Ultrasound Imaging of a Bicornuate Uterus with a Pregnancy and an Intrauterine contraceptive device in different Horns: A Case Report from Zimbabwe
Lavin Mutandiro
School of Allied Health Science, Harare Institute of Technology
Damian Murambasvina
Carestream Ultrasound Centre, Harare
Bornface Chinene
School of Allied Health Science, Harare Institute of Technology
DOI: https://doi.org/10.55320/mjz.49.2.1001
Keywords: ultrasound imaging, intrauterine devices (IUCDs), Bicornuate uterus
ABSTRACT
A bicornuate uterus is a congenital abnormality that results from the incomplete lateral fusion of the two müllerian ducts. The WHO eligibility criteria for contraceptive use, states that the use of intrauterine devices (IUCDs) is contraindicated for women with uterine abnormalities. However, in most cases, the presence of the bicornuate uterus is not known at the time of IUCD insertion. We herein report a case of a 41-year-old woman who had a bicornuate uterus with an IUCD in situ in the left horn and a live pregnancy in the right horn. The aim of this case report is to highlight the important role ultrasound imaging can play in the diagnosis of congenital uterine abnormalities in patients using IUCDs. Furthermore, the report also discusses the ultrasound imaging techniques that a diagnostician can adopt to optimize the diagnosis.
INTRODUCTION
A bi-cornuate uterus (BU) is a congenital abnormality that results from the incomplete lateral fusion of the two Müllerian ducts. It can be classified as a Class IV Müllerian duct anomaly and leads to varying degrees of separation between the two uterine cavities or horns.[1] The WHO eligibility criteria for contraceptive use[2] , states that the use of intrauterine devices (IUCDs) is contraindicated for women with uterine abnormalities. However, in most cases, the presence of the BU is not known at the time of IUCD insertion.[3, 4] We report a case of a 41-year-old woman who had a BU with an IUCD in situ in the left horn and a live pregnancy in the right horn. The aim of this case report is to highlight the important role ultrasound imaging can play in the diagnosis of congenital uterine abnormalities in patients using IUCDs.
CASE PRESENTATION
A para 3 gravida 4, 41-year-old lady was referred for an ultrasound scan as she was complaining of lower abdominal pain and menorrhagia. A malpositioned Intrauterine Contraceptive Device (IUCD) was suspected. She had three pregnancies carried to term and normal vaginal delivery. The bladder was filled for a trans-abdominal ultrasound. Using a 3,5 MHz probe, a general sweep of the whole pelvis was performed in the longitudinal and transverse orientations. A detailed scan of the uterus was then performed in the longitudinal and transverse orientation from the fundus to the cervix. The left and right adnexae were examined in turn and the ovaries were both evaluated. Images of the uterus, uterine contents and adnexa were taken. The uterus was measured in the longitudinal and transverse orientation. The crown-rump length was measured for gestational age.
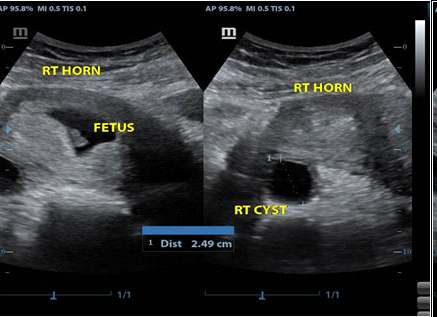
Ultrasound imaging findings were as follows:
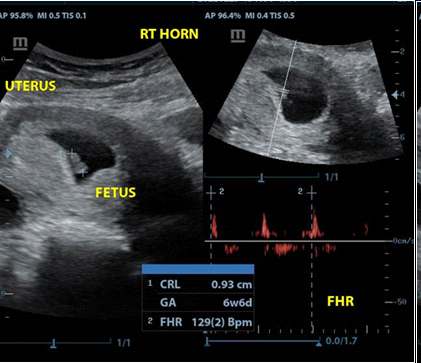
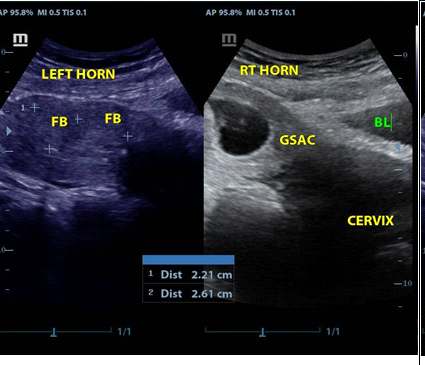
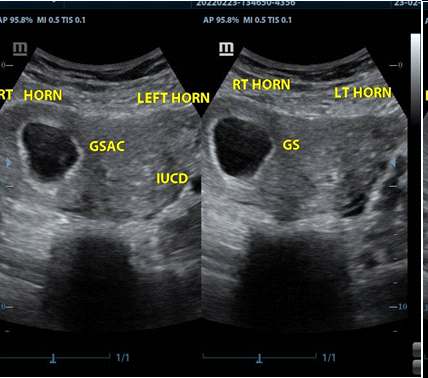
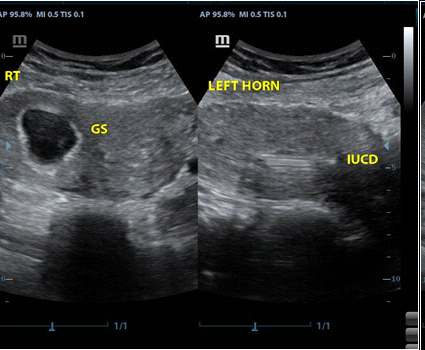
In the transverse orientation, the uterus demonstrated two distinct endometrial echoes side by side separated by myometrial tissue, in the fundus. The dip in the fundus, fundal indentation was 12 mm. The uterus was bulky with a gestation sac with a live foetus (Figure 1) with a heart rate of 129 beats per minute in the upper third of the uterus in the right horn. There were two myometrial solid masses in the left horn of the uterus (Figure 2). An IUCD was detected in the left endometrial cavity (Figures 3 and 4). Both ovaries were visualized with a well-defined anechoic mass in the left ovary which was consistent with a corpus luteal cyst (Figure 5). No free fluid was detected in the pouch of Douglas. The internal os was closed and the cervix was long and thick. Both kidneys did not have hydronephrosis, masses or cysts and were in the renal fossa. The findings were consistent with a bi-cornuate uterus with a gestation sac and foetus of 6 weeks and 6 days, in the right horn. There were two fibroids in the left anterior myometrium and an IUCD was noted in situ in the left endometrial cavity. The IUCD was removed, but the patient insisted on continuing with the pregnancy. An elective caesarean section was carried out at 38 weeks due to breech presentation of the baby. A 2.8 kilogramme baby was delivered.
DISCUSSION
The IUCD eligibility guidelines[2, 5] state that pelvic ultrasound imaging may be indicated prior to or at the same time as IUCD insertion in women with heavy menstrual bleeding (HMB) or as indicated by clinical history. This report, however, underscores the important role pelvic ultrasound imaging can play in excluding congenital uterine anomalies prior to IUCD insertion. Many women with a BU are asymptomatic and have a normal physical exam, it is usually an incidental finding through imaging for other reasons.[1, 6] 1,6 A review by Tepper et al.[3] showed that in a total of 20 cases of Müllerian duct anomalies, in 17 cases the anomaly was not known at the time of IUCD insertion. The same study noted that eleven cases reported a failure of IUCDs to prevent pregnancy and identified a total of 12 pregnancies of which 10 were diagnosed while the IUCD was still in place. The patient in our case had a normal obstetric history, i.e., three children and hence there was no suspicion of any uterine abnormalities. However, these anomalies are associated with health and reproductive problems like contraception failure as in this situation. This implies that determining the exact nature and severity of the anomaly by ultrasound imaging is critical to the management and counselling of the affected patients.[7]
The advantages of ultrasound in pelvic imaging have been shown by many studies.[8] When evaluating a woman with a possible BU, 2-D ultrasound (transabdominal or transvaginal) is often the first pelvic imaging technique employed in many settings. In order to evaluate BU, the ultrasound examination should be performed during the secretory phase of the menstrual cycle, as the echogenic endometrium is more easily recognized at this time.[9] Two-Dimensional ultrasound allows for visualization of the uterine structure, including the architecture of the myometrium and endometrium, and assessment of the ovaries. A pattern of low sensitivity and high specificity is noted with 2-D ultrasound evaluation of uterine anomalies. Although 2-D ultrasound may only identify approximately half of the uterine anomalies present, the diagnosis of an anomaly is highly likely to be correct. The addition of saline infusion to a 2-D ultrasound (saline infusion sonogram; SIS) provides better visualization of intrauterine pathology. However, even when combining 2-D ultrasound with SIS, it remains difficult to differentiate a BU from other uterine anomalies such as a septate uterus or didelphys uterus. In addition, given the possible anatomic variations of BU, a more advanced 3-D ultrasound is often needed to better characterize a BU.[1] Three-Dimensional ultrasound facilitates simultaneous visualization of both the external (serosa surface) and internal (endometrial) contours of the uterine fundus through its unique feature of providing the coronal plane of the uterus.[10]
The main disadvantage of ultrasound imaging is that it is very operator-dependent, which means it requires much skill and practice to become good at the evaluations and interpretations.[8] In the case of BU, the ultrasound diagnostician should be aware of differential diagnosis. If the imaging demonstrates two separate endometrial cavities, the differential diagnosis includes a septate uterus.1 A fundal indentation of at least 10mm is commonly used to differentiate a bi-cornuate from a septate uterus.11 The differentiation of BU from the septate uterus is critical due to the difference in their management. A septate uterus is managed via hysteroscopic resection while a BU requires a unification of the uterus. If cervical duplication is appreciated, this anomaly can be seen with bi-cornuate, septate, didelphys, and normal uteri. Lastly, a non-obstructing or obstructing longitudinal vaginal septum can occur with bi-cornuate, septate, didelphys, and normal uteri. A detailed evaluation of pelvic anatomy is therefore essential to formulate a differential diagnosis and make the proper diagnosis.[1]
The use of IUCD has been shown by some studies to be a risk factor for ectopic pregnancy.[12, 13] Women with a history of IUCD use have a 16 times more risk of ectopic pregnancy compared to women with no IUCD.[14] It is imperative that the diagnostician does not misdiagnose the pregnancy in the other horn of a BU as an ectopic pregnancy when one sees an IUCD in situ, in the other horn. Furthermore, it is important to do a thorough check of the adnexa to exclude a heterotopic pregnancy. Heterotopic pregnancy is a situation in which both an extra-uterine (ectopic pregnancy) and an intrauterine pregnancy occur simultaneously. In addition, the association of Müllerian duct and renal tract anomalies has long been recognized by many studies.[15] When uterine anomalies are detected, the ultrasound examination should be extended to the kidneys because of the frequent association with renal anomalies which are reported in up to 31% of cases.[9] Our case had a normal urinary system.
There are other imaging modalities that can be used to diagnose BU. Hysterosalpingography (HSG) demonstrates the opacification of two symmetric fusiform uterine cavities (horns) and fallopian tubes. Historically, an inter-cornual angle of greater than 105° was used for diagnosis. However, imaging overlap with a septate uterus makes differentiation impossible at HSG examination.[16] Magnetic Resonance Imaging (MRI) is typically reserved for complex or indeterminate cases because of its high-cost and low-accessibility. MRI is the imaging standard of reference because it is non-invasive, does not involve ionizing radiation, has multiplanar capability, allows excellent soft-tissue characterization, and permits a greater field of interrogation than does US. The use of MRI for the evaluation of Müllerian duct anomalies reduces the number of invasive procedures and related costs by guiding management decisions.[17]
The decision to manage a patient with the BU depends on the presentation of the patient. Firstly, if a woman presents for a routine evaluation during her pregnancy and gets diagnosed with a BU, then aggressive prenatal monitoring is indicated to prevent obstetric complications. Secondly, a patient can present with a history of recurrent abortions or preterm labour in preceding pregnancies. The latter presentation is an indication for the surgical unification of the uterus, Strassman metroplasty.[1] The procedure is carried out in four stages. The procedure initiates by making a transverse incision over the fundus of the uterus, staying away from utero-tubal junctions to avoid injury. Subsequently, the uterine cavity is opened, and the septum is removed after splitting the partition. Thus, the procedure transforms the double cavity into a single cavity. Ultimately the cavity is closed by vertical suturing to prevent endometrial adhesions. The laparoscopic approach is preferred to the abdominal metroplasty. The laparoscopic approach provides leverage in terms of less bleeding and decreased rate of infections. It also reports significantly reduced postoperative adhesion formation, which can be credited to a decrease in tissue handling and drying of tissues.[16] Prophylactic antibiotics are continued postoperatively and the recommended hospital stay is 2-3 days. The patient must use a barrier method of contraception for 3 months, after which conception can be attempted.
CONCLUSION
This case highlights the importance of ultrasound imaging prior to IUCD insertion. Furthermore, in the case of Müllerian duct anomalies, the diagnostician should examine the urinary and reproductive system to exclude associated anomalies. Lastly, IUCD is a risk factor for ectopic pregnancy, hence the need to fully examine both adnexal regions.
REFERENCES
- Pfeifer SM. Congenital Müllerian Anomalies: Diagnosis and Management. New York: Springer; 2016.
- Medical Eligibility Criteria for Contraceptive Use: A WHO Family Planning Cornerstone. 4th ed. Geneva: World Health Organization; 2010. PMID: 23741782.
- Tepper NK, Zapata LB, Jamieson DJ, Curtis KM. Use of intrauterine devices in women with uterine anatomic abnormalities. International Journal of Gynecology and Obstetrics. 2010;109:52–4.
- Sanyal R, Banerjee S, Taori K. Pregnancy and IUD in Different Horns of the Uterus. J Clin Ultrasound. 2007;35(1):40–1.
- FSRH Clinical Guideline: Intrauterine Contraception (April 2015, amended September 2019)
- Mergo P, Maclean J, Serguei MedvedevWang H, Gerasymchuk G. Sonography of a bicorunate uterus : Pregnancy in one and an IUD in the other horn of a bicornuate uterus. Eurorad. 2019.
- Cassar OA, Dalli SM. Pregnancy in a bicornuate uterus with contraceptive coil in situ - a case report. Obstet Gynecol Int J. 2017;7(3):249‒252. DOI: 10.15406/ogij.2017.07.00247
- Bhide, A., Datar, S., & Stebbins, K. (2021). Development of Ultrasound Scanning: Case Histories of Significant Medical Advances. Harvard Business School Accounting & Management Unit Working Paper, (20).
- Bates, Jane. Manual of diagnostic ultrasound. Ultrasound in Medicine and Biology, Volume 22, Issue 6, 767
- Jayaprakasan K, Ojha K. Diagnosis of Congenital Uterine Abnormalities: Practical Considerations. J Clin Med. 2022 Feb 25;11(5):1251. doi: 10.3390/jcm11051251. PMID: 35268343; PMCID: PMC8911320.
- Stadtmauer, Laurel and Ilan Tur-Kaspa. “Ultrasound Imaging in Reproductive Medicine.” Springer International Publishing (2019).
- Li C, Zhao WH, Meng CX, Ping H, Qin GJ, Cao SJ, et al. Contraceptive use and the risk of ectopic pregnancy: A multi-center case-control study. PLoS ONE. 2014;9(12):1–17.
- Heinemann K, Reed S, Moehner S, Do Minh T. Comparative contraceptive effectiveness of levonorgestrel-releasing and copper intrauterine devices: The European Active Surveillance Study for Intrauterine Devices. Contraception. 2015;91(4):280–3. Available from: http://dx.doi.org/10.1016/j.contraception.2015.01.011
- Koirala S, Balla P, Pokhrel A, Koirala S, Pant S, Paudyal S. A rare case of ovarian ectopic pregnancy with IUD in situ: A case report from Nepal. Clinical Case Reports. 2020;8(12):3240–3.
- K. Heinonen P. Renal tract malformations associated with Müllerian duct anomalies. Clinical Obstetrics, Gynecology and Reproductive Medicine. 2018;4(1):1–5.
- Kaur P, Panneerselvam D. Bicornuate Uterus. StatPearls. 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560859/
- Behr SC, Courtier JL, Qayyum A. Imaging of Müllerian Duct Anomalies. Radiographics. 2012;(October Special Issue):E233–50. Available from: 10.1148/rg.326125515
Medical Journal of Zambia, Vol 49, 2
The Medical Journal of Zambia, ISSN 0047-651X, is published by the Zambia Medical Association.
© This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.