) is genetically determined and is structural homologous with plasminogen fibrin binding domain; hence competing with plasminogen activity and increasing cardiovascular risk by causing a pro-coagulant state. Lipoprotein (a) also causes inflammatory reactions, endothelial dysfunction and oxidative stress which further increases the risk of cardiovascular events. Therefore, lowering lipoprotein (a) could potentially reduce the risk of cardiovascular diseases; though, only limited evidence supports this hypothesis because no clinical trials have adequately tested the hypothesis that lowering serum lipoprotein (a) reduces the incidence of future atherosclerotic cardiovascular events [11] . In our case report, the patient had elevated serum lipoprotein (a) levels nearly three times the normal range (137mg/dl), his BMI was 25.9 and he had no other identifiable risk factors. This case is similar to another case that was reported in Japan of a male, 23years old who survived a total occlusion of the left coronary artery main trunk and was found with a lipoprotein (a) level of 74mg/dl but had normal triglycerides, LDL and HDL cholesterol [12] .
Our case is peculiar though, because the cardiovascular event in our patient happened in a young person with a background 10-year history of chest pain, who then suffered plaque rupture and an acute MI probably triggered by SARS COV2 inflammation, then was found with an elevated serum lipoprotein (a) level. This is the strength of this case report as it highlights this unique presentation in our patient. Most literature agrees on the fact that acute coronary syndrome will increase with the COVID-19 pandemic due to inflammatory responses and especially cytokine storm associated with SARS COV-2 infection [13] and most acute coronary events have most occurred in acutely ill COVID patients with respiratory failure; thrombotic coronary events in asymptomatic recovering patients is not well described. Our patient was in his second month post COVID pneumonia and probably had on-going inflammation as was typical in most post COVID patients with long COVID syndrome, hence the plaque rupture.
Despite receiving high dose Niacin and statins, our patient still has persistently elevated serum lipoprotein (a) levels and has no access to PCSK9 receptor blockers which are unavailable in our resource-limited setting. This is the weakness of this case because the patient remains at risk of developing CAD in the other coronary vessels that were not previously affected because the prevention requires lowering his lipoprotein (a) levels with PCSK9 receptor blockers which the patient cannot afford as it has to be sourced abroad and very expensive.
However, the patient says they were fortunate that a correct diagnosis was made timely warranting an immediate intervention which prevented them from getting consequences of untreated myocardial infarction when they first presented to our facility. He does his regularly activities normally and has not experienced any chest pains since then.
CONCLUSION
Elevated lipoprotein (a) appears to be an important factor for premature coronary artery disease and must be considered in young patients presenting with acute coronary syndromes in the absence of traditional cardiovascular risk factors. The 2019 European Society of Cardiology guidelines on management of dyslipidaemia recommend a once in a lifetime test for Lp (a) levels [14] . This underscores the importance of having a baseline lipoprotein (a) level for everyone to identify individuals among the young population that could be at risk of presenting with PCAD.
LIST OF ABBREVIATIONS
ACS------Acute Coronary Syndromes
BMI------Body Mass Index
CAD------Coronary artery disease
DES------Drug eluting stent
EF-------Ejection fraction
HDL------High density lipoprotein
HIV------Human Immunodeficiency Virus
LDL------Low density lipoprotein
MI-------Myocardial infarction
NSTEMI----Non-ST elevation myocardial infarction
PCI-------Percutaneous coronary interventio
PCSK9-----Pro-protein convertase subtilisin/kexin type 9
RCA-------Right coronary artery
STEMI-----ST elevation myocardial infarction
REFERENECES
- Shah N, Kelly AM, Cox N, Wong C, Soon K. Myocardial Infarction in the ‘’young’’: Risk Factors, Presentation, Management and Prognosis. Heart Lung Circ. 2016 Oct; 25(10):955-60.
- Aram J. Mirza, Abdulsalam Y.Taha, Bahar R. Khdhir. Risk factors for acute coronary syndrome in patients below the age of 40 years. The Egyptian Heart Journal. 2018 December; 70 (4).
- Kannel WB, Abbot RD. Incidence and prognosis of unrecognized myocardial infarction. An update on the Framingham study. N Engl J Med 1984; 311:1144.
- Yang et al. Risk factors and outcomes of very young adults who experience myocardial infarction: The Partners YOUNG-MI Registry. Am J Med. 2020 May; 133(5): 605–612.e1.
- Ekou A, Yao H, Kouamé I, Boni RY, Ehouman E, N'Guetta R. Primary PCI in the management of STEMI in sub-Saharan Africa: insights from Abidjan Heart Institute catheterisation laboratory. Cardiovasc J Afr. 2020 Jul/Aug; 31(4):201-204.
- Moustapha Sarr, Djibril Mari Ba, and Serigne Abou Ba. Acute Coronary Syndrome in Young Sub-Saharan Africans: A prospective Study of 21 cases. BMC Cardiovascular Disord. 2013; 13:118.
- Sinha SK, Krishna V, Thakur R, Kumar A, Mishra r, Asif M, Afdaali N, Mohan varma C. Acute Myocardial infarction in very young Adults: A clinical presentation, Risk factors, hospital outcome index, and their angiographic characteristics in north India-AMIYA Study. ARYA Atheroscler. 2017 Mar; 13(2): 79-87.
- Pradhan AD, Paynter NP, Everett BM, Glynn RJ, Amarenco P, Elam M, Ginsberg H, Hiatt WR, Ishibashi S, Koenig W, Nordestgaard BG, Fruchart JC, Libby P, Ridker PM. Rationale and design of the Pemafibrate to reduce cardiovascular outcomes by reducing triglycerides in patients with diabetes (PROMINENT) study. Am Heart J. 2018 Dec; 206:80-93.
- Gudbjartsson DF et al. Lipoprotein (a) Concentration and Risks of cardiovascular Disease and Diabetes. J Am Coll Cardiol.2019 Dec 17; 74(24):2982-2994.
- Miksenas H, Januzzi JL Jr, Natarajan P. Lipoprotein (a) and cardiovascular Diseases. JAMA.2021 Jul 27; 326(4):352-353.
- Rhainds, D., Brodeur, M.R. & Tardif, JC. Lipoprotein (a): When to measure and how to treat? Curr Atheroscler Rep 23, 51 2021.
- Hiroaki Hiraiwa, MD, Ryota Morimoto, MD, PhD, and Toyoaki Murohara, MD, PhD, FJCC. A survival case of a young adult patient with ST-elevated myocardial infarction with high levels of lipoprotein (a). J Cardiol Cases. 2019 Jun; 19(6): 207-210.
- Ahmad Jabri, MD; Ankur Kalra, MD; Ashish Kumar, MBBS; et al. Incidence of Stress Cardiomyopathy During the Coronavirus Disease 2019 Pandemic. JAMA Netw Open. 2020; 3(7).
- https://www.escardio.org/static- file/Escardio/Guidelines/publications/DYSLIPguidelines-dyslipidemias-FT.pdf
APPENDIX
Medical Journal of Zambia, Vol 50, 3
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.