Incidental Finding of Posterior Urethral Valve During Routine Antenatal.
Ultrasound: Diagnostic Imaging Case Report in Botswana.
Cuthbert Mulenga
Ghanzi Primary Hospital, Ghanzi District, Botswana.
Osward Bwanga
Midland University Hospital Tullamore, Radiology Department, Co. Offaly, Ireland
Thabo A. Moloi
Princess Marina Hospital, Department of Obstetrics and Gynaecology, Gaborone, Botswana.
DOI: https://doi.org/10.55320/mjz.49.3.369
Keywords: Anhydromnios, Antenatal ultrasound, Hydroureteronephrosis, Posterior urethral valve (PUV).
ABSTRACT
Medical ultrasound is a particularly useful imaging method used in the diagnosis of urinary foetal anomalies. One such foetal anomaly is the posterior urethral valve (PUV), which is a congenital malformation of the male urethra occurring early in gestation life. PUV is a common cause of obstructive uropathy in males and foetal death during pregnancy. We report from a medical imaging perspective on a rare and high-risk case of a PUV detected during routine antenatal ultrasound imaging in Botswana. The first scan performed at 16 weeks of gestation age was unremarkable. However, subsequent antenatal ultrasound scans at and after 20 weeks demonstrated bilateral hydronephrosis, distended ureters, and a urinary bladder which gradually increased with the gestation age. There was also a corresponding reduction in amniotic fluid and foetal movements. As a result of these complications, the pregnancy was classified as a “high-risk.” At 30 weeks, spontaneous labour occurred and a fresh still birth was delivered.
INTRODUCTION
Medical ultrasound plays an important role in the diagnosis of congenital urinary anomalies during foetal development. One of the foetal anomalies is the posterior urethral valve (PUV). Kilciler et al.[1] define a posterior urethral valve as a congenital malformation of the male urethra occurring early in gestation life. It is the most common cause of congenital bladder outlet obstruction and its responsible for about 17% of paediatric end-stage kidney disease.[2-3] This condition is present in males with an incidence in the range of 1:5000 to 1:8000 live births.[3-4] In severe cases of near-complete or complete obstruction during foetal development, death may result due to oligohydramnios, foetal renal failure, and pulmonary hypoplasia.[4-5] However, those who survive after birth suffer ongoing bladder dysfunction and progressive kidney injury resulting from early childhood.[2,4,6,7] These complications can be minimized with early diagnosis and appropriate management of the patient in specialised hospitals.
Since its inception in the early 1970s, standard 2D ultrasound has been a cornerstone of prenatal diagnosis of foetal malformations.3[3,4,8,9] Despite the modern advances in medical imaging technologies, such as 3D ultrasonography, and magnetic resonance imaging (MRI), they have contributed less to the current knowledge than 2D ultrasound.[10] Standard 2D ultrasound remains the main medical imaging method in the diagnosis of foetal anomalies.
In Botswana, the 2010 guidelines for antenatal care and management of obstetrics are used to manage pregnant women.[11] These guidelines stipulate that a pregnant woman should attend at least three antenatal visits during the first, second and third trimesters. This allows monitoring of the health of both the foetus and the mother by healthcare professionals that include midwives, obstetricians, and sonographers. The monitoring includes the early identification of foetal abnormalities and the initiation of relevant interventions.
To the best knowledge of the authors, this is the first case report on PUV to be documented from imaging’s perceptive in Botswana. At the time of this report, there has never been any known published cases on PUV from an imaging perspective. Most of the cases reported in the international literature on this topic are from medical professionals.[1,6,7,12] We, therefore, report a rare diagnostic imaging case of PUV detected during a routine antenatal ultrasound in Botswana.
CASE PRESENTATION
A 22-year-old pregnant African ethnicity woman (gravida 3 para 2) presented in her fifth month to the outpatient department (OPD) for antenatal services in March 2021. By her dates, she was 20 weeks pregnant. As per procedure, she was referred to our imaging department by the attending obstetrician for her second-trimester prenatal ultrasound scan. An ALOKA 350 plus ultrasound machine with a 2.5-5.0 MHz transabdominal transducer was used to assess the pregnancy throughout this diagnostic imaging case report.
First ultrasound scan
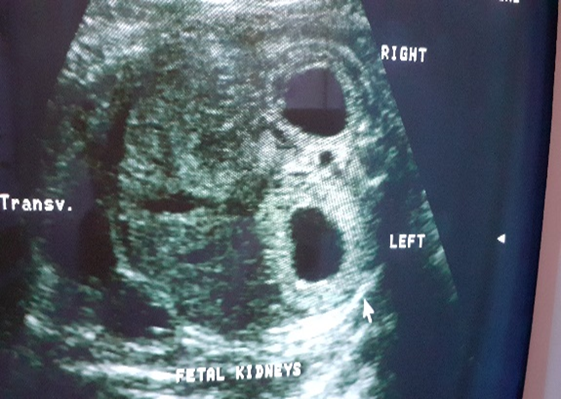
The first prenatal routine ultrasound at 16 weeks was unremarkable, and showed normal foetal kidneys, bladder, and adequate amniotic fluid volume (Figure 1). As per ultrasound guidelines, a second-trimester foetal anomaly scan was arranged at 20 weeks gestation age.
Second ultrasound scan
The second ultrasound revealed a male live foetus of 20 weeks gestation age, with bilateral hydronephrosis, distended urinary bladder, and significant oligohydramnios (Figure 2a). Figure 2b shows male foetal genitalia demonstrated during ultrasound scans. With the abnormal sonographic findings, a follow-up rescan at 24 weeks was arranged to assess the foetal urinary system.


On enquiry, her previous pregnancies were not associated with any foetal-maternal complications. The woman had no medical or surgical problem and there was no family history of chromosomal, congenital, or growth anomaly. She was generally in good health.
Third ultrasound scan
A follow-up rescans at 24 weeks gestation age revealed grossly distended urinary bladder, bilateral hydroureteronephrosis, and anhydramnios with reduced foetal movement (Figure 3).

At this point, the sonographic findings raised a strong suspicion of PUV obstruction. The woman was counselled by the midwife and the attending obstetrician regarding the possible poor prognosis. The attending obstetrician discussed the foetal scan findings with the sonographer and follow-up rescan at 27 weeks was arranged to monitor the foetal wellbeing.
Fourth ultrasound scan
The follow-up rescan was performed at 27 weeks and revealed a live foetus in breech presentation, reduced hydronephrosis compared to the previous scan, grossly over distended urinary bladder with generalized wall thickening (Figure 4), and anhydramnios.

The neonatal specialist based at the referral hospital was informed and advised close monitoring with possible admission as a case of congenital PUV with poor prognosis. The woman was admitted and informed of the available clinical optional intervention of medical termination of the pregnancy, as newer modern interventions to improve the prognosis are not available in the country. Foetal growth continued on the 50th percentile with grossly reduced amniotic fluid volume. From this time, the pregnancy was managed as “high risk” and the woman was informed by the attending obstetrician of the possible medical termination or adverse pregnancy outcome.
Fifth ultrasound scan
An ultrasound scan follow-up a fortnight later was performed which continued to show anhydramios, bilateral hydroureteronephrosis, over distended urinary bladder with a “keyhole sign” (Figure 6a) and reduced foetal movement. Both kidneys showed increased cortical echogenicity, with the fullness of the central pelvis (Figure 6b).

Given the persistent sonographic findings of anhydramios, over distended urinary bladder, and bilateral hydroureteronephrosis with its associated foetal complications, the mother received continued support and counselling by the obstetrician. Due to multiple organ involvement, and continued poor prognosis, she was informed and advised to opt for a medical termination of the pregnancy which she declined.
The outcome of the pregnancy
At 30 weeks of gestation age, a spontaneous labour occurred, and a fresh still birth was delivered with a foetal weight of 1900g and length of 43.1cm. The imaging department was informed of the outcome and immediately the whole-body plain X-ray often called ‘Baby-gram’ was requested by the obstetrician and performed to check for any missed possible skeletal abnormalities on prenatal ultrasound scans which appeared normal (Figure 7).

A thorough physical examination was done by the obstetrician on the foetus which showed a moderately distended urinary bladder. The male external genitalia were normally developed; a fine cannula could be passed through the foetal urethral meatus but could not be passed into the urinary bladder due to an obstruction at the level of the urethral vesical junction. The physical assessment and all sonographic findings proved this case as of PUV.
DISCUSSION
In this case report, medical ultrasound was used as the first-line imaging modality to diagnose PUV. Unlike plain film X-rays, ultrasound imaging is free of ionising radiation, and is regarded as the safest diagnostic tool for pregnant women.[9-13] The World Health Organization (WHO)[8] recommends three antenatal ultrasound scans during pregnancy. The first scan at 8-12 weeks to confirm intrauterine pregnancy, the number of foetuses, gestation age, and early detection of abnormal pregnancy; the second scan at 16-20 weeks to assess for any foetal anomalies; the third scan at 32 weeks onwards to determine foetal presentation, placental location, estimation of foetal weight (EFW) and general foetal wellbeing. However, ultrasound is highly operator dependent.[13] This means that to have a correct diagnosis, the sonographer should be appropriately trained and experienced. For this reason, the World Health Organization (WHO)[9] recommends that antenatal ultrasounds be performed by a competent person to enable detection of any pregnancy complications and facilitate timely and appropriate management. However, there is an acute scarcity of sonographers in Botswana. This can be attributed due to the non-availability of a training institution offering medical imaging courses, such as radiography and ultrasound.
Antenatal ultrasound plays an important role in the identification of foetal gender. This is of great importance in the management of pregnancy in families at increased risk of sex inherited diseases and diagnosis of foetal abnormalities such as PUV.[13-14] This is best performed in the second trimester of pregnancy when the external genitalia are well developed and visualized, and the foetus can freely move in the amniotic fluid.[14] The gender diagnosis is made by visualization of the external genitalia: a boy is diagnosed if the sonographer sees the penis and scrotum and a girl the labia. Literature reports that PUV occurs exclusively in males due to the complex development of a male genital urinary system which occurs between the fourth and fifth week of embryogenic life.[5,6,7] This was as in our case where male foetal genitalia was confirmed by ultrasound at 20 weeks of gestation age (Figure 2b). In the context of the case under discussion, the sonographic finding of a male was the first feature which narrowed the diagnosis to PUV.
One of the complications of PUV is obstruction of the urinary tract affecting the kidneys, ureters, and urinary bladder. In this case report, there was bilateral hydroureteronephrosis and a grossly thick-walled distended urinary bladder which resembled a keyhole (Figure 6a). In ultrasound, this is referred as a “Keyhole sign”. The obstruction of the foetal urethra resulted in the build-up of urine in the kidneys and ureters (hydroureteronephrosis) and over-distension of the urinary bladder. This sonographic finding agrees with what is reported in the literature regarding PUV.[4,,6,7] If no intervention is done, this may result in damage to the foetal kidneys, which may be ascertained sonographically as abnormal increased renal cortical echogenicity (Figure 6b).[7] This second sonographic feature of an obstructed urinary tract narrowed the diagnosis to that of the PUV case.
During pregnancy, the amniotic fluid provides necessary fluid, space, and growth factors to allow normal development and growth of foetal organs such as lungs.[15-16] In this case, there was a significant reduction in amniotic fluid volume as the pregnancy progressed. Suliburska et al.[15] add that foetal urination is the main mechanism contributing to the amniotic fluid volume and its essential role in the normal development and maturation of the lungs. Its persistent deficiency may result in lung hypoplasia, which is the incomplete development of parts of the lungs.[16] Because of the gross oligohydramnios at 30 weeks, there was significantly reduced foetal movement. Ultrasound also revealed increased abnormal renal echogenicity which is consistent with foetal renal failure which has a high prenatal morbidity and mortality rate.[17] This third sonographic finding of oligohydramnios added to the evidence of a case of PUV.
Literature reports that PUV is associated with skeletal abnormalities such as craniospinal defects and poor bone growth.[7-12] To rule out skeletal abnormalities which could have been missed during an antenatal ultrasound, a ‘babygram ’was performed on the foetus. An anterior-posterior view of the whole body was imaged as recommended in the radiography literature.[18] The “babygram” revealed no evidence of associated skeletal abnormalities (Figure 8).
CONCLUSION
PUV is a rare congenital malformation affecting the urinary system in males. Medical ultrasound is regarded as the first-line imaging modality used to diagnose this foetal anomaly. This imaging case report demonstrates that prenatal diagnosis requires follow-up serial ultrasound scans which play an important role in the assessment and progression of the complications that come with the pregnancy. It is highly recommended to have a minimum of three prenatal ultrasound scans: in the first, second, and third trimesters. However, there is a scarcity of sonographers in Botswana to cover a comprehensive ultrasound service. To improve the quality of antenatal services, it is recommended to train or recruit more sonographers.
CONSENT
Consent was obtained from the patient to use the information from her scan results. Permission was also sought and granted by our hospital management to have access to the patient’s information and use sonographic and X-ray images in this publication [Ref: GDHMT; 4/7/6 I].
REFERENCES
- Kilciler M, Basal S, Irkilata HC, Zor M, Okan M, Dayanc M. Adult posterior urethral valve: a case report. GMS German Medical Science. 2010; 8: 1-3.
- Hodges SJ, Patel B, McLorie G, Atala A. Posterior urethral valves. Scientific World Journal. 2009; 9:1119-1126.
- Talabi AO, Sowande OA, Etonyeaku AC, Salako AA, Adejuyigbe O. Posterior urethral valves in children: pattern of presentation and outcome of initial treatment in Ile-Ife, Nigeria. Niger J Surg Off Publ Niger Surg Res Soc. 2015;21(2):151-156.
- Tambo FFM, Tolefac PN, Ngowe MN, Minkande JZ, Guemkam G, Telelen NA. et al. Posterior urethral valves: 10 years audit of epidemiologic, diagnostic and therapeutic aspects in Yaoundé gynaeco-obstetric and paediatric hospital. BMC Urol. 2018; 18 (46):1-7.
- Rowell AC, Sangster GP, Caraway JD, Walker PW, Elmajian DA, Heldmann MG. Genitourinary imaging: part 1, congenital urinary anomalies and their management. AJR Am J Roentgenol. 2012; 199(5):545-553.
- Bureau M, Bolduc S. Allantoic cysts and posterior urethral valves: a case report. Ultrasound Obstet Gynecol. 2011 Jul;38(1):116-118.
- Sharma A, Agarwal S, Aggarwal A, Sankhwar S. Posterior urethral valve associated with a foreign body in posterior urethra: a first of its kind report. BMJ Case Rep. 2018 Sep 23;2018: bcr2018226257.
- World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. World Health Organization; 2016.
- Ehrlich RA, Coakes DM. Patient care in radiography: with an introduction to medical imaging. 10th ed. London: Elsevier; 2020.
- Benacerraf BR, Benson CB, Abuhamad AZ, Copel JA, Abramowicz JS, Devore GR, et al. Three- and 4-dimensional ultrasound in obstetrics and gynecology: proceedings of the American Institute of Ultrasound in Medicine Consensus Conference. J Ultrasound Med. 2005;24 (12):1587-1597.
- Ministry of Health. Guidelines for antenatal care and management of obstetrics emergence n prevention of mother to child transmission on HIV. Gaborone: Ministry of Health; 2010.
- Pradhan M, Singh N, Singh AK, Kumari N. Rare association of fetal posterior urethral valve with ureteric stricture. J Prenat Med. 2012;6(1):1-3.
- Bwanga O, Mwase G, Kaunda HC. Midwives’ experiences of performing obstetric ultrasounds in maternity care: a systematic review. African Journal of Midwifery and Women’s Health. 2021; 15(2): 1-8.
- Gharekhanloo F. The ultrasound identification of fetal gender at the gestational age of 11-12 weeks. J Family Med Prim Care. 2018;7(1): 210-212.
- Suliburska J, Kocyłowski R, Komorowicz I, Grzesiak M, Bogdański P, Barałkiewicz D. Concentrations of mineral in amniotic fluid and their relations to selected maternal and fetal parameters. Biol Trace Elem Res. 2016;172(1): 37-45.
- lasberg T, Jackson P, Pavlova Z, Nair S. Infant with clinical evidence of pulmonary hypoplasia: a case report. Cureus. 2017;9(5): e1298.
- Roth KS, Carter WH Jr, Chan JC. Obstructive nephropathy in children: long-term progression after relief of posterior urethral valve. Pediatrics. 2001;107(5):1004-1010.
- Whitley AS, Jefferson G, Sloane KHC, Anderson G, Hoadley G. Clark’s positioning in radiography. 13th ed. London: CRC Press Ltd; 2015.
Medical Journal of Zambia, Vol 49, 3
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.