An 86-Year-Old Male with Metastasized Cancer Treated with External Beam Radiation Therapy: A Case Report from Zimbabwe
Eucaria Mushosho
School of Allied Health Sciences, Harare Institute of Technology
Gracious Motsi
School of Allied Health Sciences, Harare Institute of Technology
Fadzai Musiwarwo
School of Allied Health Sciences, Harare Institute of Technology
Bornface Chinene
School of Allied Health Sciences, Harare Institute of Technology
DOI: https://doi.org/10.55320/mjz.49.3.367
Keywords:Prostate cancer, external beam radiotherapy, hormone therapy
ABSTRACT
Prostate cancer is the most common malignancy diagnosed in men and the second most common cause of cancer deaths in men. Incidence increases drastically after the age of 50, however, it is more common in males above the age of 65. Prostatic cancer is asymptomatic in its early stages, i.e., when it is still localized, hence most patients present with late-stage cancers. Patients with late-stage prostate cancer usually present with urethral obstruction, nocturia, narrow stream, and they rarely present with pain or stiffness caused by bony metastases. The common treatment for late-stage prostate cancer is hormonal therapy. We herein present a case of an 86-year-old male who presented with metastasized prostate cancer. The cancer had metastasized to the head of the femur and there was bone fracture in the neck of the femur as well. The patient received external beam radiotherapy as palliative treatment due to the limited resources in Zimbabwe. The patient did not come for follow up review and hence it was not possible to conclude whether the external beam treatment was an effective palliative treatment. The learning points in this case are as follows: stage at presentation of man with cancer of the prostate in comparison with what literature say, management done in comparison to the recommended management guidelines, follow up strategies to minimize patients absconding follow up reviews and how loss of follow up to patients treated affect future evidence-based management of patients.
INTRODUCTION
Prostate cancer (PCa) is a disease whereby malignant cells develop in the prostate, a gland in the male reproductive system. This malignancy is the most commonly diagnosed cancer in men and the second most common cause of cancer deaths in men[1]. African American men are twice as likely than men of any other racial or ethnic group to be diagnosed with PCa and to die of the malignancy[2] . Estimated new cases globally in 2020 were 1 414 259 which is 7.3 % of all cancers and there were 375 304 deaths constituting 3.8% of all cancer deaths[3] . Global incidence rates for PCa vary from 6.3% to 83.4% with highest age standardized incidence rates being recorded in Northern Europe and lowest in South Central Asia. Prostate cancer is the most commonly diagnosed cancer among men of African origin and has the leading mortality rates, with highest rates being recorded in East Africa and the West African countries[4] . The same author however argues that data collection and Prostate Specific Antigen testing are minimal in the African continent which severely affect the reliability and statistical analysis of data. Major worrying presenting patterns of PCa in Africa is that majority of the new cases are diagnosed at advanced stages with metastasis and poor prognosis resulting in low chances of long-term survival. In Zimbabwe PCa is the second most common cancer after cervical cancer, and is the leading malignancy among black men contributing 22.5% of male cancers [5] .
CASE PRESENTATION
An 86-year-old male presented to the radiation oncology department with pathological fracture of the left femur in March 2018. The patient was referred by orthopaedic surgeons following hemiarthroplasty at a hospital in Zimbabwe which was done six months prior for pathological fracture of the left neck of the femur. The left femoral head was taken for histological evaluation and was seen to be an invasive well differentiated adenocarcinoma. The patient had no history of urinary symptoms. A PSA test done in April 2018 was elevated at 11ng/mL. The conclusion was that the primary tumour was prostate cancer and the pathological fracture was due to bone metastasis. However, there was no documentation of prostate biopsy.
Medical history revealed that the patient was HIV positive and on tenolam for the previous year. Upon evaluation at the oncology centre, the patient had no weight loss, fever or night sweats. The patient developed deep vein thrombosis post operatively. Familial history revealed that the patient was staying in a high-density suburb of Harare, the capital city of Zimbabwe, with two children of his seven children. It was reported that his wife was late but cause of death was not recorded. The patient had no history of tuberculosis, tobacco smoking or alcohol use. The patient needed assistance with most activities of daily living.
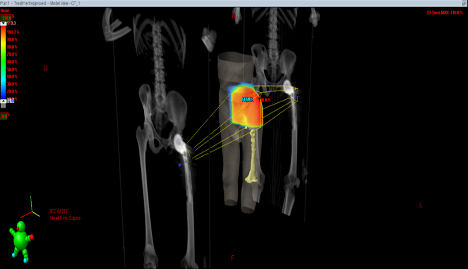
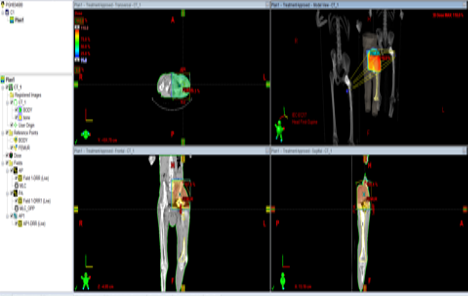
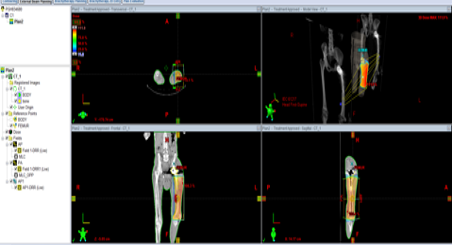
Femoral head biopsy and PSA test were done and the cancer was staged as advanced prostate cancer TxNxM1 (Stage IV), with metastasis to the bone, particularly left femoral head and the left femur. The examining oncologists planned the following for diagnosis and treatment; laboratory tests including full blood count, liver function tests, urea and electrolytes as well as a PSA test. Chest x-ray, and Ultrasound of the abdomen and pelvis were also prescribed. The patient was given zoledronic acid as bisphosphonate therapy, morphine to manage his pain as well as bisacodyl, celecoxib, and dexamethasone. Patient received palliative radiation therapy in the left pelvis for the femoral head as well as to the left femur, which had been prescribed as 20Gy given in five fractions over five days, using parallel opposed field technique.
The patient responded well to the treatment as he reported less pain. However, the patient did not come back for review, and there was no record of follow-up which was done.
DISCUSSION
The patient in this case presented with advanced PCa which had metastasized to the bone. About 80% of the time prostate cancer cells metastasize to the bone which include the spine, femur and the pelvic bones[6] . As the malignancy spreads to distal organs, it develops more complications such as bone pain, pathological fracture and spinal cord compression. The 86-year presented with a fractured neck of femur. This is in line with the argument that, autopsies have revealed that 80% of advanced PCa is accompanied by the development of skeletal metastases [7] . Patients with advanced disease present with pain or stiffness that would have been caused by bony metastases [8] . Common complications caused by bone metastases include bone pain, pathological fracture and spinal cord compression
The primary disease was not treated since patient presented late with bone metastasis which is a common finding in African man. Late presentation could be due to a number of factors. This could be due to the asymptomatic nature of PCa as stated by Giona [4] . In most cases PCa may not cause symptoms at all but the recorded symptoms are frequent urination, weak or interrupted urine flow, blood in urine, nocturia, dysuria, new onset of erectile dysfunction, pain in pelvis, spine, shoulders and ribs, unexplained weight loss, lymphedema and renal insufficiency[8] . In this case the patient did not present with any of the symptoms above except for bone pain which was due to a pathological fracture. On presentation PSA test were used to stage the malignancy which was staged as Advanced prostate cancer stage IV. Most carcinomas of the prostate are found because of elevated PSA level while the tumour is not palpable in most patients[9] . Depending on the histologic grade (Gleason score) and pre-treatment PSA, extracapsular extension is currently detected in less than 10% of patients on rectal digital examination. Palpable tumours are noted in approximately 30% to 40% of patients . In the case in question the PSA test was done after the pathological fracture and was used to stage the disease.
It is possible that the patient could have been attempting other treatment alternatives such as traditional medicines which is normal practice for most people in Zimbabwe[10] . In Zimbabwe there is a three-tier healthcare system which consists of traditional healers, spiritual healers and the health sector. It has been shown that the health sector is a last resort for many patients in Zimbabwe after the traditional healers and spiritual healers would have failed. By the time patients seek medical care, the cancer would have already advanced, and in this case metastasized[11]. While the argument is not that patients should not try other means of treatment besides the formal health management, it is important that the three types of treatment adopted in Zimbabwe be integrated so that there is a seamless referral system for the traditional and /or spiritual to the formal medical system. This helps in continuity of management. Also, clear guidelines should be followed such that the integration of the three methods of patient management do not result in poor patient management.
The patient in this case was 86 years’ old which agrees with prostate cancer presentation patterns where prostate cancer is more common in older patients and also more aggressive with progressive age[12] . Being an elderly may have contributed towards presenting early since it was indicated in the patient history that patient needed to be assisted by others most of the time.
Men are less likely to seek health care compared to women and when they do, they present with late stage disease, hence the patient in this case sought medical help too late which also affect the prognosis of the disease. Prostate cancer screening is not as common as other cancers such as breast cancer, as there has not been any focused screening policy or strategy in Sub-Saharan Africa[13] . which also includes Zimbabwe. Lack of screening protocols associated with asymptomatic properties of early stages of cancer of the prostate means most Zimbabwean men present with late and advanced PCa. Lack of knowledge of the disease could have contributed to late presentation. This is supported by a study carried out by Moyo,[14] on men’s knowledge about PCa in Zimbabwe. The findings of the study were that even if prostate cancer is the most common cancer affecting men in Zimbabwe, men’s awareness of the disease and comprehensive knowledge about the signs and symptoms, screening methods and the age groups predisposed to the risk of the disease have remained poorly understood.
The patient in question was HIV positive and on treatment, but HIV is not considered a risk factor for prostate cancer. Causes of PCa are not known, but the main risk factors include obesity, age, family history, lower levels of Vitamin D, prostatitis and elevated blood levels of testosterone. The strongest risk factor for the disease, excluding advanced age, is a family history of cancer of the prostate[15] . suggesting the importance of genetic factors in disease development. Genome-wide association studies have identified more than 70 susceptibility loci associated with modest relative risks of prostate cancer, which, when taken together, explain approximately 30% of the familial prostate cancer risk, with BRCA1/2 mutations conferring a more aggressive prostate cancer phenotype with a higher probability of nodal involvement and distant metastasis [16] .
The main technique used to treat the patient was palliative external beam radiotherapy to treat the pathological fracture due to metastases to the bone on the left femur. Treatment methods for patients with bone metastases are mostly palliative and include hormonal therapy, chemotherapy, pharmacological management, radiotherapy for pain and spinal cord compressions, surgical fixation for pathological fractures, and decompression for spinal cord, and the use of bisphosphonates to inhibit osteoclast activity[17] . Radiotherapy remains the mainstay of treatment for pelvic disease control and encouraging results have been reported with androgen ablation as adjuvant therapy [18] .
The American Cancer Society,[9] states that local radiotherapy may be useful for perineal pain, bleeding, or bony pain. It may be offered postoperatively, or as an alternative if the patient is unfit for surgical intervention. A single fraction of local radiotherapy is effective for pain relief in symptomatic bony metastases in up to 76% of patients[8] . It may, however, take several weeks before its effect manifest. In cases where a large treatment field is required, hemibody irradiation is utilized, usually encompassing pelvis and the upper femurs, this frequently results in diarrhoea and nausea. The treatment techniques adopted for the case were two parallel opposed adjacent fields with no separation to avoid an overlap because it was just palliative, treating the pelvis and head of femur and the femoral field[19] .
The standard of care for treating metastatic PCa is hormonal therapy. This type of treatment is aimed at lowering the production of testosterone and other male hormones. Testosterone acts like a fuel that encourages PCa to grow. Without testosterone and other male hormones, PCa goes into remission, often for many years[9] . Androgens are crucial for proliferation, differentiation, and spread of prostate cancer cells [20] . Androgen deprivation results in an initial programmed cell death (apoptosis) in both normal and malignant prostate cells. The goal of systemic androgen deprivation therapy (ADT) for prostate cancer is to suppress testosterone to castrate levels. In the case presented above, the patient did not receive any form of hormonal therapy because androgen deprivation therapy is not commonly used in many developing countries, especially in Zimbabwe due to its unavailability and its high cost. According to Cassel et al., (2019)[21] the most common treatment of advanced prostate cancer in Africa is surgical castration, as most modern treatment options such as hormonal therapy are unavailable or unaffordable.
The patient in this case received zoledronic acid as bisphosphonate therapy. Bone complications in prostate cancer can occur as a result of skeletal metastases, long term treatment with androgen withdrawal or following external beam radiotherapy. Bisphosphonates, which are now widely used in breast cancer treatment, have been shown to reduce bony pain in prostatic cancer for 2–3 weeks after a single intravenous infusion, in up to 30% of patients[22] . Bisphosphonates act by decreasing the rate of bone turnover, reducing the number of osteoclasts, their recruitment, lifespan and activity.
A combination of hormonal therapy and external beam radiotherapy could have been beneficial to the patient. A study by Rusthoven, et al.,18 sought to evaluate the use of local therapies such as external beam radiotherapy for the treatment of metastatic prostate cancer together with androgen deprivation therapy. In the study, the National Cancer Database (NCDB) was used to evaluate the overall survival of men with metastatic prostate cancer treated with ADT with and without prostate external beam radiotherapy. The study showed that men with metastatic cancer receiving prostate external beam radiotherapy and ADT lived substantially longer than those treated with ADT alone [18] .
Besides hormone therapy and radiotherapy other treatment protocols that could have been used to manage the patient include chemo-hormonal therapy. In chemo-hormonal therapy, large clinical trials have recently demonstrated benefits of early initiation of chemotherapy concomitantly with ADT. As evidenced in the trial study by Sweeney, et al., [23] and James & Sydes[24] patients with high volume, newly diagnosed or recurrent hormone therapy naïve metastatic prostate cancer having adequate prostate and organ function should be considered for chemo-hormonal therapy. This is widely accepted as the new standard of care therapy for these patients.
CONCLUSION
There is need for increase in awareness campaigns and education for prostate cancer to avoid patients presenting with advanced cancers. While hormone therapy is effective in the management of late stage prostate cancer, in this case it was not taken as an option probably due to cost, creating a gap in the management of the patient which could result in poor prognosis.
ETHICAL CONSIDERATIONS
Permission to access patient information was obtained from the chief radiographer at the oncology centre where the patient was treated. No approval was required from the Medical Research Council of Zimbabwe since the names and initials of the patient that lead to patient identification were not used. Patient confidentiality was observed, and there was no harm or unnecessary radiation exposure to the patient. After obtaining permission from the department an ethical clearance certificate from the department of Radiography was obtained [certificate number 2021/01D].
AUTHOR CONTRIBUTIONS
G. Motsi was responsible for case identification and initial write up. F.Musiwarwo retrieved the plan and write up on recommended treatment protocols. E.Y.Mushosho supervised the case and realigned it for publication. B. Chinene did plagiarism checks, editing and formatting of the paper.
REFERENCES
- Schatten H. Brief Overview of Prostate Cancer Statistics, Grading, Diagnosis and Treatment Strategies. Adv Exp Med Biol. 2018;1095:1-14. doi: 10.1007/978-3-319-95693-0_1. PMID: 30229546.
- PDQ Adult Treatment Editorial Board. Prostate Cancer Treatment (PDQ®): Health Professional Version. 2022 Oct 14. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002–. PMID: 26389471.
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021 May;71(3):209-249. doi: 10.3322/caac.21660. Epub 2021 Feb 4. PMID: 33538338.
- Giona S. The Epidemiology of Prostate Cancer. In: Bott SRJ, Ng KL, editors. Prostate Cancer [Internet]. Brisbane (AU): Exon Publications; 2021 May 27. Chapter 1. PMID: 34181376.
- Musarurwa, P., Juru, T. & Bara, H. Prostate cancer in Harare City, Zimbabwe: Trends in incidence, mortality and epidemiological characteristics, 2006-2015, Harare: Tephinet Task Force; 2016.
- Michael J. Morris, (2019), on Metastatic Prostate Cancer: Adding Abiraterone Acetate to Enzalutamide; ASCO meeting, www.ascopost.com Last visited 3/04/2022.
- Wong SK, Mohamad NV, Giaze TR, Chin KY, Mohamed N, Ima-Nirwana S. Prostate Cancer and Bone Metastases: The Underlying Mechanisms. Int J Mol Sci. 2019 May 27;20(10):2587. doi: 10.3390/ijms20102587. PMID: 31137764; PMCID: PMC6567184.
- Cancer.net (2021) Prostate Cancer Statistics; www.cancer.net Last visited 3/04/2022
- American Cancer Society. Tests to Diagnose and Stage Prostate Cancer; https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/how-diagnosed.html
- Adama Ly. Traditional Medicines and Cancer Therapies in African Landscape. J Tumour Med Prev. 2018; 3(1):555601. DOI: 10.19080/JTMP.2018.03.555601.
- Maree JE, Wright SC. How would early detection be possible? An enquiry into cancer related knowledge, understanding and health seeking behaviour of urban Black women in Tshwane, South Africa. Eur J Oncol Nurs. 2010 Jul;14(3):190-6. doi: 10.1016/j.ejon.2009.10.009. Epub 2009 Nov 26. PMID: 19944646.
- Martinez Chanza, B Bernard, P Barnard, P. Barthelemy, A. Accarain, M.Paesmans, L, Desmyter, D. T,Kintde Roodenbeke, T. Gil, S, Sideris (2021) Prevalence and Clinical Impact of Tumour BRA1 and BRA 2 mutations in Patients with Localized or Metastatic Hormone Sensitive Prostate Cancer; Prostate Cancer and Prostatic Diseases pgs. 1-9 www.scholar.google.com last visited 3/04/2022
- Bello JO, Buhari T, Mohammed TO, et al. Determinants of prostate specific antigen screening test uptake in an urban community in North-Central Nigeria. Afr Health Sci. 2019;19(1):1665-1670. doi:10.4314/ahs.v19i1.42
- Moyo, S. (2017). Men's knowledge about prostate cancer: a case study of rural Mhondoro‐Ngezi, Kadoma District, Zimbabwe. European Journal of Cancer Care, 26, &NA;
- Leigh Ellis, (2018) Stopping Cancer before it Spreads; Prostate Cancer Foundation; pcf.org last visited 3/04/2022
- Eeles R, Goh C, Castro E, Bancroft E, Guy M, Al Olama AA, Easton D, Kote-Jarai Z. The genetic epidemiology of prostate cancer and its clinical implications. Nat Rev Urol. 2014 Jan;11(1):18-31. doi: 10.1038/nrurol.2013.266. Epub 2013 Dec 3. PMID: 24296704.
- Huang, C.-Y.et al. Prostate Cancer with Bone Metastases: A Clinical Profile. Mid-Taiwan Journal of Medicine, 18 July 2015. pp. 82-89.
- Rusthoven CG, Jones BL, Flaig TW, Crawford ED, Koshy M, Sher DJ, Mahmood U, Chen RC, Chapin BF, Kavanagh BD, Pugh TJ. Improved Survival With Prostate Radiation in Addition to Androgen Deprivation Therapy for Men With Newly Diagnosed Metastatic Prostate Cancer. J Clin Oncol. 2016 Aug 20;34(24):2835-42. doi: 10.1200/JCO.2016.67.4788. Epub 2016 Jun 20. PMID: 27325855.
- Faiz M. Khan, and John P. Gibbons, (2014), Khan’s the Physics of Radiation Therapy, Lippincott, Williams and Wilkins, USA.
- Kluth LA, Shariat SF, Kratzik C, Tagawa S, Sonpavde G, Rieken M, Scherr DS, Pummer K. The hypothalamic-pituitary-gonadal axis and prostate cancer: implications for androgen deprivation therapy. World J Urol. 2014 Jun;32(3):669-76. doi: 10.1007/s00345-013-1157-5. Epub 2013 Sep 3. PMID: 23999854.
- Cassell A, Yunusa B, Jalloh M, Ndoye M, Mbodji MM, Diallo A, Kouka SC, Labou I, Niang L, Gueye SM. Management of Advanced and Metastatic Prostate Cancer: A Need for a Sub-Saharan Guideline. J Oncol. 2019 Dec 5;2019:1785428. doi: 10.1155/2019/1785428. PMID: 31885569; PMCID: PMC6915139.
- Macherey S, Monsef I, Jahn F, Jordan K, Yuen KK, Heidenreich A, Skoetz N. Bisphosphonates for advanced prostate cancer. Cochrane Database Syst Rev. 2017 Dec 26;12(12):CD006250. doi: 10.1002/14651858.CD006250.pub2. PMID: 29278410; PMCID: PMC6486306.
- Sweeney CJ, Chen YH, Carducci M, Liu G, Jarrard DF, Eisenberger M, Wong YN, Hahn N, Kohli M, Cooney MM, Dreicer R, Vogelzang NJ, Picus J, Shevrin D, Hussain M, Garcia JA, DiPaola RS. Chemohormonal Therapy in Metastatic Hormone-Sensitive Prostate Cancer. N Engl J Med. 2015 Aug 20;373(8):737-46. doi: 10.1056/NEJMoa1503747. Epub 2015 Aug 5. PMID: 26244877; PMCID: PMC4562797.
- James ND, Sydes MR, Clarke NW, Mason MD, Dearnaley DP, Spears MR, Ritchie AW, Parker CC, Russell JM, Attard G, et al.; STAMPEDE investigators. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet. 2016 Mar 19;387(10024):1163-77. doi: 10.1016/S0140-6736(15)01037-5. Epub 2015 Dec 21. PMID: 26719232; PMCID: PMC4800035.
Medical Journal of Zambia, Vol 49, 3
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.